User login
KD025 shows promise for steroid-dependent cGVHD
SALT LAKE CITY – KD025, an orally available Rho-associated coiled-coil kinase 2–selective inhibitor, is demonstrating encouraging activity and safety in patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2a clinical trial.
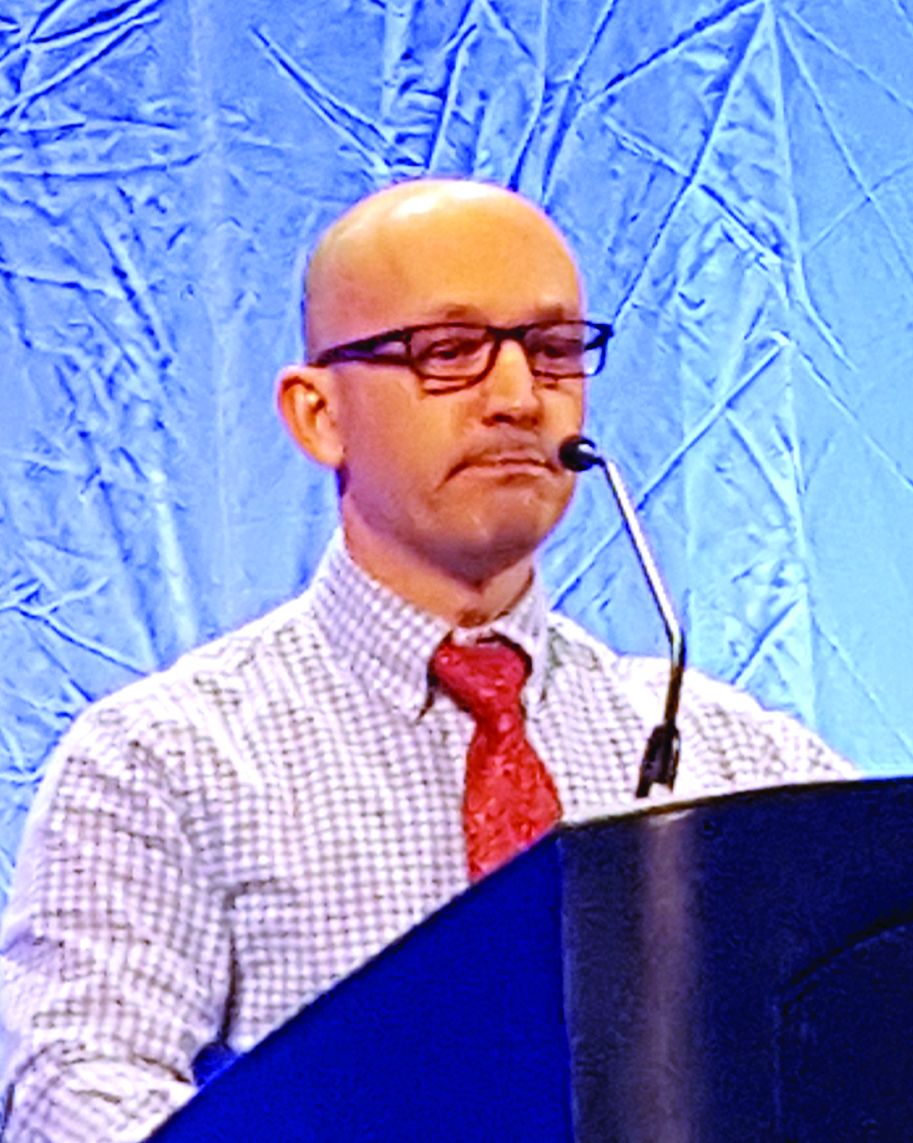
Initial results from the ongoing open-label trial known as KD025-208 showed that 11 of 17 patients (65%) and 11 of 16 patients (69%) enrolled in 200-mg daily and 200-mg twice-daily dose cohorts, respectively, had a clinical response with no reported treatment-related serious adverse events at any evaluation time point, Aleksandr Lazaryan, MD, PhD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The median duration of treatment in the 200-mg daily group (cohort 1) was 37 weeks, and in the 200-mg twice-daily group (cohort 2) was 28 weeks. At last follow-up, eight patients remained active in each cohort, and these patients had a median treatment duration of 53 and 38 weeks, respectively, he said.
In cohort 1, four patients went off the study because of cGVHD progression, and five withdrew, including two who experienced recurrence of their underlying hematologic malignancy. In cohort 2, 7 of the 16 patients experienced progression of cGVHD, he noted.
Patients in cohorts 1 and 2 had a median age of 52 years and had received at least 2 months of steroid treatment and no more than 3 prior lines of therapy. They were comparable with respect to baseline characteristics, including median time to and duration of GVHD, time from diagnosis to enrollment, median prednisone dose, and median number of prior therapies. They had involvement of various – and often multiple – organ systems: 58% had four or more systems affected at the time of enrollment, and 21% had five or more systems affected.
“This, in a way, reflects a real-life mix of the cGVHD population of patients, with some of those patients having advanced cGVHD,” said Dr. Lazaryan.
Responses were observed across all affected organ systems, with complete responses documented in the upper and lower gastrointestinal tracts. About 75% of patients in cohort 1 who had multiple organ systems involved at enrollment demonstrated responses in at least four organ systems.
Furthermore, the responses were rapid: 68% of responses occurred in the first 8 weeks of treatment and appeared durable, Dr. Lazaryan said, noting that 7 of the 17 patients in cohort 1 had sustained responses for more than 20 weeks, and 3 patients had sustained responses for more than 32 weeks.
“The durability data continue to mature in this trial,” he added.
The adverse events that occurred were consistent with what would be expected for the cGVHD patient population treated with steroids, he said, reporting that no patients discontinued treatment because of infection, no opportunistic or fungal infections have been reported to date, and no treatment-related serious adverse events were reported.
Steroid dose reductions were experienced by 40% and 26% of patients in cohorts 1 and 2, respectively. The dose reductions were achieved in both KD025 responders and nonresponders, he noted.
Overall, four patients (12%) were able to discontinue steroids, and 80% in both cohorts experienced reductions in background tacrolimus.
In addition, up to 65% of patients in cohort 1 achieved a greater than seven point reduction on the Lee cGVHD Symptom Scale, with both responders and nonresponders experiencing improvement on this endpoint.
