User login
American Society for Dermatologic Surgery (ASDS): Annual Meeting
Keep canthopexy, canthoplasty in your sights for periorbital aging
CHICAGO – Canthopexy and canthoplasty are simple, minimally invasive procedures that are often overlooked when treating periorbital aging, Dr. Cameron D. Chesnut said at the annual meeting of the American Society for Dermatologic Surgery.
“In a simple procedure you can do in the office in literally 5 or 10 minutes under local anesthesia, you can restore the integrity of the lower lid, which in addition gives some improvement in the upper lids by lifting the globe back up,” he said.
Canthopexy and canthoplasty are very commonly performed with blepharoplasty, but can be useful on their own or in combination with fillers in mild cases of retinacular aging or lower-lid ectropion where you don’t need or want a true, full-blown blepharoplasty.
There is a labyrinth of connective tissues attached to Whitnall’s tubercle and as patients age, there is laxity of the septum, retinaculum, and orbicularis; rounding of the lateral canthal angle; and a negative intercanthal tilt that develops as the lateral canthus drops in relation to the medial canthus, said Dr. Chesnut, who is in private practice in Spokane, Wash.
In the canthopexy, the lateral canthal tendon is folded over and stabilized with a stitch, but not dispensed with. “Yes, this is surgical, but this is literally a stab incision with an 11 blade to access this,” he noted.
The key to a successful canthopexy is to release the tarsal strap, which is relatively resistant to aging laxity and tethers the lateral canthus inferiorly. “While everything else around it becomes lax, it tends to stay pretty strong and pulls down the whole lateral canthal complex,” he observed.
The canthoplasty creates more tension on the lower lid, but is more invasive. The lateral canthal tendon is cut, releasing the retinaculum. The eyelid opening is then shortened and the tendon reconstructed and reattached to the bone.
Particular attention should be paid in both procedures to globe position, particularly in patients with a negative vector in which the globe protrudes beyond their malar eminence and lower eyelid, Dr. Chesnut pointed out.
“You need to be careful with these patients because if you tighten the lower lid too much, the lower lid margin will take the path of least resistance and descend down the globe instead of up,” he said. “These are the patients that may need volume or face lifting to increase that malar support.” Complications can include overtightening, but this is nearly impossible to do with a canthopexy and usually relaxes with a canthoplasty, Dr. Chesnut said in an interview. “Avoiding it all boils down to proper preoperative planning of the amount of tightening needed.”
Likewise, proper planning can avoid undercorrection.
“This can occasionally be from failure of the reconstructed or plicated lateral canthal tendon, but this is a very robust structure, and when properly fixated to the periosteum of Whitnall’s tubercle, failure is unlikely,” Dr. Chesnut explained. “The tendon will continue to age normally, so a canthopexy patient may require or want more tightening with a canthoplasty years down the road.”
Lower-lid laxity should be assessed in all patients prior to either procedure and can be determined by performing the distraction test, in which the eyelid is grasped and pulled anteriorly. If the eyelid can be distracted by more than 6 mm to 8 mm, then laxity is present. The snapback test, where the lower lid is pulled toward the inferior orbital rim and then released, can also be used to identify poor lid tone.
Dr. Chesnut reported having no conflicts of interest.
CHICAGO – Canthopexy and canthoplasty are simple, minimally invasive procedures that are often overlooked when treating periorbital aging, Dr. Cameron D. Chesnut said at the annual meeting of the American Society for Dermatologic Surgery.
“In a simple procedure you can do in the office in literally 5 or 10 minutes under local anesthesia, you can restore the integrity of the lower lid, which in addition gives some improvement in the upper lids by lifting the globe back up,” he said.
Canthopexy and canthoplasty are very commonly performed with blepharoplasty, but can be useful on their own or in combination with fillers in mild cases of retinacular aging or lower-lid ectropion where you don’t need or want a true, full-blown blepharoplasty.
There is a labyrinth of connective tissues attached to Whitnall’s tubercle and as patients age, there is laxity of the septum, retinaculum, and orbicularis; rounding of the lateral canthal angle; and a negative intercanthal tilt that develops as the lateral canthus drops in relation to the medial canthus, said Dr. Chesnut, who is in private practice in Spokane, Wash.
In the canthopexy, the lateral canthal tendon is folded over and stabilized with a stitch, but not dispensed with. “Yes, this is surgical, but this is literally a stab incision with an 11 blade to access this,” he noted.
The key to a successful canthopexy is to release the tarsal strap, which is relatively resistant to aging laxity and tethers the lateral canthus inferiorly. “While everything else around it becomes lax, it tends to stay pretty strong and pulls down the whole lateral canthal complex,” he observed.
The canthoplasty creates more tension on the lower lid, but is more invasive. The lateral canthal tendon is cut, releasing the retinaculum. The eyelid opening is then shortened and the tendon reconstructed and reattached to the bone.
Particular attention should be paid in both procedures to globe position, particularly in patients with a negative vector in which the globe protrudes beyond their malar eminence and lower eyelid, Dr. Chesnut pointed out.
“You need to be careful with these patients because if you tighten the lower lid too much, the lower lid margin will take the path of least resistance and descend down the globe instead of up,” he said. “These are the patients that may need volume or face lifting to increase that malar support.” Complications can include overtightening, but this is nearly impossible to do with a canthopexy and usually relaxes with a canthoplasty, Dr. Chesnut said in an interview. “Avoiding it all boils down to proper preoperative planning of the amount of tightening needed.”
Likewise, proper planning can avoid undercorrection.
“This can occasionally be from failure of the reconstructed or plicated lateral canthal tendon, but this is a very robust structure, and when properly fixated to the periosteum of Whitnall’s tubercle, failure is unlikely,” Dr. Chesnut explained. “The tendon will continue to age normally, so a canthopexy patient may require or want more tightening with a canthoplasty years down the road.”
Lower-lid laxity should be assessed in all patients prior to either procedure and can be determined by performing the distraction test, in which the eyelid is grasped and pulled anteriorly. If the eyelid can be distracted by more than 6 mm to 8 mm, then laxity is present. The snapback test, where the lower lid is pulled toward the inferior orbital rim and then released, can also be used to identify poor lid tone.
Dr. Chesnut reported having no conflicts of interest.
CHICAGO – Canthopexy and canthoplasty are simple, minimally invasive procedures that are often overlooked when treating periorbital aging, Dr. Cameron D. Chesnut said at the annual meeting of the American Society for Dermatologic Surgery.
“In a simple procedure you can do in the office in literally 5 or 10 minutes under local anesthesia, you can restore the integrity of the lower lid, which in addition gives some improvement in the upper lids by lifting the globe back up,” he said.
Canthopexy and canthoplasty are very commonly performed with blepharoplasty, but can be useful on their own or in combination with fillers in mild cases of retinacular aging or lower-lid ectropion where you don’t need or want a true, full-blown blepharoplasty.
There is a labyrinth of connective tissues attached to Whitnall’s tubercle and as patients age, there is laxity of the septum, retinaculum, and orbicularis; rounding of the lateral canthal angle; and a negative intercanthal tilt that develops as the lateral canthus drops in relation to the medial canthus, said Dr. Chesnut, who is in private practice in Spokane, Wash.
In the canthopexy, the lateral canthal tendon is folded over and stabilized with a stitch, but not dispensed with. “Yes, this is surgical, but this is literally a stab incision with an 11 blade to access this,” he noted.
The key to a successful canthopexy is to release the tarsal strap, which is relatively resistant to aging laxity and tethers the lateral canthus inferiorly. “While everything else around it becomes lax, it tends to stay pretty strong and pulls down the whole lateral canthal complex,” he observed.
The canthoplasty creates more tension on the lower lid, but is more invasive. The lateral canthal tendon is cut, releasing the retinaculum. The eyelid opening is then shortened and the tendon reconstructed and reattached to the bone.
Particular attention should be paid in both procedures to globe position, particularly in patients with a negative vector in which the globe protrudes beyond their malar eminence and lower eyelid, Dr. Chesnut pointed out.
“You need to be careful with these patients because if you tighten the lower lid too much, the lower lid margin will take the path of least resistance and descend down the globe instead of up,” he said. “These are the patients that may need volume or face lifting to increase that malar support.” Complications can include overtightening, but this is nearly impossible to do with a canthopexy and usually relaxes with a canthoplasty, Dr. Chesnut said in an interview. “Avoiding it all boils down to proper preoperative planning of the amount of tightening needed.”
Likewise, proper planning can avoid undercorrection.
“This can occasionally be from failure of the reconstructed or plicated lateral canthal tendon, but this is a very robust structure, and when properly fixated to the periosteum of Whitnall’s tubercle, failure is unlikely,” Dr. Chesnut explained. “The tendon will continue to age normally, so a canthopexy patient may require or want more tightening with a canthoplasty years down the road.”
Lower-lid laxity should be assessed in all patients prior to either procedure and can be determined by performing the distraction test, in which the eyelid is grasped and pulled anteriorly. If the eyelid can be distracted by more than 6 mm to 8 mm, then laxity is present. The snapback test, where the lower lid is pulled toward the inferior orbital rim and then released, can also be used to identify poor lid tone.
Dr. Chesnut reported having no conflicts of interest.
EXPERT ANALYSIS FROM THE ASDS ANNUAL MEETING
Gel patch speeds laser tattoo removal
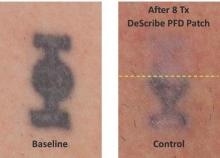
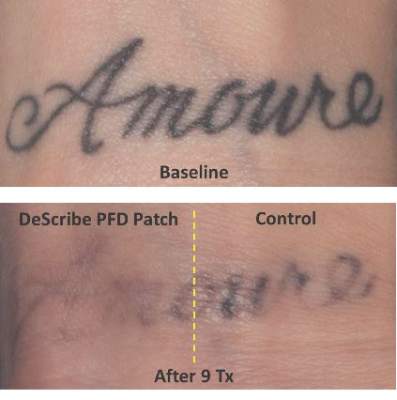
CHICAGO – Treating tattoos through a transparent perfluorodecalin-infused gel patch may cut down on the number of laser treatments needed to remove unwanted tattoos, results of a small pilot study suggest.
In 11 of 17 patients, tattoos treated through the perfluorodecalin (PFD) patch showed more rapid clearance of their tattoos compared with conventional treatment with the same 755-nm Q-switched alexandrite laser, Dr. Brian Biesman said at the annual meeting of the American Society for Dermatologic Surgery.
There were, however, a wide variety of responses, likely reflecting the heterogeneity of the tattoos themselves, ranging from no difference after many treatment sessions to more than 80% clearance after only two sessions, said Dr. Biesman, who is in private practice in Nashville, Tenn. Perfluorodecalin, a fluorocarbon that enhances oxygen delivery, reduces the epidermal whitening that typically limits Q-switched laser tattoo removal to a single pass. Use of the PFD patch in a prior study resolved whitening within an average of 5 seconds, allowing for three to four laser passes in less than 5 minutes (Lasers Surg Med. 2013 Feb;45[2]:76-80).
The DeScribe Transparent PFD Patch (ON Light Sciences) was approved in the United States in April 2015 for use as an accessory to laser tattoo removal procedures using a 755-nm Q-switched alexandrite laser in Fitzpatrick skin type I-III patients.
Anecdotal evidence presented by Dr. Biesman from his own patients suggests that the PFD patch may also speed tattoo clearance when used with different pulse durations and wavelengths, including 5-nanosecond (1,064 nm, 532 nm, and 650 nm) and picosecond (755 nm, 532 nm, and 1,064 nm) lasers.