Chronic GVHD remains a leading cause of post-transplant morbidity and mortality. KD025, which is currently in phase 2 development for inflammatory fibrotic disease, has been shown in preclinical models to down-regulate T helper 17 cells and T follicular helper cells while up-regulating anti-inflammatory regulatory T cells, thereby potentially correcting the immunological imbalance seen in cGVHD, Dr. Lazaryan said.
Analysis is ongoing in this study, including in a third cohort of patients treated with 200 mg of KD025 four times daily, which recently completed accrual. An expansion cohort, at a dose yet to be determined, will include approximately 40 patients, he noted.
The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
sworcester@frontlinemedcom.com
SOURCE: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
SALT LAKE CITY – KD025, an orally available Rho-associated coiled-coil kinase 2–selective inhibitor, is demonstrating encouraging activity and safety in patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2a clinical trial.
Initial results from the ongoing open-label trial known as KD025-208 showed that 11 of 17 patients (65%) and 11 of 16 patients (69%) enrolled in 200-mg daily and 200-mg twice-daily dose cohorts, respectively, had a clinical response with no reported treatment-related serious adverse events at any evaluation time point, Aleksandr Lazaryan, MD, PhD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The median duration of treatment in the 200-mg daily group (cohort 1) was 37 weeks, and in the 200-mg twice-daily group (cohort 2) was 28 weeks. At last follow-up, eight patients remained active in each cohort, and these patients had a median treatment duration of 53 and 38 weeks, respectively, he said.
In cohort 1, four patients went off the study because of cGVHD progression, and five withdrew, including two who experienced recurrence of their underlying hematologic malignancy. In cohort 2, 7 of the 16 patients experienced progression of cGVHD, he noted.
Patients in cohorts 1 and 2 had a median age of 52 years and had received at least 2 months of steroid treatment and no more than 3 prior lines of therapy. They were comparable with respect to baseline characteristics, including median time to and duration of GVHD, time from diagnosis to enrollment, median prednisone dose, and median number of prior therapies. They had involvement of various – and often multiple – organ systems: 58% had four or more systems affected at the time of enrollment, and 21% had five or more systems affected.
“This, in a way, reflects a real-life mix of the cGVHD population of patients, with some of those patients having advanced cGVHD,” said Dr. Lazaryan.
Responses were observed across all affected organ systems, with complete responses documented in the upper and lower gastrointestinal tracts. About 75% of patients in cohort 1 who had multiple organ systems involved at enrollment demonstrated responses in at least four organ systems.
Furthermore, the responses were rapid: 68% of responses occurred in the first 8 weeks of treatment and appeared durable, Dr. Lazaryan said, noting that 7 of the 17 patients in cohort 1 had sustained responses for more than 20 weeks, and 3 patients had sustained responses for more than 32 weeks.
“The durability data continue to mature in this trial,” he added.
The adverse events that occurred were consistent with what would be expected for the cGVHD patient population treated with steroids, he said, reporting that no patients discontinued treatment because of infection, no opportunistic or fungal infections have been reported to date, and no treatment-related serious adverse events were reported.
Steroid dose reductions were experienced by 40% and 26% of patients in cohorts 1 and 2, respectively. The dose reductions were achieved in both KD025 responders and nonresponders, he noted.
Overall, four patients (12%) were able to discontinue steroids, and 80% in both cohorts experienced reductions in background tacrolimus.
In addition, up to 65% of patients in cohort 1 achieved a greater than seven point reduction on the Lee cGVHD Symptom Scale, with both responders and nonresponders experiencing improvement on this endpoint.
Chronic GVHD remains a leading cause of post-transplant morbidity and mortality. KD025, which is currently in phase 2 development for inflammatory fibrotic disease, has been shown in preclinical models to down-regulate T helper 17 cells and T follicular helper cells while up-regulating anti-inflammatory regulatory T cells, thereby potentially correcting the immunological imbalance seen in cGVHD, Dr. Lazaryan said.
Analysis is ongoing in this study, including in a third cohort of patients treated with 200 mg of KD025 four times daily, which recently completed accrual. An expansion cohort, at a dose yet to be determined, will include approximately 40 patients, he noted.
The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
sworcester@frontlinemedcom.com
SOURCE: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
SALT LAKE CITY – KD025, an orally available Rho-associated coiled-coil kinase 2–selective inhibitor, is demonstrating encouraging activity and safety in patients with steroid-dependent or refractory chronic graft-versus-host disease (cGVHD) in a phase 2a clinical trial.
Initial results from the ongoing open-label trial known as KD025-208 showed that 11 of 17 patients (65%) and 11 of 16 patients (69%) enrolled in 200-mg daily and 200-mg twice-daily dose cohorts, respectively, had a clinical response with no reported treatment-related serious adverse events at any evaluation time point, Aleksandr Lazaryan, MD, PhD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The median duration of treatment in the 200-mg daily group (cohort 1) was 37 weeks, and in the 200-mg twice-daily group (cohort 2) was 28 weeks. At last follow-up, eight patients remained active in each cohort, and these patients had a median treatment duration of 53 and 38 weeks, respectively, he said.
In cohort 1, four patients went off the study because of cGVHD progression, and five withdrew, including two who experienced recurrence of their underlying hematologic malignancy. In cohort 2, 7 of the 16 patients experienced progression of cGVHD, he noted.
Patients in cohorts 1 and 2 had a median age of 52 years and had received at least 2 months of steroid treatment and no more than 3 prior lines of therapy. They were comparable with respect to baseline characteristics, including median time to and duration of GVHD, time from diagnosis to enrollment, median prednisone dose, and median number of prior therapies. They had involvement of various – and often multiple – organ systems: 58% had four or more systems affected at the time of enrollment, and 21% had five or more systems affected.
“This, in a way, reflects a real-life mix of the cGVHD population of patients, with some of those patients having advanced cGVHD,” said Dr. Lazaryan.
Responses were observed across all affected organ systems, with complete responses documented in the upper and lower gastrointestinal tracts. About 75% of patients in cohort 1 who had multiple organ systems involved at enrollment demonstrated responses in at least four organ systems.
Furthermore, the responses were rapid: 68% of responses occurred in the first 8 weeks of treatment and appeared durable, Dr. Lazaryan said, noting that 7 of the 17 patients in cohort 1 had sustained responses for more than 20 weeks, and 3 patients had sustained responses for more than 32 weeks.
“The durability data continue to mature in this trial,” he added.
The adverse events that occurred were consistent with what would be expected for the cGVHD patient population treated with steroids, he said, reporting that no patients discontinued treatment because of infection, no opportunistic or fungal infections have been reported to date, and no treatment-related serious adverse events were reported.
Steroid dose reductions were experienced by 40% and 26% of patients in cohorts 1 and 2, respectively. The dose reductions were achieved in both KD025 responders and nonresponders, he noted.
Overall, four patients (12%) were able to discontinue steroids, and 80% in both cohorts experienced reductions in background tacrolimus.
In addition, up to 65% of patients in cohort 1 achieved a greater than seven point reduction on the Lee cGVHD Symptom Scale, with both responders and nonresponders experiencing improvement on this endpoint.
Chronic GVHD remains a leading cause of post-transplant morbidity and mortality. KD025, which is currently in phase 2 development for inflammatory fibrotic disease, has been shown in preclinical models to down-regulate T helper 17 cells and T follicular helper cells while up-regulating anti-inflammatory regulatory T cells, thereby potentially correcting the immunological imbalance seen in cGVHD, Dr. Lazaryan said.
Analysis is ongoing in this study, including in a third cohort of patients treated with 200 mg of KD025 four times daily, which recently completed accrual. An expansion cohort, at a dose yet to be determined, will include approximately 40 patients, he noted.
The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
sworcester@frontlinemedcom.com
SOURCE: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Clinical response rates in cohorts 1 and 2 were 65% and 69%, respectively.
Study details: Preliminary findings in 33 patients from a phase 2a trial.
Disclosures: The trial is sponsored by Kadmon. Dr. Lazaryan reported advisory board membership and consultancy for GLyPharma Therapeutic.
Source: Lazaryan A et al. 2018 BMT Tandem Meetings, Abstract 38.
Nonmyeloablative conditioning gets a radiation boost for severe hemoglobinopathies
SALT LAKE CITY – A nonmyeloablative conditioning regimen with a boosted dose of total body irradiation yielded success for a cohort of patients with severe hemoglobinopathy and haploidentical donors.
Of 17 patients with severe sickle cell disease or beta-thalassemia who received allogeneic bone marrow transplants, all but one had successful engraftment, and 13 have achieved full donor chimerism, said Javier Bolaños-Meade, MD.
“Cure of severe hemoglobinopathies is now possible for most patients,” said Dr. Bolaños-Meade. “It should no longer be considered as available to only a fraction of such patients,” such as those who come with a fully-matched donor and those able to tolerate myeloablative conditioning, he said.
Of the patients who received bone marrow transplants, five patients have stopped immunosuppressive therapy, and all patients are alive, having been followed for a median of 15 months (range, 3-34 months).
The rate of graft versus host disease (GVHD) was low: Two patients developed grade 2 acute GVHD, and one patient developed grade 3 acute GVHD; another three patients had mild to moderate chronic GVHD, but all GVHD has resolved, said Dr. Bolaños-Meade.
Historically, the difficulties with transplant in this population were numerous. “No. 1, it’s very difficult to find an HLA-matched donor,” said Dr. Bolaños-Meade. Also, since there’s no target for graft-versus-tumor effect post-transplant, any amount of chronic GVHD is also high on the list of concerns when considering a transplant for hemoglobinopathy.
“The other problem in this group of patients is their ability to tolerate myeloablation,” he said. The accumulated burden of disease, as well as sequelae of transfusion dependence for some, may make a myeloablative regime too risky.
Dr. Bolaños-Meade said that he and his collaborators at Johns Hopkins University, Baltimore, wanted to be able to address all of these concerns in one regimen. “We were trying to work out a system that may be able to solve all the problems – to use nonmyeloablation and to use whatever donor is available.”
His research group had previously shown that nonmyeloablative transplants were well tolerated in patients with sickle cell disease and that haploidentical donors could be used (Blood. 2012 Nov 22;120[22]:4285-91). “However, we had a very high incidence of graft failure,” Dr. Bolaños-Meade said.
A strategy to increase the engraftment rate while still limiting toxicity, he said, would be to increase the dose of total body irradiation used in the conditioning regimen, from 200 to 400 centigray (cGy); this higher dose was incorporated into the study protocol.
Patients were enrolled if they had severe sickle cell disease (SCD; n = 12) or beta-thalassemia (n = 5).
To enroll in the study, SCD patients had to have been hospitalized at least twice a year in the preceding 2 years. The patients with SCD were a median 26 years of age (range, 6-31 years); four were male, and eight were female. Three of the SCD patients were transfusion dependent, and several had such serious complications as osteonecrosis, brain changes seen in medical imaging, and acute coronary syndrome.
The beta-thalassemia patients were a median 7 years of age (range, 6-16 years); all but one were female, and all had been transfusion dependent since infancy.
Bone marrow donors were not all first degree relatives: There were five mothers, four fathers, four brothers, and three sisters, but also an aunt. Two pairs had major ABO incompatibility, and five had minor ABO incompatibility. Ten were ABO compatible.
The conditioning regimen for all patients involved rabbit antithymocyte globulin, fludarabine, and cyclophosphamide, and then total body irradiation given the day before transplant.
After transplant, in addition to standard supportive care, patients received cyclophosphamide on days 3 and 4. Beginning on day 5, patients received mycophenolate mofetil through day 35 and sirolimus for 1 full year after transplant.
The antithymocyte globulin induced sickle cell crises in all SCD patients, and one patient developed sirolimus-induced diabetes. One other patient had a worsening of Meniere disease, and another patient developed BK virus cystitis.
Breaking down outcomes by disease type, Dr. Bolaños-Meade said that the one engraftment failure occurred in an SCD patient. Of the remaining 11 engrafted patients, 9 have full donor chimerism, and all but 1 of the 11 are transfusion independent now. The patient who remains transfusion dependent has mixed chimerism and received bone marrow from a donor with major ABO mismatch. Although one of the five beta-thalassemia patients also has mixed chimerism, all are now transfusion independent.