“It does appear that this patch is efficacious with other Q-switched lasers, both nanosecond and picosecond,” he said, adding that this work is preliminary and under careful study.
The pilot study involved 17 patients with Fitzpatrick skin types I-III and black or blue tattoos treated with a conventional Q-switched alexandrite laser at the maximum tolerable fluence through the PFD patch on one side for three to four passes and with one pass through the air on the other side.
The patch allowed a factor of 1.5-times to 1.8-times higher fluence than control, Dr. Biesman said. In no case did the control side tattoo fade faster than the PFD patch side.
The study was sufficiently powered to qualitatively answer the question of whether the patch could enhance the clearance rate relative to control, but the quantitative rate could not be measured because of the small patient numbers, he noted.
Predictive factors were not identifiable because of the large number of variables, such as tattoo ink, tattoo location, and patient age.
There were no unanticipated adverse events with up to a year of follow-up. Three patients reported three areas of skin hypopigmentation that fully resolved, Dr. Biesman said.
The majority of patients in the pilot study, as well as in a 30-patient pivotal study, reported higher satisfaction with the patch treatment. This seemed to be from a combination of factors, including less discomfort during and after treatment, easier posttreatment recovery, and faster resolution, he said in an interview.
“In our practice, the patch has become the standard of care,” he added. “My nursing staff is highly protective of our patients and will not permit treatment of our patients without the patch. Based on our patients’ objective and subjective experience, I concur.”
Further studies to formally evaluate the performance of the patch in the treatment of benign pigmented lesions and with other Q-switched lasers, using a variety of wavelengths and pulse durations, are currently under consideration.
CHICAGO – Treating tattoos through a transparent perfluorodecalin-infused gel patch may cut down on the number of laser treatments needed to remove unwanted tattoos, results of a small pilot study suggest.
In 11 of 17 patients, tattoos treated through the perfluorodecalin (PFD) patch showed more rapid clearance of their tattoos compared with conventional treatment with the same 755-nm Q-switched alexandrite laser, Dr. Brian Biesman said at the annual meeting of the American Society for Dermatologic Surgery.
There were, however, a wide variety of responses, likely reflecting the heterogeneity of the tattoos themselves, ranging from no difference after many treatment sessions to more than 80% clearance after only two sessions, said Dr. Biesman, who is in private practice in Nashville, Tenn. Perfluorodecalin, a fluorocarbon that enhances oxygen delivery, reduces the epidermal whitening that typically limits Q-switched laser tattoo removal to a single pass. Use of the PFD patch in a prior study resolved whitening within an average of 5 seconds, allowing for three to four laser passes in less than 5 minutes (Lasers Surg Med. 2013 Feb;45[2]:76-80).
The DeScribe Transparent PFD Patch (ON Light Sciences) was approved in the United States in April 2015 for use as an accessory to laser tattoo removal procedures using a 755-nm Q-switched alexandrite laser in Fitzpatrick skin type I-III patients.
Anecdotal evidence presented by Dr. Biesman from his own patients suggests that the PFD patch may also speed tattoo clearance when used with different pulse durations and wavelengths, including 5-nanosecond (1,064 nm, 532 nm, and 650 nm) and picosecond (755 nm, 532 nm, and 1,064 nm) lasers.
“It does appear that this patch is efficacious with other Q-switched lasers, both nanosecond and picosecond,” he said, adding that this work is preliminary and under careful study.
The pilot study involved 17 patients with Fitzpatrick skin types I-III and black or blue tattoos treated with a conventional Q-switched alexandrite laser at the maximum tolerable fluence through the PFD patch on one side for three to four passes and with one pass through the air on the other side.
The patch allowed a factor of 1.5-times to 1.8-times higher fluence than control, Dr. Biesman said. In no case did the control side tattoo fade faster than the PFD patch side.
The study was sufficiently powered to qualitatively answer the question of whether the patch could enhance the clearance rate relative to control, but the quantitative rate could not be measured because of the small patient numbers, he noted.
Predictive factors were not identifiable because of the large number of variables, such as tattoo ink, tattoo location, and patient age.
There were no unanticipated adverse events with up to a year of follow-up. Three patients reported three areas of skin hypopigmentation that fully resolved, Dr. Biesman said.
The majority of patients in the pilot study, as well as in a 30-patient pivotal study, reported higher satisfaction with the patch treatment. This seemed to be from a combination of factors, including less discomfort during and after treatment, easier posttreatment recovery, and faster resolution, he said in an interview.
“In our practice, the patch has become the standard of care,” he added. “My nursing staff is highly protective of our patients and will not permit treatment of our patients without the patch. Based on our patients’ objective and subjective experience, I concur.”
Further studies to formally evaluate the performance of the patch in the treatment of benign pigmented lesions and with other Q-switched lasers, using a variety of wavelengths and pulse durations, are currently under consideration.
CHICAGO – Treating tattoos through a transparent perfluorodecalin-infused gel patch may cut down on the number of laser treatments needed to remove unwanted tattoos, results of a small pilot study suggest.
In 11 of 17 patients, tattoos treated through the perfluorodecalin (PFD) patch showed more rapid clearance of their tattoos compared with conventional treatment with the same 755-nm Q-switched alexandrite laser, Dr. Brian Biesman said at the annual meeting of the American Society for Dermatologic Surgery.
There were, however, a wide variety of responses, likely reflecting the heterogeneity of the tattoos themselves, ranging from no difference after many treatment sessions to more than 80% clearance after only two sessions, said Dr. Biesman, who is in private practice in Nashville, Tenn. Perfluorodecalin, a fluorocarbon that enhances oxygen delivery, reduces the epidermal whitening that typically limits Q-switched laser tattoo removal to a single pass. Use of the PFD patch in a prior study resolved whitening within an average of 5 seconds, allowing for three to four laser passes in less than 5 minutes (Lasers Surg Med. 2013 Feb;45[2]:76-80).
The DeScribe Transparent PFD Patch (ON Light Sciences) was approved in the United States in April 2015 for use as an accessory to laser tattoo removal procedures using a 755-nm Q-switched alexandrite laser in Fitzpatrick skin type I-III patients.
Anecdotal evidence presented by Dr. Biesman from his own patients suggests that the PFD patch may also speed tattoo clearance when used with different pulse durations and wavelengths, including 5-nanosecond (1,064 nm, 532 nm, and 650 nm) and picosecond (755 nm, 532 nm, and 1,064 nm) lasers.
“It does appear that this patch is efficacious with other Q-switched lasers, both nanosecond and picosecond,” he said, adding that this work is preliminary and under careful study.
The pilot study involved 17 patients with Fitzpatrick skin types I-III and black or blue tattoos treated with a conventional Q-switched alexandrite laser at the maximum tolerable fluence through the PFD patch on one side for three to four passes and with one pass through the air on the other side.
The patch allowed a factor of 1.5-times to 1.8-times higher fluence than control, Dr. Biesman said. In no case did the control side tattoo fade faster than the PFD patch side.
The study was sufficiently powered to qualitatively answer the question of whether the patch could enhance the clearance rate relative to control, but the quantitative rate could not be measured because of the small patient numbers, he noted.
Predictive factors were not identifiable because of the large number of variables, such as tattoo ink, tattoo location, and patient age.
There were no unanticipated adverse events with up to a year of follow-up. Three patients reported three areas of skin hypopigmentation that fully resolved, Dr. Biesman said.
The majority of patients in the pilot study, as well as in a 30-patient pivotal study, reported higher satisfaction with the patch treatment. This seemed to be from a combination of factors, including less discomfort during and after treatment, easier posttreatment recovery, and faster resolution, he said in an interview.
“In our practice, the patch has become the standard of care,” he added. “My nursing staff is highly protective of our patients and will not permit treatment of our patients without the patch. Based on our patients’ objective and subjective experience, I concur.”
Further studies to formally evaluate the performance of the patch in the treatment of benign pigmented lesions and with other Q-switched lasers, using a variety of wavelengths and pulse durations, are currently under consideration.
AT THE ASDS ANNUAL MEETING
Key clinical point: A transparent perfluorodecalin-infused patch allows for more rapid, multipass laser tattoo removal.
Major finding: Tattoo clearance was accelerated with the PFD patch in 11 of 17 patients.
Data source: A split-skin pilot study comparing results of laser treatments with and without the patch in 17 patients with black or blue tattoos.
Disclosures: Dr. Biesman reported being a shareholder of ON Light Sciences, the study sponsor and manufacturer of the PFD patch.
Dermatologists’ management of melanoma varies
CHICAGO – Significant variance exists in management of primary cutaneous melanoma, according to a national survey of 510 dermatologists.
Most dermatologists (36%) preferred a shave biopsy for lesions suspected of being melanoma, despite guidelines from the American Academy of Dermatology (AAD) and National Comprehensive Cancer Network (NCCN) guidelines that recommend narrow excision biopsy.
In all, 31% of dermatologists used a narrow local excision (less than 5 mm margin), 13% saucerization/scoop shave biopsy, 11%, punch biopsy, 3% wide local excision, and 7% other.
“The guidelines and academy are all very clear that one of the goals of the biopsy is to obtain tumor depth, so we were surprised that a significant number of providers use shave biopsy or other methods that may leave a risk of not getting the correct depth,” study co-author Dr. Aaron S. Farberg, a melanoma clinical research fellow at the National Society for Cutaneous Medicine in New York City, said in an interview.
Notably, dermatologists in academic and dermatology-based group practices were significantly less likely than those in multispecialty or solo practice to use narrow excision (23% vs. 42%; P < .001).
Although treatment for melanoma evolves continuously, the authors observed that dermatologists remain at the forefront of melanoma management and play a critical role in patient decision making.
“This study suggests that a knowledge gap may exist representing an educational opportunity to more effectively disseminate and implement recommended approaches,” Dr. Farberg and Dr. Darrell Rigel, of New York University School of Medicine, reported in a poster presentation at the annual meeting of the American Society for Dermatologic Surgery.
The survey also revealed that dermatologists are going beyond suggested surgical margins when excising melanoma.
For malignant melanoma in situ (MMIS), 62% used a 5 mm or less margin, 36% a 6 mm to 10 mm margin, and 2% a 1.1 cm to 1.9 cm margin. For these lesions, the AAD recommends a 0.5 cm-1 cm (5 mm-10 mm) margin and the NCCN a 0.5 cm margin, Drs. Farber and Rigel reported.
Academic dermatologists were significantly more likely than all other practice types to refer patients with MMIS out for excision (18% vs. 10%; P < .05).
For invasive melanoma less than 1 mm in depth, both the AAD and NCCN recommend a 1 cm margin (10 mm). In all, 61% of dermatologists reported using 6 mm to 10 mm margins, with 34% opting for 1.1 cm to 1.9 cm margins, 3% at least 2 cm margins, and 2% no more than 5 mm margins.
No significant difference was found across provider types for treatment of melanomas less than 1 mm in depth.
For invasive melanoma greater than 1 mm in depth, 54% of respondents used 1.1 cm to 1.9 cm margins, with most (67%) referring the patient to another provider. Both national guidelines recommend 1 cm to 2 cm margins for melanomas 1 mm to 2 mm in depth and 2 cm margins for melanoma greater than 2 mm in depth.
Academic dermatologists were significantly more likely than other dermatologists to treat these lesions rather than to refer the patient out (51% vs. 30%; P < .001).