The boost in hemoglobin post-transplant was relatively modest for the beta-thalassemia group, from a median 9.5 to 10.1 g/dL at the most recent visit. However, the pretransplant levels were boosted by transfusions for all patients in this group, Dr. Bolaños-Meade pointed out.
The SCD patients saw their hemoglobin go from a median 8.65 to 11.4 g/dL (P = .001). Median bilirubin for this group dropped from 2.4 to 0.2 mg/dL (P = .002) with the cessation of sickling-related hemolysis; significant improvements were also seen in absolute reticulocyte counts and lactate dehydrogenase levels.
Dr. Bolaños-Meade reported that he is on the data safety monitoring board of Incyte.
SOURCE: Bolaños-Meade J et al. BMT Tandem Meetings, Abstract LBA-3.
SALT LAKE CITY – A nonmyeloablative conditioning regimen with a boosted dose of total body irradiation yielded success for a cohort of patients with severe hemoglobinopathy and haploidentical donors.
Of 17 patients with severe sickle cell disease or beta-thalassemia who received allogeneic bone marrow transplants, all but one had successful engraftment, and 13 have achieved full donor chimerism, said Javier Bolaños-Meade, MD.
“Cure of severe hemoglobinopathies is now possible for most patients,” said Dr. Bolaños-Meade. “It should no longer be considered as available to only a fraction of such patients,” such as those who come with a fully-matched donor and those able to tolerate myeloablative conditioning, he said.
Of the patients who received bone marrow transplants, five patients have stopped immunosuppressive therapy, and all patients are alive, having been followed for a median of 15 months (range, 3-34 months).
The rate of graft versus host disease (GVHD) was low: Two patients developed grade 2 acute GVHD, and one patient developed grade 3 acute GVHD; another three patients had mild to moderate chronic GVHD, but all GVHD has resolved, said Dr. Bolaños-Meade.
Historically, the difficulties with transplant in this population were numerous. “No. 1, it’s very difficult to find an HLA-matched donor,” said Dr. Bolaños-Meade. Also, since there’s no target for graft-versus-tumor effect post-transplant, any amount of chronic GVHD is also high on the list of concerns when considering a transplant for hemoglobinopathy.
“The other problem in this group of patients is their ability to tolerate myeloablation,” he said. The accumulated burden of disease, as well as sequelae of transfusion dependence for some, may make a myeloablative regime too risky.
Dr. Bolaños-Meade said that he and his collaborators at Johns Hopkins University, Baltimore, wanted to be able to address all of these concerns in one regimen. “We were trying to work out a system that may be able to solve all the problems – to use nonmyeloablation and to use whatever donor is available.”
His research group had previously shown that nonmyeloablative transplants were well tolerated in patients with sickle cell disease and that haploidentical donors could be used (Blood. 2012 Nov 22;120[22]:4285-91). “However, we had a very high incidence of graft failure,” Dr. Bolaños-Meade said.
A strategy to increase the engraftment rate while still limiting toxicity, he said, would be to increase the dose of total body irradiation used in the conditioning regimen, from 200 to 400 centigray (cGy); this higher dose was incorporated into the study protocol.
Patients were enrolled if they had severe sickle cell disease (SCD; n = 12) or beta-thalassemia (n = 5).
To enroll in the study, SCD patients had to have been hospitalized at least twice a year in the preceding 2 years. The patients with SCD were a median 26 years of age (range, 6-31 years); four were male, and eight were female. Three of the SCD patients were transfusion dependent, and several had such serious complications as osteonecrosis, brain changes seen in medical imaging, and acute coronary syndrome.
The beta-thalassemia patients were a median 7 years of age (range, 6-16 years); all but one were female, and all had been transfusion dependent since infancy.
Bone marrow donors were not all first degree relatives: There were five mothers, four fathers, four brothers, and three sisters, but also an aunt. Two pairs had major ABO incompatibility, and five had minor ABO incompatibility. Ten were ABO compatible.
The conditioning regimen for all patients involved rabbit antithymocyte globulin, fludarabine, and cyclophosphamide, and then total body irradiation given the day before transplant.
After transplant, in addition to standard supportive care, patients received cyclophosphamide on days 3 and 4. Beginning on day 5, patients received mycophenolate mofetil through day 35 and sirolimus for 1 full year after transplant.
The antithymocyte globulin induced sickle cell crises in all SCD patients, and one patient developed sirolimus-induced diabetes. One other patient had a worsening of Meniere disease, and another patient developed BK virus cystitis.
Breaking down outcomes by disease type, Dr. Bolaños-Meade said that the one engraftment failure occurred in an SCD patient. Of the remaining 11 engrafted patients, 9 have full donor chimerism, and all but 1 of the 11 are transfusion independent now. The patient who remains transfusion dependent has mixed chimerism and received bone marrow from a donor with major ABO mismatch. Although one of the five beta-thalassemia patients also has mixed chimerism, all are now transfusion independent.
The boost in hemoglobin post-transplant was relatively modest for the beta-thalassemia group, from a median 9.5 to 10.1 g/dL at the most recent visit. However, the pretransplant levels were boosted by transfusions for all patients in this group, Dr. Bolaños-Meade pointed out.
The SCD patients saw their hemoglobin go from a median 8.65 to 11.4 g/dL (P = .001). Median bilirubin for this group dropped from 2.4 to 0.2 mg/dL (P = .002) with the cessation of sickling-related hemolysis; significant improvements were also seen in absolute reticulocyte counts and lactate dehydrogenase levels.
Dr. Bolaños-Meade reported that he is on the data safety monitoring board of Incyte.
SOURCE: Bolaños-Meade J et al. BMT Tandem Meetings, Abstract LBA-3.
SALT LAKE CITY – A nonmyeloablative conditioning regimen with a boosted dose of total body irradiation yielded success for a cohort of patients with severe hemoglobinopathy and haploidentical donors.
Of 17 patients with severe sickle cell disease or beta-thalassemia who received allogeneic bone marrow transplants, all but one had successful engraftment, and 13 have achieved full donor chimerism, said Javier Bolaños-Meade, MD.
“Cure of severe hemoglobinopathies is now possible for most patients,” said Dr. Bolaños-Meade. “It should no longer be considered as available to only a fraction of such patients,” such as those who come with a fully-matched donor and those able to tolerate myeloablative conditioning, he said.