“This is exciting new data that suggests that there still is a variance in early melanoma management,” Dr. Rigel, past president of AAD and ASDS, said in an interview. “The data suggest more studies need to be done to better access why this is occurring.”
Dr. Hensin Tsao, who served on the 2011 AAD guideline working group and is co-chairing the AAD’s pending guideline update, said in an interview that, “Dr. Rigel is well respected in the field and the project will undoubtedly be submitted for publication and subject to further review. It is worthwhile to wait on the final published results and conclusions.”
He agreed, however, with the authors’ suggestion that there is significant variation in practice. Regarding the finding that 36% of respondents use a shave biopsy for suspicious lesions, the AAD guidelines recommend that the entire lesion be removed with a 1 mm to 3 mm margin, which can be accomplished by an elliptical or punch excision with sutures or shave removal to a depth below the anticipated plane of the lesion, Dr. Tsao, of Massachusetts General Hospital in Boston, said.
“It is quite possible that some of the respondents to the questionnaire interpreted ‘shave biopsy’ as a full shave disk excision,” he said. “That said, intentional and routine partial sampling of suspected melanomas would be at odds with the guidelines.”
It is not inappropriate to remove a suspicious lesion, if small enough, with a punch biopsy, Dr. Tsao said, adding, “Perhaps again, the respondents failed to distinguish between partial punch biopsy and punch excision.”
On occasion, the AAD guidelines also make accommodations for an incisional biopsy “of the clinically or dermatoscopically most atypical portion of the lesion.” In this situation, a smaller incisional punch biopsy may be performed of the highly suspicious area.
“There are certainly areas that the investigators have identified which could represent potential knowledge gaps,” Dr. Tsao said. “For instance, 14% of the respondents used a 0.6 cm to 1.0 cm (6 mm-10 mm) margin for melanoma greater than 1 mm.”
Dermatologists’ surveillance of patients in the survey was somewhat less divergent. The most recommended follow-up interval for patients diagnosed within the last 5 years, was 6 months (49%), followed by a 3-month interval (25%), and other (24%). Follow-up was extended to yearly by 63% of dermatologists for patients diagnosed more than five years earlier, Dr. Farberg and Dr. Rigel reported.
Both the AAD and NCCN recommend follow-up every 3 to 12 months for those diagnosed with melanoma within the previous 5 years, while for those diagnosed more than 5 years prior, the AAD recommends follow-up every 3 to 12 months and the NCCN every 12 months.
“Adherence to evidence-based guidelines should lead to improved patient outcomes and quality of care. However, newer studies and emerging data may also justify deviations from existing guidelines, suggesting review of those guidelines may be indicated,” Dr. Farberg and Dr. Rigel concluded.
For example, a prospective series examining surgical margins in 1,072 patients with 1,120 malignant melanoma in situs showed that only 86% were successfully excised with a 6-mm margin, significantly less than the 98.9% clearance achieved with a 9-mm margin, Dr. Farberg told this publication.
That said, a 9-mm margin may not be appropriate for all lesions, such as those on the face, he observed.
The investigators said they hope the survey results will spur on revision of the guidelines, last updated in 2011.
Limitations of the survey include a lack of information on clinical factors such as patient history or anatomic site, the survey may have led to generalized answers, and access to care and reimbursement also may have impacted management, the authors noted.
The response rate to the survey was also low at 8%, with 6,177 practicing U.S. dermatologists surveyed. The demographics of the respondents, however, strongly reflected the full AAD membership, Dr. Farberg said. No significant geographical differences were observed.
CHICAGO – Significant variance exists in management of primary cutaneous melanoma, according to a national survey of 510 dermatologists.
Most dermatologists (36%) preferred a shave biopsy for lesions suspected of being melanoma, despite guidelines from the American Academy of Dermatology (AAD) and National Comprehensive Cancer Network (NCCN) guidelines that recommend narrow excision biopsy.
In all, 31% of dermatologists used a narrow local excision (less than 5 mm margin), 13% saucerization/scoop shave biopsy, 11%, punch biopsy, 3% wide local excision, and 7% other.
“The guidelines and academy are all very clear that one of the goals of the biopsy is to obtain tumor depth, so we were surprised that a significant number of providers use shave biopsy or other methods that may leave a risk of not getting the correct depth,” study co-author Dr. Aaron S. Farberg, a melanoma clinical research fellow at the National Society for Cutaneous Medicine in New York City, said in an interview.
Notably, dermatologists in academic and dermatology-based group practices were significantly less likely than those in multispecialty or solo practice to use narrow excision (23% vs. 42%; P < .001).
Although treatment for melanoma evolves continuously, the authors observed that dermatologists remain at the forefront of melanoma management and play a critical role in patient decision making.
“This study suggests that a knowledge gap may exist representing an educational opportunity to more effectively disseminate and implement recommended approaches,” Dr. Farberg and Dr. Darrell Rigel, of New York University School of Medicine, reported in a poster presentation at the annual meeting of the American Society for Dermatologic Surgery.
The survey also revealed that dermatologists are going beyond suggested surgical margins when excising melanoma.
For malignant melanoma in situ (MMIS), 62% used a 5 mm or less margin, 36% a 6 mm to 10 mm margin, and 2% a 1.1 cm to 1.9 cm margin. For these lesions, the AAD recommends a 0.5 cm-1 cm (5 mm-10 mm) margin and the NCCN a 0.5 cm margin, Drs. Farber and Rigel reported.
Academic dermatologists were significantly more likely than all other practice types to refer patients with MMIS out for excision (18% vs. 10%; P < .05).
For invasive melanoma less than 1 mm in depth, both the AAD and NCCN recommend a 1 cm margin (10 mm). In all, 61% of dermatologists reported using 6 mm to 10 mm margins, with 34% opting for 1.1 cm to 1.9 cm margins, 3% at least 2 cm margins, and 2% no more than 5 mm margins.
No significant difference was found across provider types for treatment of melanomas less than 1 mm in depth.
For invasive melanoma greater than 1 mm in depth, 54% of respondents used 1.1 cm to 1.9 cm margins, with most (67%) referring the patient to another provider. Both national guidelines recommend 1 cm to 2 cm margins for melanomas 1 mm to 2 mm in depth and 2 cm margins for melanoma greater than 2 mm in depth.
Academic dermatologists were significantly more likely than other dermatologists to treat these lesions rather than to refer the patient out (51% vs. 30%; P < .001).
“This is exciting new data that suggests that there still is a variance in early melanoma management,” Dr. Rigel, past president of AAD and ASDS, said in an interview. “The data suggest more studies need to be done to better access why this is occurring.”
Dr. Hensin Tsao, who served on the 2011 AAD guideline working group and is co-chairing the AAD’s pending guideline update, said in an interview that, “Dr. Rigel is well respected in the field and the project will undoubtedly be submitted for publication and subject to further review. It is worthwhile to wait on the final published results and conclusions.”
He agreed, however, with the authors’ suggestion that there is significant variation in practice. Regarding the finding that 36% of respondents use a shave biopsy for suspicious lesions, the AAD guidelines recommend that the entire lesion be removed with a 1 mm to 3 mm margin, which can be accomplished by an elliptical or punch excision with sutures or shave removal to a depth below the anticipated plane of the lesion, Dr. Tsao, of Massachusetts General Hospital in Boston, said.
“It is quite possible that some of the respondents to the questionnaire interpreted ‘shave biopsy’ as a full shave disk excision,” he said. “That said, intentional and routine partial sampling of suspected melanomas would be at odds with the guidelines.”
It is not inappropriate to remove a suspicious lesion, if small enough, with a punch biopsy, Dr. Tsao said, adding, “Perhaps again, the respondents failed to distinguish between partial punch biopsy and punch excision.”
On occasion, the AAD guidelines also make accommodations for an incisional biopsy “of the clinically or dermatoscopically most atypical portion of the lesion.” In this situation, a smaller incisional punch biopsy may be performed of the highly suspicious area.
“There are certainly areas that the investigators have identified which could represent potential knowledge gaps,” Dr. Tsao said. “For instance, 14% of the respondents used a 0.6 cm to 1.0 cm (6 mm-10 mm) margin for melanoma greater than 1 mm.”
Dermatologists’ surveillance of patients in the survey was somewhat less divergent. The most recommended follow-up interval for patients diagnosed within the last 5 years, was 6 months (49%), followed by a 3-month interval (25%), and other (24%). Follow-up was extended to yearly by 63% of dermatologists for patients diagnosed more than five years earlier, Dr. Farberg and Dr. Rigel reported.
Both the AAD and NCCN recommend follow-up every 3 to 12 months for those diagnosed with melanoma within the previous 5 years, while for those diagnosed more than 5 years prior, the AAD recommends follow-up every 3 to 12 months and the NCCN every 12 months.
“Adherence to evidence-based guidelines should lead to improved patient outcomes and quality of care. However, newer studies and emerging data may also justify deviations from existing guidelines, suggesting review of those guidelines may be indicated,” Dr. Farberg and Dr. Rigel concluded.
For example, a prospective series examining surgical margins in 1,072 patients with 1,120 malignant melanoma in situs showed that only 86% were successfully excised with a 6-mm margin, significantly less than the 98.9% clearance achieved with a 9-mm margin, Dr. Farberg told this publication.
That said, a 9-mm margin may not be appropriate for all lesions, such as those on the face, he observed.
The investigators said they hope the survey results will spur on revision of the guidelines, last updated in 2011.
Limitations of the survey include a lack of information on clinical factors such as patient history or anatomic site, the survey may have led to generalized answers, and access to care and reimbursement also may have impacted management, the authors noted.
The response rate to the survey was also low at 8%, with 6,177 practicing U.S. dermatologists surveyed. The demographics of the respondents, however, strongly reflected the full AAD membership, Dr. Farberg said. No significant geographical differences were observed.
CHICAGO – Significant variance exists in management of primary cutaneous melanoma, according to a national survey of 510 dermatologists.
Most dermatologists (36%) preferred a shave biopsy for lesions suspected of being melanoma, despite guidelines from the American Academy of Dermatology (AAD) and National Comprehensive Cancer Network (NCCN) guidelines that recommend narrow excision biopsy.
In all, 31% of dermatologists used a narrow local excision (less than 5 mm margin), 13% saucerization/scoop shave biopsy, 11%, punch biopsy, 3% wide local excision, and 7% other.
“The guidelines and academy are all very clear that one of the goals of the biopsy is to obtain tumor depth, so we were surprised that a significant number of providers use shave biopsy or other methods that may leave a risk of not getting the correct depth,” study co-author Dr. Aaron S. Farberg, a melanoma clinical research fellow at the National Society for Cutaneous Medicine in New York City, said in an interview.
Notably, dermatologists in academic and dermatology-based group practices were significantly less likely than those in multispecialty or solo practice to use narrow excision (23% vs. 42%; P < .001).
Although treatment for melanoma evolves continuously, the authors observed that dermatologists remain at the forefront of melanoma management and play a critical role in patient decision making.
“This study suggests that a knowledge gap may exist representing an educational opportunity to more effectively disseminate and implement recommended approaches,” Dr. Farberg and Dr. Darrell Rigel, of New York University School of Medicine, reported in a poster presentation at the annual meeting of the American Society for Dermatologic Surgery.
The survey also revealed that dermatologists are going beyond suggested surgical margins when excising melanoma.