Of the patients who received bone marrow transplants, five patients have stopped immunosuppressive therapy, and all patients are alive, having been followed for a median of 15 months (range, 3-34 months).
The rate of graft versus host disease (GVHD) was low: Two patients developed grade 2 acute GVHD, and one patient developed grade 3 acute GVHD; another three patients had mild to moderate chronic GVHD, but all GVHD has resolved, said Dr. Bolaños-Meade.
Historically, the difficulties with transplant in this population were numerous. “No. 1, it’s very difficult to find an HLA-matched donor,” said Dr. Bolaños-Meade. Also, since there’s no target for graft-versus-tumor effect post-transplant, any amount of chronic GVHD is also high on the list of concerns when considering a transplant for hemoglobinopathy.
“The other problem in this group of patients is their ability to tolerate myeloablation,” he said. The accumulated burden of disease, as well as sequelae of transfusion dependence for some, may make a myeloablative regime too risky.
Dr. Bolaños-Meade said that he and his collaborators at Johns Hopkins University, Baltimore, wanted to be able to address all of these concerns in one regimen. “We were trying to work out a system that may be able to solve all the problems – to use nonmyeloablation and to use whatever donor is available.”
His research group had previously shown that nonmyeloablative transplants were well tolerated in patients with sickle cell disease and that haploidentical donors could be used (Blood. 2012 Nov 22;120[22]:4285-91). “However, we had a very high incidence of graft failure,” Dr. Bolaños-Meade said.
A strategy to increase the engraftment rate while still limiting toxicity, he said, would be to increase the dose of total body irradiation used in the conditioning regimen, from 200 to 400 centigray (cGy); this higher dose was incorporated into the study protocol.
Patients were enrolled if they had severe sickle cell disease (SCD; n = 12) or beta-thalassemia (n = 5).
To enroll in the study, SCD patients had to have been hospitalized at least twice a year in the preceding 2 years. The patients with SCD were a median 26 years of age (range, 6-31 years); four were male, and eight were female. Three of the SCD patients were transfusion dependent, and several had such serious complications as osteonecrosis, brain changes seen in medical imaging, and acute coronary syndrome.
The beta-thalassemia patients were a median 7 years of age (range, 6-16 years); all but one were female, and all had been transfusion dependent since infancy.
Bone marrow donors were not all first degree relatives: There were five mothers, four fathers, four brothers, and three sisters, but also an aunt. Two pairs had major ABO incompatibility, and five had minor ABO incompatibility. Ten were ABO compatible.
The conditioning regimen for all patients involved rabbit antithymocyte globulin, fludarabine, and cyclophosphamide, and then total body irradiation given the day before transplant.
After transplant, in addition to standard supportive care, patients received cyclophosphamide on days 3 and 4. Beginning on day 5, patients received mycophenolate mofetil through day 35 and sirolimus for 1 full year after transplant.
The antithymocyte globulin induced sickle cell crises in all SCD patients, and one patient developed sirolimus-induced diabetes. One other patient had a worsening of Meniere disease, and another patient developed BK virus cystitis.
Breaking down outcomes by disease type, Dr. Bolaños-Meade said that the one engraftment failure occurred in an SCD patient. Of the remaining 11 engrafted patients, 9 have full donor chimerism, and all but 1 of the 11 are transfusion independent now. The patient who remains transfusion dependent has mixed chimerism and received bone marrow from a donor with major ABO mismatch. Although one of the five beta-thalassemia patients also has mixed chimerism, all are now transfusion independent.
The boost in hemoglobin post-transplant was relatively modest for the beta-thalassemia group, from a median 9.5 to 10.1 g/dL at the most recent visit. However, the pretransplant levels were boosted by transfusions for all patients in this group, Dr. Bolaños-Meade pointed out.
The SCD patients saw their hemoglobin go from a median 8.65 to 11.4 g/dL (P = .001). Median bilirubin for this group dropped from 2.4 to 0.2 mg/dL (P = .002) with the cessation of sickling-related hemolysis; significant improvements were also seen in absolute reticulocyte counts and lactate dehydrogenase levels.
Dr. Bolaños-Meade reported that he is on the data safety monitoring board of Incyte.
SOURCE: Bolaños-Meade J et al. BMT Tandem Meetings, Abstract LBA-3.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Of the 17 patients who received haploidentical bone marrow transplant, 13 have achieved full chimerism.
Study details: Report of 17 consecutive patients with severe sickle cell disease or beta-thalassemia who received nonmyeloablative conditioning and bone marrow transplant from haploidentical donors.
Disclosures: Dr. Bolaños-Meade reported no outside sources of funding for the study. He is on the data safety monitoring board of Incyte.
Source: Bolaños-Meade J et al. 2018 BMT Tandem Meetings, Abstract LBA-3.
Outpatient CAR T infusions feasible using liso-cel
SALT LAKE CITY – A CD19-directed 4-1BB chimeric antigen receptor (CAR) T cell product showed efficacy and a low rate of cytokine release syndrome and neurotoxicity in patients with aggressive lymphomas and poor prognoses, raising the possibility of outpatient administration and fewer hospitalization days in this high-risk group.
A total of 86 patients who received inpatient infusions of lisocabtagene maraleucel (liso-cel, also known as JCAR017) had a mean 15.6 days of hospitalization, compared with 9.3 days for 8 outpatient recipients, said Jeremy Abramson, MD, speaking at a top abstracts session of the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
As of October 2017, eight patients had received liso-cel infusion as outpatients with at least 28 days of postinfusion data, Dr. Abramson said.
Although all but one required hospital admission, at a median of 5 days postinfusion (range, 4-22 days), there had been no intensive care unit admissions, and no outpatient recipients had experienced severe cytokine release syndrome (CRS) or neurotoxicity. All admitted patients presented with fever.
Among the study population, “Cytokine release syndrome was only seen in 35% of our entire dataset,” with neurologic toxicity seen in 19% of participants, Dr. Abramson said. “The majority of subjects had no CRS and no toxicity,” he said. Severe CRS occurred in 1% of the study population, and severe neurotoxicity in 12%. There were no deaths related to either complication.