For malignant melanoma in situ (MMIS), 62% used a 5 mm or less margin, 36% a 6 mm to 10 mm margin, and 2% a 1.1 cm to 1.9 cm margin. For these lesions, the AAD recommends a 0.5 cm-1 cm (5 mm-10 mm) margin and the NCCN a 0.5 cm margin, Drs. Farber and Rigel reported.
Academic dermatologists were significantly more likely than all other practice types to refer patients with MMIS out for excision (18% vs. 10%; P < .05).
For invasive melanoma less than 1 mm in depth, both the AAD and NCCN recommend a 1 cm margin (10 mm). In all, 61% of dermatologists reported using 6 mm to 10 mm margins, with 34% opting for 1.1 cm to 1.9 cm margins, 3% at least 2 cm margins, and 2% no more than 5 mm margins.
No significant difference was found across provider types for treatment of melanomas less than 1 mm in depth.
For invasive melanoma greater than 1 mm in depth, 54% of respondents used 1.1 cm to 1.9 cm margins, with most (67%) referring the patient to another provider. Both national guidelines recommend 1 cm to 2 cm margins for melanomas 1 mm to 2 mm in depth and 2 cm margins for melanoma greater than 2 mm in depth.
Academic dermatologists were significantly more likely than other dermatologists to treat these lesions rather than to refer the patient out (51% vs. 30%; P < .001).
“This is exciting new data that suggests that there still is a variance in early melanoma management,” Dr. Rigel, past president of AAD and ASDS, said in an interview. “The data suggest more studies need to be done to better access why this is occurring.”
Dr. Hensin Tsao, who served on the 2011 AAD guideline working group and is co-chairing the AAD’s pending guideline update, said in an interview that, “Dr. Rigel is well respected in the field and the project will undoubtedly be submitted for publication and subject to further review. It is worthwhile to wait on the final published results and conclusions.”
He agreed, however, with the authors’ suggestion that there is significant variation in practice. Regarding the finding that 36% of respondents use a shave biopsy for suspicious lesions, the AAD guidelines recommend that the entire lesion be removed with a 1 mm to 3 mm margin, which can be accomplished by an elliptical or punch excision with sutures or shave removal to a depth below the anticipated plane of the lesion, Dr. Tsao, of Massachusetts General Hospital in Boston, said.
“It is quite possible that some of the respondents to the questionnaire interpreted ‘shave biopsy’ as a full shave disk excision,” he said. “That said, intentional and routine partial sampling of suspected melanomas would be at odds with the guidelines.”
It is not inappropriate to remove a suspicious lesion, if small enough, with a punch biopsy, Dr. Tsao said, adding, “Perhaps again, the respondents failed to distinguish between partial punch biopsy and punch excision.”
On occasion, the AAD guidelines also make accommodations for an incisional biopsy “of the clinically or dermatoscopically most atypical portion of the lesion.” In this situation, a smaller incisional punch biopsy may be performed of the highly suspicious area.
“There are certainly areas that the investigators have identified which could represent potential knowledge gaps,” Dr. Tsao said. “For instance, 14% of the respondents used a 0.6 cm to 1.0 cm (6 mm-10 mm) margin for melanoma greater than 1 mm.”
Dermatologists’ surveillance of patients in the survey was somewhat less divergent. The most recommended follow-up interval for patients diagnosed within the last 5 years, was 6 months (49%), followed by a 3-month interval (25%), and other (24%). Follow-up was extended to yearly by 63% of dermatologists for patients diagnosed more than five years earlier, Dr. Farberg and Dr. Rigel reported.
Both the AAD and NCCN recommend follow-up every 3 to 12 months for those diagnosed with melanoma within the previous 5 years, while for those diagnosed more than 5 years prior, the AAD recommends follow-up every 3 to 12 months and the NCCN every 12 months.
“Adherence to evidence-based guidelines should lead to improved patient outcomes and quality of care. However, newer studies and emerging data may also justify deviations from existing guidelines, suggesting review of those guidelines may be indicated,” Dr. Farberg and Dr. Rigel concluded.
For example, a prospective series examining surgical margins in 1,072 patients with 1,120 malignant melanoma in situs showed that only 86% were successfully excised with a 6-mm margin, significantly less than the 98.9% clearance achieved with a 9-mm margin, Dr. Farberg told this publication.
That said, a 9-mm margin may not be appropriate for all lesions, such as those on the face, he observed.
The investigators said they hope the survey results will spur on revision of the guidelines, last updated in 2011.
Limitations of the survey include a lack of information on clinical factors such as patient history or anatomic site, the survey may have led to generalized answers, and access to care and reimbursement also may have impacted management, the authors noted.
The response rate to the survey was also low at 8%, with 6,177 practicing U.S. dermatologists surveyed. The demographics of the respondents, however, strongly reflected the full AAD membership, Dr. Farberg said. No significant geographical differences were observed.
AT THE ASDS ANNUAL MEETING
Key clinical point: Significant variance exists in dermatologists’ management of melanoma.
Major finding: Only 31% of dermatologists used narrow excision as recommended to biopsy suspicious lesions.
Data source: Survey of 510 U.S. practicing dermatologists.
Disclosures: The authors reported having no financial disclosures.
Hyaluronidase eases post-Mohs periorbital swelling
CHICAGO – Hyaluronidase can speed the resolution of postoperative periorbital lymphedema in patients undergoing Mohs micrographic surgery and flap repair, a prospective case series suggests.
Lymphedema resolved in all seven cases treated with hyaluronidase (Hyalase) injections in 4-6 weeks, compared with 3 months as would be expected, Dr. Sweta Rai, of St John’s Institute of Dermatology, King’s College London, said at the annual meeting of the American Society for Dermatologic Surgery.
“In the periorbital area where the skin is very thin and therefore even small amounts of lymphovascular fluid is visible, postoperative lymphedema is a cosmetic concern, especially as patients want to resume their daily activities as soon as possible postoperatively,” she said in an interview.
Hyaluronidase is widely used in cosmetic surgery in the breakdown of hyaluronic acid fillers, where the mucolytic enzyme splits and lowers the viscosity of hyaluronic acid in the extracellular matrix.
Dr. Rai and her coauthor Dr. Hooman Khorasani, chief of Mohs, reconstructive, and cosmetic surgery at Mount Sinai School of Medicine in New York, turned to hyaluronidase because it’s well documented that hyaluronic acid is produced by the body as an automatic response to promote wound healing
Patients undergoing Mohs surgery for large eye tumors often require complex flap repairs that cross the lower eyelid and cheek junction, which results in greater lymphedema. Hyaluronic acid produces a scaffolding effect at the wound site that, in combination with periorbital lymphedema when the vascular channels are cut, is thought to lead to fluid stasis. Hyaluronidase breaks down this scaffolding, allowing the lymphovascular fluid to drain into the subcutaneous tissue, Dr. Rai explained.
The investigators use a 1,500-unit vial of generic hyaluronidase diluted with 1.5 mL of normal saline and inject 100-150 units subcutaneously starting 2 weeks postoperatively at the time of suture removal and repeat the injections every 2 weeks until the swelling resolves.
Patients should undergo an intradermal prick test prior to injections to exclude the risk of type I hypersensitivity anaphylaxis previously reported with human hyaluronidase injections, Dr. Rai cautioned.
In all seven patients, aged 42-80 years, periorbital lymphedema resolved with 150-450 units of hyaluronidase. The patients included a women referred for treatment 2 months after Mohs surgery. The index case, involving a man with a periorbital defect and a medially based advancement flap, resolved with only a single 150-unit injection given 2 weeks after surgery, Dr. Rai said.
“Most of my patients are working and lead busy work and social lives, and they’ve all commented on how pleased they are with the results and on how quickly they are able to resume their normal lives,” she said.
The maximum number of injections needed in the cohort was three. No adverse events have been reported.
Session comoderator Dr. Seemal Desai, a dermatologist in private practice near Dallas, said the technique is very practical, hits an unmet need, and could potentially prevent tropia when used around the eye.
“My only comment is that if you’re using human hyaluronidase, the skin testing to make sure there is no anaphylaxis is important,” he said. “But if you’re using synthetic or recombinant hyaluronidase, which is really what we use here more, I don’t think that would be an issue. I think this was a great idea to do this, especially for advancement flaps.”
Fellow comoderator and Mohs surgeon Dr. Ramona Behshad, in private practice in St. Louis, Mo., said the case series provides a novel and practical use for hyaluronidase, which is “very underused” in dermatology practices and often goes to waste because it expires.
Dr. Rai and her maxillofacial surgery colleagues at King’s College are performing a randomized controlled trial using hyaluronidase on all head and neck postoperative wounds to assess its effect on postoperative lymphedema and recovery times with and without the agent. “Hopefully, this will provide further information on its efficacy including other sites on the head and neck,” she said.
CHICAGO – Hyaluronidase can speed the resolution of postoperative periorbital lymphedema in patients undergoing Mohs micrographic surgery and flap repair, a prospective case series suggests.
Lymphedema resolved in all seven cases treated with hyaluronidase (Hyalase) injections in 4-6 weeks, compared with 3 months as would be expected, Dr. Sweta Rai, of St John’s Institute of Dermatology, King’s College London, said at the annual meeting of the American Society for Dermatologic Surgery.
“In the periorbital area where the skin is very thin and therefore even small amounts of lymphovascular fluid is visible, postoperative lymphedema is a cosmetic concern, especially as patients want to resume their daily activities as soon as possible postoperatively,” she said in an interview.
Hyaluronidase is widely used in cosmetic surgery in the breakdown of hyaluronic acid fillers, where the mucolytic enzyme splits and lowers the viscosity of hyaluronic acid in the extracellular matrix.
Dr. Rai and her coauthor Dr. Hooman Khorasani, chief of Mohs, reconstructive, and cosmetic surgery at Mount Sinai School of Medicine in New York, turned to hyaluronidase because it’s well documented that hyaluronic acid is produced by the body as an automatic response to promote wound healing
Patients undergoing Mohs surgery for large eye tumors often require complex flap repairs that cross the lower eyelid and cheek junction, which results in greater lymphedema. Hyaluronic acid produces a scaffolding effect at the wound site that, in combination with periorbital lymphedema when the vascular channels are cut, is thought to lead to fluid stasis. Hyaluronidase breaks down this scaffolding, allowing the lymphovascular fluid to drain into the subcutaneous tissue, Dr. Rai explained.
The investigators use a 1,500-unit vial of generic hyaluronidase diluted with 1.5 mL of normal saline and inject 100-150 units subcutaneously starting 2 weeks postoperatively at the time of suture removal and repeat the injections every 2 weeks until the swelling resolves.
Patients should undergo an intradermal prick test prior to injections to exclude the risk of type I hypersensitivity anaphylaxis previously reported with human hyaluronidase injections, Dr. Rai cautioned.
In all seven patients, aged 42-80 years, periorbital lymphedema resolved with 150-450 units of hyaluronidase. The patients included a women referred for treatment 2 months after Mohs surgery. The index case, involving a man with a periorbital defect and a medially based advancement flap, resolved with only a single 150-unit injection given 2 weeks after surgery, Dr. Rai said.
“Most of my patients are working and lead busy work and social lives, and they’ve all commented on how pleased they are with the results and on how quickly they are able to resume their normal lives,” she said.
The maximum number of injections needed in the cohort was three. No adverse events have been reported.
Session comoderator Dr. Seemal Desai, a dermatologist in private practice near Dallas, said the technique is very practical, hits an unmet need, and could potentially prevent tropia when used around the eye.