Dr. Abramson reported these results from the TRANSCEND NHL 001 trial, a seamless design phase 1 pivotal trial of liso-cel enrolling patients with relapsed and refractory aggressive B cell non-Hodgkin lymphoma (NHL). Liso-cel delivers CD19-directed CD4 and CD8 CAR T cells in a 1:1 ratio, said Dr. Abramson, director of the lymphoma program at the Massachusetts General Hospital Cancer Center, Boston.
A total of 91 patients were randomized to one of the three dose-finding cohorts of the multicenter trial of liso-cel. One cohort received 5 x 107 cells in a single dose; a second cohort received the same number of cells but in two doses administered 14 days apart; the third cohort received a single dose of 1 x 108 cells.
The seamless trial design then moved to dose expansion, using the two single doses established in the dose-finding phase of the study. Ultimately, Dr. Abramson said, the third and pivotal diffuse large B-cell lymphoma (DLBCL) cohort received the higher single dose, since a dose-response relationship was seen in the earlier cohorts. No increase in cytokine release syndrome or neurotoxicity has been seen with the higher dose in patients evaluated to date.
Patients (median age, 61 years) were eligible to participate in the trial if they had relapsed or refractory DLBCL, primary mediastinal B-cell lymphoma, grade 3B follicular lymphoma, or mantle cell lymphoma. Patients with a failed prior allogeneic stem cell transplant or secondary central nervous system involvement were eligible, but all patients had to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2.
As the trial moved to the core pivotal phase, eligibility requirements shifted slightly to include patients with ECOG status 0 or 1, and lymphoma diagnoses narrowed to include only DLBCL not otherwise specified (NOS), transformed follicular lymphoma, and high-grade B-cell lymphoma with double- and triple-hit cytogenetics. The core group was nearing completion of accrual at the time of the presentation, which presented preliminary results from this phase of the trial.
Among the 88 evaluable patients in the initial population with DLBCL receiving any of three dose levels, the best overall response rate (ORR) was 74% (95% confidence interval, 63%-83%); 52% of these patients achieved complete response (CR; 95% CI, 41%-63%).
For patients receiving the higher dose of liso-cel, the ORR was 81% (95% CI, 62%-94%), with a 63% CR rate (95% CI, 42%-81%), bearing out the dose-response rate that had been seen earlier in the trial, Dr. Abramson said.
The median duration of response in all TRANSCEND patients was 9.2 months; the median duration of remission has not been reached, he said. “We see evidence of durable response at 3 months in all our high-risk subsets, and that includes double- and triple-hit lymphomas, double-expresser lymphomas, patients who’ve never achieved prior complete remission, and patients with refractory disease.”
“The overall results are similarly encouraging,” Dr. Abramson said, with 86% of all patients alive at 6 months. Among the complete responders, 94% are alive at the 6-month mark. “The median duration of complete responders has not been reached in this cohort,” he said.
These results are notable, Dr. Abramson said, since about 90% of study participants have at least one disease risk factor that would predict median overall survival of 3-6 months.
During the period after leukapheresis while the CAR T cells were in production, patients could have ongoing treatment, but received PET scans to confirm disease before continuing enrollment in the trial and receiving liso-cel. The time from apheresis to product release for the pivotal cohort is now under 21 days, he said.
The study was supported by Juno Therapeutics, which plans to market liso-cel. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
SOURCE: Abramson J et al. Abstract 5.
SALT LAKE CITY – A CD19-directed 4-1BB chimeric antigen receptor (CAR) T cell product showed efficacy and a low rate of cytokine release syndrome and neurotoxicity in patients with aggressive lymphomas and poor prognoses, raising the possibility of outpatient administration and fewer hospitalization days in this high-risk group.
A total of 86 patients who received inpatient infusions of lisocabtagene maraleucel (liso-cel, also known as JCAR017) had a mean 15.6 days of hospitalization, compared with 9.3 days for 8 outpatient recipients, said Jeremy Abramson, MD, speaking at a top abstracts session of the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
As of October 2017, eight patients had received liso-cel infusion as outpatients with at least 28 days of postinfusion data, Dr. Abramson said.
Although all but one required hospital admission, at a median of 5 days postinfusion (range, 4-22 days), there had been no intensive care unit admissions, and no outpatient recipients had experienced severe cytokine release syndrome (CRS) or neurotoxicity. All admitted patients presented with fever.
Among the study population, “Cytokine release syndrome was only seen in 35% of our entire dataset,” with neurologic toxicity seen in 19% of participants, Dr. Abramson said. “The majority of subjects had no CRS and no toxicity,” he said. Severe CRS occurred in 1% of the study population, and severe neurotoxicity in 12%. There were no deaths related to either complication.
Dr. Abramson reported these results from the TRANSCEND NHL 001 trial, a seamless design phase 1 pivotal trial of liso-cel enrolling patients with relapsed and refractory aggressive B cell non-Hodgkin lymphoma (NHL). Liso-cel delivers CD19-directed CD4 and CD8 CAR T cells in a 1:1 ratio, said Dr. Abramson, director of the lymphoma program at the Massachusetts General Hospital Cancer Center, Boston.
A total of 91 patients were randomized to one of the three dose-finding cohorts of the multicenter trial of liso-cel. One cohort received 5 x 107 cells in a single dose; a second cohort received the same number of cells but in two doses administered 14 days apart; the third cohort received a single dose of 1 x 108 cells.
The seamless trial design then moved to dose expansion, using the two single doses established in the dose-finding phase of the study. Ultimately, Dr. Abramson said, the third and pivotal diffuse large B-cell lymphoma (DLBCL) cohort received the higher single dose, since a dose-response relationship was seen in the earlier cohorts. No increase in cytokine release syndrome or neurotoxicity has been seen with the higher dose in patients evaluated to date.
Patients (median age, 61 years) were eligible to participate in the trial if they had relapsed or refractory DLBCL, primary mediastinal B-cell lymphoma, grade 3B follicular lymphoma, or mantle cell lymphoma. Patients with a failed prior allogeneic stem cell transplant or secondary central nervous system involvement were eligible, but all patients had to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2.