“My only comment is that if you’re using human hyaluronidase, the skin testing to make sure there is no anaphylaxis is important,” he said. “But if you’re using synthetic or recombinant hyaluronidase, which is really what we use here more, I don’t think that would be an issue. I think this was a great idea to do this, especially for advancement flaps.”
Fellow comoderator and Mohs surgeon Dr. Ramona Behshad, in private practice in St. Louis, Mo., said the case series provides a novel and practical use for hyaluronidase, which is “very underused” in dermatology practices and often goes to waste because it expires.
Dr. Rai and her maxillofacial surgery colleagues at King’s College are performing a randomized controlled trial using hyaluronidase on all head and neck postoperative wounds to assess its effect on postoperative lymphedema and recovery times with and without the agent. “Hopefully, this will provide further information on its efficacy including other sites on the head and neck,” she said.
CHICAGO – Hyaluronidase can speed the resolution of postoperative periorbital lymphedema in patients undergoing Mohs micrographic surgery and flap repair, a prospective case series suggests.
Lymphedema resolved in all seven cases treated with hyaluronidase (Hyalase) injections in 4-6 weeks, compared with 3 months as would be expected, Dr. Sweta Rai, of St John’s Institute of Dermatology, King’s College London, said at the annual meeting of the American Society for Dermatologic Surgery.
“In the periorbital area where the skin is very thin and therefore even small amounts of lymphovascular fluid is visible, postoperative lymphedema is a cosmetic concern, especially as patients want to resume their daily activities as soon as possible postoperatively,” she said in an interview.
Hyaluronidase is widely used in cosmetic surgery in the breakdown of hyaluronic acid fillers, where the mucolytic enzyme splits and lowers the viscosity of hyaluronic acid in the extracellular matrix.
Dr. Rai and her coauthor Dr. Hooman Khorasani, chief of Mohs, reconstructive, and cosmetic surgery at Mount Sinai School of Medicine in New York, turned to hyaluronidase because it’s well documented that hyaluronic acid is produced by the body as an automatic response to promote wound healing
Patients undergoing Mohs surgery for large eye tumors often require complex flap repairs that cross the lower eyelid and cheek junction, which results in greater lymphedema. Hyaluronic acid produces a scaffolding effect at the wound site that, in combination with periorbital lymphedema when the vascular channels are cut, is thought to lead to fluid stasis. Hyaluronidase breaks down this scaffolding, allowing the lymphovascular fluid to drain into the subcutaneous tissue, Dr. Rai explained.
The investigators use a 1,500-unit vial of generic hyaluronidase diluted with 1.5 mL of normal saline and inject 100-150 units subcutaneously starting 2 weeks postoperatively at the time of suture removal and repeat the injections every 2 weeks until the swelling resolves.
Patients should undergo an intradermal prick test prior to injections to exclude the risk of type I hypersensitivity anaphylaxis previously reported with human hyaluronidase injections, Dr. Rai cautioned.
In all seven patients, aged 42-80 years, periorbital lymphedema resolved with 150-450 units of hyaluronidase. The patients included a women referred for treatment 2 months after Mohs surgery. The index case, involving a man with a periorbital defect and a medially based advancement flap, resolved with only a single 150-unit injection given 2 weeks after surgery, Dr. Rai said.
“Most of my patients are working and lead busy work and social lives, and they’ve all commented on how pleased they are with the results and on how quickly they are able to resume their normal lives,” she said.
The maximum number of injections needed in the cohort was three. No adverse events have been reported.
Session comoderator Dr. Seemal Desai, a dermatologist in private practice near Dallas, said the technique is very practical, hits an unmet need, and could potentially prevent tropia when used around the eye.
“My only comment is that if you’re using human hyaluronidase, the skin testing to make sure there is no anaphylaxis is important,” he said. “But if you’re using synthetic or recombinant hyaluronidase, which is really what we use here more, I don’t think that would be an issue. I think this was a great idea to do this, especially for advancement flaps.”
Fellow comoderator and Mohs surgeon Dr. Ramona Behshad, in private practice in St. Louis, Mo., said the case series provides a novel and practical use for hyaluronidase, which is “very underused” in dermatology practices and often goes to waste because it expires.
Dr. Rai and her maxillofacial surgery colleagues at King’s College are performing a randomized controlled trial using hyaluronidase on all head and neck postoperative wounds to assess its effect on postoperative lymphedema and recovery times with and without the agent. “Hopefully, this will provide further information on its efficacy including other sites on the head and neck,” she said.
AT THE ASDS ANNUAL MEETING
Key clinical point: Hyaluronidase injections speed resolution of periorbital postoperative lymphedema in patients undergoing Mohs surgery and flap repair.
Major finding: Lymphedema resolved in all seven cases within 4-6 weeks of hyaluronidase administration.
Data source: The study was a prospective case series of seven patients.
Disclosures: The authors reported having no financial disclosures.
Biopsy-site photography an easy winner on all counts
CHICAGO – Biopsy-site photography appears to reduce the risk of potential wrong-site surgery and can easily be incorporated into dermatology practice, according to Dr. Jeremy Etzkorn.
When Dr. Etzkorn took on this quality improvement initiative on his own, only 5 of 239 routine biopsy-site photographs evaluated were inadequate. The biopsy site was not clearly marked in two photos with multiple suspicious lesions, and anatomic landmarks were absent in three.
“Almost 98% of the time, the photograph was adequate, which just shows it doesn’t require much training or time to get images of the skin,” the Mohs surgeon said at the annual meeting of the American Society for Dermatologic Surgery.
Biopsy-site photos were taken primarily by medical assistants, as well as nurses, who received minimal, informal training on digital photography and were guided to take at least one photograph with anatomic landmarks present.
Dr. Etzkorn of the University of Pennsylvania Health System, Philadelphia, conducted a prospective, observational cohort study of 329 patients/tumors referred for Mohs micrographic surgery or standard excision to the dermatologic surgery unit at Penn Dermatology. Patients were asked to identify their biopsy site, indicate whether they remembered a photo being taken, and quantify on a 10-point scale their level of confidence that the originally biopsied site was treated on the day of surgery.
Dr. Etzkorn identified the biopsy site before consulting the medical record for a biopsy-site photograph. If the photo was absent and he and the patient agreed on the biopsy site, they proceeded to surgery. If there was any disagreement, surgery was postponed and the referring physician consulted.
Overall, 239 patients (73%) had biopsy-site photographs, and 90 patients (27%), referred to the practice before photography was implemented, did not.
In 12.5% of cases, the patient misidentified the biopsy site, and in 6.7% of cases the physician did, which is similar to what has been reported in the literature, Dr. Etzkorn said.
Biopsy-site photography prevented wrong-site surgery in 3 of the 239 cases (1.25%) where these photographs were available. “Without the photo I would normally have done surgery on that site because the patient was confident it was the right site; I was confident it was the right site,” he said.
Importantly, all three lesions were biopsied, and all were squamous cell carcinoma in situ. So while it was the wrong site, the surgery would not have been inappropriate, Dr. Etzkorn noted.
Surgery was postponed to consult the referring physician in 3% of cases (10/329).
Complete patient confidence (10 of 10 points) that the correct site was treated was achieved in 95% of cases, with most of the remaining patients at 9 of 10 points, he said.
Risk factors for patient biopsy-site misidentification were the inability to see the site without a mirror (odds ratio, 3.95; P = .002) and time between the biopsy and surgery (OR, 2.19; P = .028). Prior studies have also shown that difficult-to-visualize sites are associated with biopsy-site misidentification, he noted.
For Dr. Etzkorn, the risk of biopsy-site misidentification quadrupled if there were multiple simultaneous biopsies from different locations (OR, 4.39; P = .003) and tripled with longer time, defined as longer than a 6-week delay vs. a delay of less than 6 weeks between biopsy and surgery (OR, 3.68; P = .007).
A biopsy-site photograph significantly increased the odds that a patient was completely confident the correct site was treated (OR, 5.48; P = .001), as did the use of Mohs surgery vs. excision (OR, 4.87; P = .017).
Once again, time between the biopsy and surgery was a significant risk factor for postponing surgery (OR, 3.52; P = .035), whereas the presence of a biopsy-site photograph cut that risk by almost 13-fold (OR, 12.5: P less than .001), Dr. Etzkorn reported.
“Biopsy-site photography is associated with increased patient confidence that the correct site is treated, decreases in surgical postponement, and the ability to identify wrong-site surgery and prevent it,” he concluded.
Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
CHICAGO – Biopsy-site photography appears to reduce the risk of potential wrong-site surgery and can easily be incorporated into dermatology practice, according to Dr. Jeremy Etzkorn.
When Dr. Etzkorn took on this quality improvement initiative on his own, only 5 of 239 routine biopsy-site photographs evaluated were inadequate. The biopsy site was not clearly marked in two photos with multiple suspicious lesions, and anatomic landmarks were absent in three.
“Almost 98% of the time, the photograph was adequate, which just shows it doesn’t require much training or time to get images of the skin,” the Mohs surgeon said at the annual meeting of the American Society for Dermatologic Surgery.
Biopsy-site photos were taken primarily by medical assistants, as well as nurses, who received minimal, informal training on digital photography and were guided to take at least one photograph with anatomic landmarks present.
Dr. Etzkorn of the University of Pennsylvania Health System, Philadelphia, conducted a prospective, observational cohort study of 329 patients/tumors referred for Mohs micrographic surgery or standard excision to the dermatologic surgery unit at Penn Dermatology. Patients were asked to identify their biopsy site, indicate whether they remembered a photo being taken, and quantify on a 10-point scale their level of confidence that the originally biopsied site was treated on the day of surgery.
Dr. Etzkorn identified the biopsy site before consulting the medical record for a biopsy-site photograph. If the photo was absent and he and the patient agreed on the biopsy site, they proceeded to surgery. If there was any disagreement, surgery was postponed and the referring physician consulted.
Overall, 239 patients (73%) had biopsy-site photographs, and 90 patients (27%), referred to the practice before photography was implemented, did not.
In 12.5% of cases, the patient misidentified the biopsy site, and in 6.7% of cases the physician did, which is similar to what has been reported in the literature, Dr. Etzkorn said.
Biopsy-site photography prevented wrong-site surgery in 3 of the 239 cases (1.25%) where these photographs were available. “Without the photo I would normally have done surgery on that site because the patient was confident it was the right site; I was confident it was the right site,” he said.
Importantly, all three lesions were biopsied, and all were squamous cell carcinoma in situ. So while it was the wrong site, the surgery would not have been inappropriate, Dr. Etzkorn noted.
Surgery was postponed to consult the referring physician in 3% of cases (10/329).
Complete patient confidence (10 of 10 points) that the correct site was treated was achieved in 95% of cases, with most of the remaining patients at 9 of 10 points, he said.
Risk factors for patient biopsy-site misidentification were the inability to see the site without a mirror (odds ratio, 3.95; P = .002) and time between the biopsy and surgery (OR, 2.19; P = .028). Prior studies have also shown that difficult-to-visualize sites are associated with biopsy-site misidentification, he noted.
For Dr. Etzkorn, the risk of biopsy-site misidentification quadrupled if there were multiple simultaneous biopsies from different locations (OR, 4.39; P = .003) and tripled with longer time, defined as longer than a 6-week delay vs. a delay of less than 6 weeks between biopsy and surgery (OR, 3.68; P = .007).