As the trial moved to the core pivotal phase, eligibility requirements shifted slightly to include patients with ECOG status 0 or 1, and lymphoma diagnoses narrowed to include only DLBCL not otherwise specified (NOS), transformed follicular lymphoma, and high-grade B-cell lymphoma with double- and triple-hit cytogenetics. The core group was nearing completion of accrual at the time of the presentation, which presented preliminary results from this phase of the trial.
Among the 88 evaluable patients in the initial population with DLBCL receiving any of three dose levels, the best overall response rate (ORR) was 74% (95% confidence interval, 63%-83%); 52% of these patients achieved complete response (CR; 95% CI, 41%-63%).
For patients receiving the higher dose of liso-cel, the ORR was 81% (95% CI, 62%-94%), with a 63% CR rate (95% CI, 42%-81%), bearing out the dose-response rate that had been seen earlier in the trial, Dr. Abramson said.
The median duration of response in all TRANSCEND patients was 9.2 months; the median duration of remission has not been reached, he said. “We see evidence of durable response at 3 months in all our high-risk subsets, and that includes double- and triple-hit lymphomas, double-expresser lymphomas, patients who’ve never achieved prior complete remission, and patients with refractory disease.”
“The overall results are similarly encouraging,” Dr. Abramson said, with 86% of all patients alive at 6 months. Among the complete responders, 94% are alive at the 6-month mark. “The median duration of complete responders has not been reached in this cohort,” he said.
These results are notable, Dr. Abramson said, since about 90% of study participants have at least one disease risk factor that would predict median overall survival of 3-6 months.
During the period after leukapheresis while the CAR T cells were in production, patients could have ongoing treatment, but received PET scans to confirm disease before continuing enrollment in the trial and receiving liso-cel. The time from apheresis to product release for the pivotal cohort is now under 21 days, he said.
The study was supported by Juno Therapeutics, which plans to market liso-cel. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
SOURCE: Abramson J et al. Abstract 5.
SALT LAKE CITY – A CD19-directed 4-1BB chimeric antigen receptor (CAR) T cell product showed efficacy and a low rate of cytokine release syndrome and neurotoxicity in patients with aggressive lymphomas and poor prognoses, raising the possibility of outpatient administration and fewer hospitalization days in this high-risk group.
A total of 86 patients who received inpatient infusions of lisocabtagene maraleucel (liso-cel, also known as JCAR017) had a mean 15.6 days of hospitalization, compared with 9.3 days for 8 outpatient recipients, said Jeremy Abramson, MD, speaking at a top abstracts session of the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
As of October 2017, eight patients had received liso-cel infusion as outpatients with at least 28 days of postinfusion data, Dr. Abramson said.
Although all but one required hospital admission, at a median of 5 days postinfusion (range, 4-22 days), there had been no intensive care unit admissions, and no outpatient recipients had experienced severe cytokine release syndrome (CRS) or neurotoxicity. All admitted patients presented with fever.
Among the study population, “Cytokine release syndrome was only seen in 35% of our entire dataset,” with neurologic toxicity seen in 19% of participants, Dr. Abramson said. “The majority of subjects had no CRS and no toxicity,” he said. Severe CRS occurred in 1% of the study population, and severe neurotoxicity in 12%. There were no deaths related to either complication.
Dr. Abramson reported these results from the TRANSCEND NHL 001 trial, a seamless design phase 1 pivotal trial of liso-cel enrolling patients with relapsed and refractory aggressive B cell non-Hodgkin lymphoma (NHL). Liso-cel delivers CD19-directed CD4 and CD8 CAR T cells in a 1:1 ratio, said Dr. Abramson, director of the lymphoma program at the Massachusetts General Hospital Cancer Center, Boston.
A total of 91 patients were randomized to one of the three dose-finding cohorts of the multicenter trial of liso-cel. One cohort received 5 x 107 cells in a single dose; a second cohort received the same number of cells but in two doses administered 14 days apart; the third cohort received a single dose of 1 x 108 cells.
The seamless trial design then moved to dose expansion, using the two single doses established in the dose-finding phase of the study. Ultimately, Dr. Abramson said, the third and pivotal diffuse large B-cell lymphoma (DLBCL) cohort received the higher single dose, since a dose-response relationship was seen in the earlier cohorts. No increase in cytokine release syndrome or neurotoxicity has been seen with the higher dose in patients evaluated to date.
Patients (median age, 61 years) were eligible to participate in the trial if they had relapsed or refractory DLBCL, primary mediastinal B-cell lymphoma, grade 3B follicular lymphoma, or mantle cell lymphoma. Patients with a failed prior allogeneic stem cell transplant or secondary central nervous system involvement were eligible, but all patients had to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2.
As the trial moved to the core pivotal phase, eligibility requirements shifted slightly to include patients with ECOG status 0 or 1, and lymphoma diagnoses narrowed to include only DLBCL not otherwise specified (NOS), transformed follicular lymphoma, and high-grade B-cell lymphoma with double- and triple-hit cytogenetics. The core group was nearing completion of accrual at the time of the presentation, which presented preliminary results from this phase of the trial.
Among the 88 evaluable patients in the initial population with DLBCL receiving any of three dose levels, the best overall response rate (ORR) was 74% (95% confidence interval, 63%-83%); 52% of these patients achieved complete response (CR; 95% CI, 41%-63%).
For patients receiving the higher dose of liso-cel, the ORR was 81% (95% CI, 62%-94%), with a 63% CR rate (95% CI, 42%-81%), bearing out the dose-response rate that had been seen earlier in the trial, Dr. Abramson said.
The median duration of response in all TRANSCEND patients was 9.2 months; the median duration of remission has not been reached, he said. “We see evidence of durable response at 3 months in all our high-risk subsets, and that includes double- and triple-hit lymphomas, double-expresser lymphomas, patients who’ve never achieved prior complete remission, and patients with refractory disease.”
“The overall results are similarly encouraging,” Dr. Abramson said, with 86% of all patients alive at 6 months. Among the complete responders, 94% are alive at the 6-month mark. “The median duration of complete responders has not been reached in this cohort,” he said.
These results are notable, Dr. Abramson said, since about 90% of study participants have at least one disease risk factor that would predict median overall survival of 3-6 months.
During the period after leukapheresis while the CAR T cells were in production, patients could have ongoing treatment, but received PET scans to confirm disease before continuing enrollment in the trial and receiving liso-cel. The time from apheresis to product release for the pivotal cohort is now under 21 days, he said.