A biopsy-site photograph significantly increased the odds that a patient was completely confident the correct site was treated (OR, 5.48; P = .001), as did the use of Mohs surgery vs. excision (OR, 4.87; P = .017).
Once again, time between the biopsy and surgery was a significant risk factor for postponing surgery (OR, 3.52; P = .035), whereas the presence of a biopsy-site photograph cut that risk by almost 13-fold (OR, 12.5: P less than .001), Dr. Etzkorn reported.
“Biopsy-site photography is associated with increased patient confidence that the correct site is treated, decreases in surgical postponement, and the ability to identify wrong-site surgery and prevent it,” he concluded.
Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
CHICAGO – Biopsy-site photography appears to reduce the risk of potential wrong-site surgery and can easily be incorporated into dermatology practice, according to Dr. Jeremy Etzkorn.
When Dr. Etzkorn took on this quality improvement initiative on his own, only 5 of 239 routine biopsy-site photographs evaluated were inadequate. The biopsy site was not clearly marked in two photos with multiple suspicious lesions, and anatomic landmarks were absent in three.
“Almost 98% of the time, the photograph was adequate, which just shows it doesn’t require much training or time to get images of the skin,” the Mohs surgeon said at the annual meeting of the American Society for Dermatologic Surgery.
Biopsy-site photos were taken primarily by medical assistants, as well as nurses, who received minimal, informal training on digital photography and were guided to take at least one photograph with anatomic landmarks present.
Dr. Etzkorn of the University of Pennsylvania Health System, Philadelphia, conducted a prospective, observational cohort study of 329 patients/tumors referred for Mohs micrographic surgery or standard excision to the dermatologic surgery unit at Penn Dermatology. Patients were asked to identify their biopsy site, indicate whether they remembered a photo being taken, and quantify on a 10-point scale their level of confidence that the originally biopsied site was treated on the day of surgery.
Dr. Etzkorn identified the biopsy site before consulting the medical record for a biopsy-site photograph. If the photo was absent and he and the patient agreed on the biopsy site, they proceeded to surgery. If there was any disagreement, surgery was postponed and the referring physician consulted.
Overall, 239 patients (73%) had biopsy-site photographs, and 90 patients (27%), referred to the practice before photography was implemented, did not.
In 12.5% of cases, the patient misidentified the biopsy site, and in 6.7% of cases the physician did, which is similar to what has been reported in the literature, Dr. Etzkorn said.
Biopsy-site photography prevented wrong-site surgery in 3 of the 239 cases (1.25%) where these photographs were available. “Without the photo I would normally have done surgery on that site because the patient was confident it was the right site; I was confident it was the right site,” he said.
Importantly, all three lesions were biopsied, and all were squamous cell carcinoma in situ. So while it was the wrong site, the surgery would not have been inappropriate, Dr. Etzkorn noted.
Surgery was postponed to consult the referring physician in 3% of cases (10/329).
Complete patient confidence (10 of 10 points) that the correct site was treated was achieved in 95% of cases, with most of the remaining patients at 9 of 10 points, he said.
Risk factors for patient biopsy-site misidentification were the inability to see the site without a mirror (odds ratio, 3.95; P = .002) and time between the biopsy and surgery (OR, 2.19; P = .028). Prior studies have also shown that difficult-to-visualize sites are associated with biopsy-site misidentification, he noted.
For Dr. Etzkorn, the risk of biopsy-site misidentification quadrupled if there were multiple simultaneous biopsies from different locations (OR, 4.39; P = .003) and tripled with longer time, defined as longer than a 6-week delay vs. a delay of less than 6 weeks between biopsy and surgery (OR, 3.68; P = .007).
A biopsy-site photograph significantly increased the odds that a patient was completely confident the correct site was treated (OR, 5.48; P = .001), as did the use of Mohs surgery vs. excision (OR, 4.87; P = .017).
Once again, time between the biopsy and surgery was a significant risk factor for postponing surgery (OR, 3.52; P = .035), whereas the presence of a biopsy-site photograph cut that risk by almost 13-fold (OR, 12.5: P less than .001), Dr. Etzkorn reported.
“Biopsy-site photography is associated with increased patient confidence that the correct site is treated, decreases in surgical postponement, and the ability to identify wrong-site surgery and prevent it,” he concluded.
Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
AT THE ASDS ANNUAL MEETING
Key clinical point: Biopsy-site photography reduces surgical delays, identifies potential wrong-site surgery, and increases patient confidence.
Major finding: Having biopsy-site photos can help prevent wrong-site surgery.
Data source: A prospective, observational cohort study of 329 patients referred for Mohs surgery or standard excision.
Disclosures: Dr. Etzkorn and his coauthor reported having no relevant financial disclosures.
Deoxycholic acid effective in trimming extreme and very mild chin fat
CHICAGO – Deoxycholic acid injections benefit patients on either end of the spectrum with mild or extreme submental fat, a phase III safety study shows.
“What this study shows is that the applicability of the product is wider than what’s represented in the registration trials because they looked at a very narrow band and this includes people with very mild and extreme [submental fat],” Dr. Richard G. Glogau of San Francisco Dermatology and the University of California, San Francisco, said in an interview. He presented the results of the study at the annual meeting of the American Society for Dermatologic Surgery.
Deoxycholic acid gained U.S. approval in April 2015 as the first injectable cytolytic drug to treat moderate to severe convexity or fullness associated with submental fat (SMF) in adults. It is marketed as Kybella.
Because treatment can be tailored based on the amount and thickness of SMF, the study sought to evaluate deoxycholic acid 2 mg/cm2 or placebo for up to six treatments 1 month apart in 47 patients with mild SMF and 46 patients with extreme SMF based on Clinician-Reported Submental Fat Rating Scale (CR-SMFRS) scores of 1 (mild) or 4 (extreme).
The predominantly female cohort had an average age of 48 years in the mild SMF group and 51 years in the extreme SMF group and a mean body mass index of 25 kg/m2 and 32.5 kg/m2, respectively. About 30% of patients in the extreme SMF group had moderate to severe skin laxity compared with about 15% in the mild SMF group.
The mean number of treatment sessions was 4.9 for placebo and 4.2 for deoxycholic acid in the mild SMF group, and 5.6 for placebo and 4.9 for deoxycholic acid in the extreme SMF group.
“I don’t think in the real world that’s our experience,” Dr. Glogau said at the meeting. “People in the mild group get by with much less and, conversely, people at the extreme end would be happy to go on higher than four or five treatments, depending on what size they started with.”
The mean total injection volume across all treatments was 17.2 mL, 13.9 mL, 38.4 mL, and 31.6 mL, respectively, which is consistent with the need for less product in mild SMF.
In the mild SMF group, SMF was reduced by one grade in significantly more patients following deoxycholic acid treatment than placebo as measured with the CR-SMFRS (74.2% vs. 20%), the Patient-Rated SMFRS (67.7% vs. 33.3%), or a composite of the two scales (61.3% vs. 6.7%).
The percentages of patients with extreme SMF achieving a one-grade improvement with deoxycholic acid were even higher: CR-SMFRS (96.4% vs. 26.7%), PR-SMFRS (89.3% vs. 46.7%), or the composite (89.3% vs. 13.3%), said Dr. Glogau.
Moreover, SMF improved by two grades on the composite endpoint in 43% of extreme SMF patients treated with deoxycholic acid vs. 0% given placebo. P values for all comparisons were less than .05.
“To reach a two-grade change in virtually anything you want to study is difficult to achieve, so I think this is a significant landmark that came out of this study,” Dr. Glogau said.
Significantly more deoxycholic acid–treated patients also reported being satisfied with the appearance of their face and chin compared with those given placebo in the mild SMF (80% vs. 46.7%; P less than .05) and extreme SMF (71.4% vs. 0%; P less than .05) groups.
Despite reductions in SMF, skin laxity was unchanged or got only slightly better from baseline in all patients on deoxycholic acid. This is not surprising, because deoxycholic acid exerts its killing effect on fat cells only, not on fibrous septae or the dermis, and skin laxity is a reflection of inherent elasticity in the dermis, together with the fibrous septae in the fat running between skin and muscle, Dr. Glogau explained.
Most adverse events were mild or moderate in severity and transient in nature, he said. Among mild SMF patients, pain was reported in 74% treated with deoxycholic acid vs. 50% with placebo, bruising in 48% vs. 50%, edema in 42% vs. 25%, numbness in 48% vs. 6%, and swelling in 42% vs. 13%. The percentages were generally similar in the extreme SMF group.
“I think the incidence of hematoma and bruising is actually a function of injection technique and numbers out in clinical practice are somewhat lower,” Dr. Glogau observed.
No drug-related serious adverse events were reported. Nerve paresis was reported in two deoxycholic acid–treated patients with mild SMF and resolved without sequelae after 4 days and after 52 days.
Dysphagia was reported in one deoxycholic acid–treated patient with extreme SMF and resolved without sequelae after 2 days.
None of the events precluded patients from receiving additional treatment, even within the 30-day interval, he said, adding that in practice most clinicians are using longer breaks between treatments.
During a discussion of the study, Dr. Glogau said he uses lidocaine to reduce pain and that local anesthesia should be standard with deoxycholic acid injections.
Fellow presenter Dr. Brian Biesman, director of the Nashville (Tenn.) Centre for Laser and Facial Surgery, said that he was injected with deoxycholic acid both with and without local anesthesia and that they’ve used local anesthesia ever since.
“It makes a huge difference from a patient experience standpoint, of being extraordinarily unpleasant without it – and I have a pretty good pain tolerance – to being extraordinarily unremarkable,” Dr. Biesman said.
Session moderator Dr. Wendy Roberts of Dermatology Rancho Mirage (Calif.), said that Dr. Glogau’s study provides clinicians with data to support deoxycholic acid use in a broader range of patients.
“Now we have a real resource that we can reference and say as a matter of fact, for mild submental fullness you will get a result and this is the study. So you’re not wasting your money, you’re not wasting your time,” she said in an interview. “I think it’s extremely important. In Southern California where I practice, people don’t want to get to be moderate to severe.”
The oral abstract session included several other deoxycholic acid presentations including long-term follow-up from phase II/III trials showing that improvements in SMF severity are maintained for up to 4 years after treatment. The improvements were due to deoxycholic acid treatment, as body weight did not significantly change throughout the follow-up period, said study author Dr. Ashish Bhatia of the DuPage Medical Group, in Naperville, Ill.
Dr. Kenneth Beer of Palm Beach (Fla.) Cosmetic, provided details on the ongoing Kythera-sponsored CONTOUR: Condition of Submental Fullness and Treatment Outcomes Registry study looking at how SMF is treated in clinical practice and the risks and benefits associated with treatment.
Kythera Biopharmaceuticals markets Kybella, which is also known as ATX-101. Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera. Several coauthors also disclosed ties to the company.
CHICAGO – Deoxycholic acid injections benefit patients on either end of the spectrum with mild or extreme submental fat, a phase III safety study shows.
“What this study shows is that the applicability of the product is wider than what’s represented in the registration trials because they looked at a very narrow band and this includes people with very mild and extreme [submental fat],” Dr. Richard G. Glogau of San Francisco Dermatology and the University of California, San Francisco, said in an interview. He presented the results of the study at the annual meeting of the American Society for Dermatologic Surgery.
Deoxycholic acid gained U.S. approval in April 2015 as the first injectable cytolytic drug to treat moderate to severe convexity or fullness associated with submental fat (SMF) in adults. It is marketed as Kybella.
Because treatment can be tailored based on the amount and thickness of SMF, the study sought to evaluate deoxycholic acid 2 mg/cm2 or placebo for up to six treatments 1 month apart in 47 patients with mild SMF and 46 patients with extreme SMF based on Clinician-Reported Submental Fat Rating Scale (CR-SMFRS) scores of 1 (mild) or 4 (extreme).
The predominantly female cohort had an average age of 48 years in the mild SMF group and 51 years in the extreme SMF group and a mean body mass index of 25 kg/m2 and 32.5 kg/m2, respectively. About 30% of patients in the extreme SMF group had moderate to severe skin laxity compared with about 15% in the mild SMF group.
The mean number of treatment sessions was 4.9 for placebo and 4.2 for deoxycholic acid in the mild SMF group, and 5.6 for placebo and 4.9 for deoxycholic acid in the extreme SMF group.
“I don’t think in the real world that’s our experience,” Dr. Glogau said at the meeting. “People in the mild group get by with much less and, conversely, people at the extreme end would be happy to go on higher than four or five treatments, depending on what size they started with.”
The mean total injection volume across all treatments was 17.2 mL, 13.9 mL, 38.4 mL, and 31.6 mL, respectively, which is consistent with the need for less product in mild SMF.
In the mild SMF group, SMF was reduced by one grade in significantly more patients following deoxycholic acid treatment than placebo as measured with the CR-SMFRS (74.2% vs. 20%), the Patient-Rated SMFRS (67.7% vs. 33.3%), or a composite of the two scales (61.3% vs. 6.7%).
The percentages of patients with extreme SMF achieving a one-grade improvement with deoxycholic acid were even higher: CR-SMFRS (96.4% vs. 26.7%), PR-SMFRS (89.3% vs. 46.7%), or the composite (89.3% vs. 13.3%), said Dr. Glogau.
Moreover, SMF improved by two grades on the composite endpoint in 43% of extreme SMF patients treated with deoxycholic acid vs. 0% given placebo. P values for all comparisons were less than .05.
“To reach a two-grade change in virtually anything you want to study is difficult to achieve, so I think this is a significant landmark that came out of this study,” Dr. Glogau said.
Significantly more deoxycholic acid–treated patients also reported being satisfied with the appearance of their face and chin compared with those given placebo in the mild SMF (80% vs. 46.7%; P less than .05) and extreme SMF (71.4% vs. 0%; P less than .05) groups.
Despite reductions in SMF, skin laxity was unchanged or got only slightly better from baseline in all patients on deoxycholic acid. This is not surprising, because deoxycholic acid exerts its killing effect on fat cells only, not on fibrous septae or the dermis, and skin laxity is a reflection of inherent elasticity in the dermis, together with the fibrous septae in the fat running between skin and muscle, Dr. Glogau explained.
Most adverse events were mild or moderate in severity and transient in nature, he said. Among mild SMF patients, pain was reported in 74% treated with deoxycholic acid vs. 50% with placebo, bruising in 48% vs. 50%, edema in 42% vs. 25%, numbness in 48% vs. 6%, and swelling in 42% vs. 13%. The percentages were generally similar in the extreme SMF group.
“I think the incidence of hematoma and bruising is actually a function of injection technique and numbers out in clinical practice are somewhat lower,” Dr. Glogau observed.
No drug-related serious adverse events were reported. Nerve paresis was reported in two deoxycholic acid–treated patients with mild SMF and resolved without sequelae after 4 days and after 52 days.
Dysphagia was reported in one deoxycholic acid–treated patient with extreme SMF and resolved without sequelae after 2 days.
None of the events precluded patients from receiving additional treatment, even within the 30-day interval, he said, adding that in practice most clinicians are using longer breaks between treatments.
During a discussion of the study, Dr. Glogau said he uses lidocaine to reduce pain and that local anesthesia should be standard with deoxycholic acid injections.
Fellow presenter Dr. Brian Biesman, director of the Nashville (Tenn.) Centre for Laser and Facial Surgery, said that he was injected with deoxycholic acid both with and without local anesthesia and that they’ve used local anesthesia ever since.
“It makes a huge difference from a patient experience standpoint, of being extraordinarily unpleasant without it – and I have a pretty good pain tolerance – to being extraordinarily unremarkable,” Dr. Biesman said.
Session moderator Dr. Wendy Roberts of Dermatology Rancho Mirage (Calif.), said that Dr. Glogau’s study provides clinicians with data to support deoxycholic acid use in a broader range of patients.
“Now we have a real resource that we can reference and say as a matter of fact, for mild submental fullness you will get a result and this is the study. So you’re not wasting your money, you’re not wasting your time,” she said in an interview. “I think it’s extremely important. In Southern California where I practice, people don’t want to get to be moderate to severe.”
The oral abstract session included several other deoxycholic acid presentations including long-term follow-up from phase II/III trials showing that improvements in SMF severity are maintained for up to 4 years after treatment. The improvements were due to deoxycholic acid treatment, as body weight did not significantly change throughout the follow-up period, said study author Dr. Ashish Bhatia of the DuPage Medical Group, in Naperville, Ill.
Dr. Kenneth Beer of Palm Beach (Fla.) Cosmetic, provided details on the ongoing Kythera-sponsored CONTOUR: Condition of Submental Fullness and Treatment Outcomes Registry study looking at how SMF is treated in clinical practice and the risks and benefits associated with treatment.
Kythera Biopharmaceuticals markets Kybella, which is also known as ATX-101. Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera. Several coauthors also disclosed ties to the company.
CHICAGO – Deoxycholic acid injections benefit patients on either end of the spectrum with mild or extreme submental fat, a phase III safety study shows.
“What this study shows is that the applicability of the product is wider than what’s represented in the registration trials because they looked at a very narrow band and this includes people with very mild and extreme [submental fat],” Dr. Richard G. Glogau of San Francisco Dermatology and the University of California, San Francisco, said in an interview. He presented the results of the study at the annual meeting of the American Society for Dermatologic Surgery.
Deoxycholic acid gained U.S. approval in April 2015 as the first injectable cytolytic drug to treat moderate to severe convexity or fullness associated with submental fat (SMF) in adults. It is marketed as Kybella.
Because treatment can be tailored based on the amount and thickness of SMF, the study sought to evaluate deoxycholic acid 2 mg/cm2 or placebo for up to six treatments 1 month apart in 47 patients with mild SMF and 46 patients with extreme SMF based on Clinician-Reported Submental Fat Rating Scale (CR-SMFRS) scores of 1 (mild) or 4 (extreme).
The predominantly female cohort had an average age of 48 years in the mild SMF group and 51 years in the extreme SMF group and a mean body mass index of 25 kg/m2 and 32.5 kg/m2, respectively. About 30% of patients in the extreme SMF group had moderate to severe skin laxity compared with about 15% in the mild SMF group.
The mean number of treatment sessions was 4.9 for placebo and 4.2 for deoxycholic acid in the mild SMF group, and 5.6 for placebo and 4.9 for deoxycholic acid in the extreme SMF group.
“I don’t think in the real world that’s our experience,” Dr. Glogau said at the meeting. “People in the mild group get by with much less and, conversely, people at the extreme end would be happy to go on higher than four or five treatments, depending on what size they started with.”
The mean total injection volume across all treatments was 17.2 mL, 13.9 mL, 38.4 mL, and 31.6 mL, respectively, which is consistent with the need for less product in mild SMF.
In the mild SMF group, SMF was reduced by one grade in significantly more patients following deoxycholic acid treatment than placebo as measured with the CR-SMFRS (74.2% vs. 20%), the Patient-Rated SMFRS (67.7% vs. 33.3%), or a composite of the two scales (61.3% vs. 6.7%).
The percentages of patients with extreme SMF achieving a one-grade improvement with deoxycholic acid were even higher: CR-SMFRS (96.4% vs. 26.7%), PR-SMFRS (89.3% vs. 46.7%), or the composite (89.3% vs. 13.3%), said Dr. Glogau.
Moreover, SMF improved by two grades on the composite endpoint in 43% of extreme SMF patients treated with deoxycholic acid vs. 0% given placebo. P values for all comparisons were less than .05.
“To reach a two-grade change in virtually anything you want to study is difficult to achieve, so I think this is a significant landmark that came out of this study,” Dr. Glogau said.
Significantly more deoxycholic acid–treated patients also reported being satisfied with the appearance of their face and chin compared with those given placebo in the mild SMF (80% vs. 46.7%; P less than .05) and extreme SMF (71.4% vs. 0%; P less than .05) groups.
Despite reductions in SMF, skin laxity was unchanged or got only slightly better from baseline in all patients on deoxycholic acid. This is not surprising, because deoxycholic acid exerts its killing effect on fat cells only, not on fibrous septae or the dermis, and skin laxity is a reflection of inherent elasticity in the dermis, together with the fibrous septae in the fat running between skin and muscle, Dr. Glogau explained.
Most adverse events were mild or moderate in severity and transient in nature, he said. Among mild SMF patients, pain was reported in 74% treated with deoxycholic acid vs. 50% with placebo, bruising in 48% vs. 50%, edema in 42% vs. 25%, numbness in 48% vs. 6%, and swelling in 42% vs. 13%. The percentages were generally similar in the extreme SMF group.
“I think the incidence of hematoma and bruising is actually a function of injection technique and numbers out in clinical practice are somewhat lower,” Dr. Glogau observed.
No drug-related serious adverse events were reported. Nerve paresis was reported in two deoxycholic acid–treated patients with mild SMF and resolved without sequelae after 4 days and after 52 days.
Dysphagia was reported in one deoxycholic acid–treated patient with extreme SMF and resolved without sequelae after 2 days.
None of the events precluded patients from receiving additional treatment, even within the 30-day interval, he said, adding that in practice most clinicians are using longer breaks between treatments.
During a discussion of the study, Dr. Glogau said he uses lidocaine to reduce pain and that local anesthesia should be standard with deoxycholic acid injections.
Fellow presenter Dr. Brian Biesman, director of the Nashville (Tenn.) Centre for Laser and Facial Surgery, said that he was injected with deoxycholic acid both with and without local anesthesia and that they’ve used local anesthesia ever since.
“It makes a huge difference from a patient experience standpoint, of being extraordinarily unpleasant without it – and I have a pretty good pain tolerance – to being extraordinarily unremarkable,” Dr. Biesman said.
Session moderator Dr. Wendy Roberts of Dermatology Rancho Mirage (Calif.), said that Dr. Glogau’s study provides clinicians with data to support deoxycholic acid use in a broader range of patients.
“Now we have a real resource that we can reference and say as a matter of fact, for mild submental fullness you will get a result and this is the study. So you’re not wasting your money, you’re not wasting your time,” she said in an interview. “I think it’s extremely important. In Southern California where I practice, people don’t want to get to be moderate to severe.”
The oral abstract session included several other deoxycholic acid presentations including long-term follow-up from phase II/III trials showing that improvements in SMF severity are maintained for up to 4 years after treatment. The improvements were due to deoxycholic acid treatment, as body weight did not significantly change throughout the follow-up period, said study author Dr. Ashish Bhatia of the DuPage Medical Group, in Naperville, Ill.
Dr. Kenneth Beer of Palm Beach (Fla.) Cosmetic, provided details on the ongoing Kythera-sponsored CONTOUR: Condition of Submental Fullness and Treatment Outcomes Registry study looking at how SMF is treated in clinical practice and the risks and benefits associated with treatment.
Kythera Biopharmaceuticals markets Kybella, which is also known as ATX-101. Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera. Several coauthors also disclosed ties to the company.
AT THE ASDS ANNUAL MEETING
Key clinical point: Deoxycholic acid injection reduces submental fat in patients with mild or extreme submental fullness.
Major finding: Submental fat improved by two grades in 43% of patients treated with deoxycholic acid vs. 0% given placebo.
Data source: A double-blind, phase III safety study comparing Kybella to placebo in 93 patients with mild or extreme submental fat.
Disclosures: Dr. Glogau, Dr. Roberts, Dr. Bhatia, and Dr. Beer reported ties to Kythera Biopharmaceuticals. Several coauthors also disclosed ties to Kythera.
Spitzoid melanoma mortality on par with conventional melanoma
CHICAGO – One in four patients with an invasive spitzoid melanoma died from melanoma within 10 years of diagnosis, according to a large SEER database analysis.
The risk of death due to melanoma increased significantly with tumor thickness, metastatic disease, head and neck lesions, male sex, and older age, Dr. Sultan Mirza reported at the annual meeting of the American Society for Dermatologic Surgery.
Spitzoid tumors represent a group of melanocytic neoplasms composed of distinct epithelioid and/or spindle cells and are important because of their mimicry of malignant melanoma.
Although there is a paucity of data, several smaller studies have suggested spitzoid melanomas are less aggressive and have a lower mortality rate when compared with conventional malignant melanoma, he said.
“Our study found spitzoid melanoma–specific mortality to be quite high and is likely to be more on par with the mortality of the conventional malignant melanoma,” Dr. Mirza of Mayo Clinic, Rochester, Minn., said in an interview.
“Given a lack of broadly accepted and well-defined diagnostic criteria, it is our suspicion that many cases of these tumors go unrecognized or are classified under various other types of neoplastic proliferations at the time of diagnosis. This, therefore, hinders our knowledge of the true prognosis of the spitzoid tumors.”
Using the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) database, the investigators identified 2,025 patients who were diagnosed between 1992 and 2010 with an epithelioid/spindle cell melanoma, epithelial cell melanoma, spindle cell melanoma not otherwise specified, or spindle cell melanoma type A or type B. After excluding patients with missing data including microscopic confirmation of malignancy or cause of death, 1,997 patients remained.
Most were white (96%), male (61%), and had invasive disease (98%). Their average age at diagnosis was 64 years, with 21 patients younger than 18 years of age. Median follow-up was 5.6 years.
Of the 1,997 patients, 773 (39%) were deceased at last follow-up. Of these, 331 (43%) died due to metastatic melanoma, Dr. Mirza said. The median time to death was 1.8 years after diagnosis.
Among the 1,956 patients with invasive disease, melanoma cause-specific survival at years 1, 5, 10, and 15 was 95%, 81%, 76%, and 74%, respectively.
Among 41 patients with in situ spitzoid melanoma, the melanoma cause-specific survival was 100% at years 1, 5, and 10.In survival analyses, a Breslow tumor depth of more than 4 mm carried a five times higher risk of melanoma-specific death than a depth of less than 1 mm (hazard ratio, 5.0; P less than .001), Dr. Mirza said.
The risk of death from melanoma increased dramatically as the stage of melanoma advanced from localized (referent) to regional (HR, 4.3; P = .001) and then to distant (HR, 19.4; P = .001).
A similar pattern was observed as patient age increased from 52 years or younger (referent) to 53-66 years (HR, 1.7; P = .001), 67- 77 years (HR, 1.7; P = .001), and finally to age 78 years and older (HR, 2.6; P = .001).
Men were twice as likely to die from melanoma as women (HR, 1.9; P = .001), he said.
The worst anatomic site for a lesion was on the head and scalp, which carried more than twice the risk of melanoma-specific death as lesions on the face and ears (HR, 2.3; P = .001).Limitations of the study were the lack of fluorescence in situ hybridization data, an inability to review and categorize tumor pathology, and confusing terminology regarding spitzoid tumors in the database, resulting in possible inclusion of other types of melanomas, Dr. Mirza said.
This variance of terminology emphasizes the need for standardized nomenclature and once accomplished, will hopefully provide further clarity regarding types of spitzoid growths, so we can know the true prognosis and treatment, he added.
CHICAGO – One in four patients with an invasive spitzoid melanoma died from melanoma within 10 years of diagnosis, according to a large SEER database analysis.
The risk of death due to melanoma increased significantly with tumor thickness, metastatic disease, head and neck lesions, male sex, and older age, Dr. Sultan Mirza reported at the annual meeting of the American Society for Dermatologic Surgery.
Spitzoid tumors represent a group of melanocytic neoplasms composed of distinct epithelioid and/or spindle cells and are important because of their mimicry of malignant melanoma.
Although there is a paucity of data, several smaller studies have suggested spitzoid melanomas are less aggressive and have a lower mortality rate when compared with conventional malignant melanoma, he said.
“Our study found spitzoid melanoma–specific mortality to be quite high and is likely to be more on par with the mortality of the conventional malignant melanoma,” Dr. Mirza of Mayo Clinic, Rochester, Minn., said in an interview.
“Given a lack of broadly accepted and well-defined diagnostic criteria, it is our suspicion that many cases of these tumors go unrecognized or are classified under various other types of neoplastic proliferations at the time of diagnosis. This, therefore, hinders our knowledge of the true prognosis of the spitzoid tumors.”
Using the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) database, the investigators identified 2,025 patients who were diagnosed between 1992 and 2010 with an epithelioid/spindle cell melanoma, epithelial cell melanoma, spindle cell melanoma not otherwise specified, or spindle cell melanoma type A or type B. After excluding patients with missing data including microscopic confirmation of malignancy or cause of death, 1,997 patients remained.
Most were white (96%), male (61%), and had invasive disease (98%). Their average age at diagnosis was 64 years, with 21 patients younger than 18 years of age. Median follow-up was 5.6 years.
Of the 1,997 patients, 773 (39%) were deceased at last follow-up. Of these, 331 (43%) died due to metastatic melanoma, Dr. Mirza said. The median time to death was 1.8 years after diagnosis.
Among the 1,956 patients with invasive disease, melanoma cause-specific survival at years 1, 5, 10, and 15 was 95%, 81%, 76%, and 74%, respectively.
Among 41 patients with in situ spitzoid melanoma, the melanoma cause-specific survival was 100% at years 1, 5, and 10.In survival analyses, a Breslow tumor depth of more than 4 mm carried a five times higher risk of melanoma-specific death than a depth of less than 1 mm (hazard ratio, 5.0; P less than .001), Dr. Mirza said.
The risk of death from melanoma increased dramatically as the stage of melanoma advanced from localized (referent) to regional (HR, 4.3; P = .001) and then to distant (HR, 19.4; P = .001).
A similar pattern was observed as patient age increased from 52 years or younger (referent) to 53-66 years (HR, 1.7; P = .001), 67- 77 years (HR, 1.7; P = .001), and finally to age 78 years and older (HR, 2.6; P = .001).
Men were twice as likely to die from melanoma as women (HR, 1.9; P = .001), he said.
The worst anatomic site for a lesion was on the head and scalp, which carried more than twice the risk of melanoma-specific death as lesions on the face and ears (HR, 2.3; P = .001).Limitations of the study were the lack of fluorescence in situ hybridization data, an inability to review and categorize tumor pathology, and confusing terminology regarding spitzoid tumors in the database, resulting in possible inclusion of other types of melanomas, Dr. Mirza said.
This variance of terminology emphasizes the need for standardized nomenclature and once accomplished, will hopefully provide further clarity regarding types of spitzoid growths, so we can know the true prognosis and treatment, he added.
CHICAGO – One in four patients with an invasive spitzoid melanoma died from melanoma within 10 years of diagnosis, according to a large SEER database analysis.
The risk of death due to melanoma increased significantly with tumor thickness, metastatic disease, head and neck lesions, male sex, and older age, Dr. Sultan Mirza reported at the annual meeting of the American Society for Dermatologic Surgery.
Spitzoid tumors represent a group of melanocytic neoplasms composed of distinct epithelioid and/or spindle cells and are important because of their mimicry of malignant melanoma.
Although there is a paucity of data, several smaller studies have suggested spitzoid melanomas are less aggressive and have a lower mortality rate when compared with conventional malignant melanoma, he said.
“Our study found spitzoid melanoma–specific mortality to be quite high and is likely to be more on par with the mortality of the conventional malignant melanoma,” Dr. Mirza of Mayo Clinic, Rochester, Minn., said in an interview.
“Given a lack of broadly accepted and well-defined diagnostic criteria, it is our suspicion that many cases of these tumors go unrecognized or are classified under various other types of neoplastic proliferations at the time of diagnosis. This, therefore, hinders our knowledge of the true prognosis of the spitzoid tumors.”
Using the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) database, the investigators identified 2,025 patients who were diagnosed between 1992 and 2010 with an epithelioid/spindle cell melanoma, epithelial cell melanoma, spindle cell melanoma not otherwise specified, or spindle cell melanoma type A or type B. After excluding patients with missing data including microscopic confirmation of malignancy or cause of death, 1,997 patients remained.
Most were white (96%), male (61%), and had invasive disease (98%). Their average age at diagnosis was 64 years, with 21 patients younger than 18 years of age. Median follow-up was 5.6 years.
Of the 1,997 patients, 773 (39%) were deceased at last follow-up. Of these, 331 (43%) died due to metastatic melanoma, Dr. Mirza said. The median time to death was 1.8 years after diagnosis.
Among the 1,956 patients with invasive disease, melanoma cause-specific survival at years 1, 5, 10, and 15 was 95%, 81%, 76%, and 74%, respectively.
Among 41 patients with in situ spitzoid melanoma, the melanoma cause-specific survival was 100% at years 1, 5, and 10.In survival analyses, a Breslow tumor depth of more than 4 mm carried a five times higher risk of melanoma-specific death than a depth of less than 1 mm (hazard ratio, 5.0; P less than .001), Dr. Mirza said.
The risk of death from melanoma increased dramatically as the stage of melanoma advanced from localized (referent) to regional (HR, 4.3; P = .001) and then to distant (HR, 19.4; P = .001).
A similar pattern was observed as patient age increased from 52 years or younger (referent) to 53-66 years (HR, 1.7; P = .001), 67- 77 years (HR, 1.7; P = .001), and finally to age 78 years and older (HR, 2.6; P = .001).
Men were twice as likely to die from melanoma as women (HR, 1.9; P = .001), he said.
The worst anatomic site for a lesion was on the head and scalp, which carried more than twice the risk of melanoma-specific death as lesions on the face and ears (HR, 2.3; P = .001).Limitations of the study were the lack of fluorescence in situ hybridization data, an inability to review and categorize tumor pathology, and confusing terminology regarding spitzoid tumors in the database, resulting in possible inclusion of other types of melanomas, Dr. Mirza said.
This variance of terminology emphasizes the need for standardized nomenclature and once accomplished, will hopefully provide further clarity regarding types of spitzoid growths, so we can know the true prognosis and treatment, he added.
AT THE ASDS ANNUAL MEETING
Key clinical point: One-fourth of patients with invasive spitzoid melanoma died from their disease within 10 years of diagnosis.
Major finding: Melanoma-specific mortality was 24% at 10 years.
Data source: SEER database analysis of 1,997 patients with Spitz cutaneous melanoma.
Disclosures: The authors reported having no financial disclosures.