The study was supported by Juno Therapeutics, which plans to market liso-cel. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
SOURCE: Abramson J et al. Abstract 5.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: High-risk lymphoma patients had more than 6 fewer inpatient days with outpatient CAR T infusion.
Study details: Seamless phase 1 trial initially evaluating 91 patients with relapsed/refractory diffuse large B cell lymphoma.
Disclosures: Juno Therapeutics sponsored the study. Dr. Abramson reported ties with Celgene, Gilead, Seattle Genetics, Novartis, and Genentech.
Source: Abramson J et al. Abstract 5.
High efficacy, no safety signals for herpes zoster vaccine post-HSCT
SALT LAKE CITY – A recently approved adjuvanted herpes zoster vaccine)(Shingrix) effectively and safely prevented herpes zoster in a population of patients with multiple myeloma and other hematologic malignancies who received autologous hematopoietic stem cell transplantation.
The use of recombinant varicella zoster virus glycoprotein E in combination with an adjuvant system gives immunosuppressed individuals who have received hematopoietic stem cell transplantation (HSCT) a safe option for prevention of herpes zoster (HZ), said Javier de la Serna, MD, PhD, speaking at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
Presenting the findings at a late-breaking abstract session, Dr. de la Serna said that for the 1,721 participants in a placebo-controlled multicenter trial who received both doses of the vaccine, the incidence of HZ for vaccine recipients was 3.0%, compared with 9.4% of placebo recipients, for a vaccine efficacy of 68.2% (95% confidence interval, 55.6-77.5; P less than 0.0001). These results met the study’s primary objective.
Postherpetic neuralgia (PHN) prevention efficacy – a secondary endpoint – was 89.3% for those receiving the vaccine (HZ/su); the incidence of PHN was 0.5% in the HZ/su study arm, compared with 4.9% for those who received placebo (95% CI, 22.5-99.8). The study also tracked other HZ complications as a secondary endpoint, finding efficacy of 77.8% (95% CI, 19.1–95.0). “The vaccine was highly efficacious in preventing all the secondary outcomes,” said Dr. de la Serna of the Hospital Universitario 12 de Octubre, Madrid.
The randomized, observer-blind phase 3 trial was conducted in 28 countries.Adults who received autologous HSCT were randomized 1:1 to receive HZ/su (n = 922) or placebo (n = 924) within 50-70 days of their transplant. Patients were excluded if they were expected to receive more than 6 months of anti–varicella zoster prophylaxis posttransplant, Dr. de la Serna said.
Participants received the first dose of HZ/su at the first study visit, and the second dose 30-60 days later. Patients were seen 1 month after the last vaccine dose, and then again at months 13 and 25, with telephone follow-up between the later visits. All participants were followed for at least 1 year, Dr. de la Serna said.
Episodes of HZ were confirmed by polymerase chain reaction assay, or, when samples were lacking or indeterminate, by agreement of at least three members of an ascertainment committee.
Of the two components of the HZ/su vaccine, glycoprotein E triggers both humoral immunity and activity of varicella zoster–specific CD4+ T cells; the adjuvant system – dubbed ASO1 – boosts immune response. The vaccine was approved by the Food and Drug Administration in October 2017 for use in adults aged 50 years and older.
In addition to the primary endpoint of vaccine efficacy in prevention of HZ cases during the study period, secondary objectives included monitoring vaccine reactogenicity and safety, and evaluating vaccine efficacy for the prevention of PHN and other complications of HZ.
Tertiary objectives included vaccine efficacy in preventing HZ during the first year posttransplant (vaccine efficacy 84.7%; 95% CI, 32.2-96.6), as well as efficacy in preventing hospitalizations related to HZ (vaccine efficacy 76.2%, 95% CI 61.1-86.0).
An exploratory analysis found vaccine efficacy of 71.8% for participants younger than 50 years (95% CI, 38.8 – 88.3). For patients aged 50 years and older, vaccine efficacy was 67.3% (95% CI, 52.6–77.9).
The safety of HZ/su was determined by analyzing data for all participants, but efficacy data included only those who received the second dose and did not develop HZ within a month of receiving the second vaccine dose.
In the efficacy group (n = 1,721), patients were mostly (n = 1,296) aged 50 years or older. Most patients (n = 937) received HSCT for multiple myeloma. Overall, participants were about 63% male, and 77% were of Caucasian/European ancestry.
Adverse events, solicited for the first 7 days after injections, were mostly mild and related to the local site pain and inflammation expected with an adjuvanted vaccine; HZ/su recipients also experienced more fatigue and muscle aches than did those receiving placebo. Median duration of symptoms was up to 3 days, with grade 3 events lasting up to 2 days.
Unsolicited and serious adverse events were similar between study arms, with a median safety follow-up period of 29 months. The investigators judged that no deaths were related to the vaccine, and there were no signals for increased rate of relapse or immune-mediated diseases.
The study was funded by GlaxoSmithKline; HZ/su(Shingrix) is marketed by GlaxoSmithKline. Dr. de la Serna reported being on the advisory board or receiving honoraria from multiple pharmaceutical companies.
SOURCE: de la Serna J et al. 2018 BMT Tandem Meetings, Abstract LBA2.
SALT LAKE CITY – A recently approved adjuvanted herpes zoster vaccine)(Shingrix) effectively and safely prevented herpes zoster in a population of patients with multiple myeloma and other hematologic malignancies who received autologous hematopoietic stem cell transplantation.
The use of recombinant varicella zoster virus glycoprotein E in combination with an adjuvant system gives immunosuppressed individuals who have received hematopoietic stem cell transplantation (HSCT) a safe option for prevention of herpes zoster (HZ), said Javier de la Serna, MD, PhD, speaking at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
Presenting the findings at a late-breaking abstract session, Dr. de la Serna said that for the 1,721 participants in a placebo-controlled multicenter trial who received both doses of the vaccine, the incidence of HZ for vaccine recipients was 3.0%, compared with 9.4% of placebo recipients, for a vaccine efficacy of 68.2% (95% confidence interval, 55.6-77.5; P less than 0.0001). These results met the study’s primary objective.
Postherpetic neuralgia (PHN) prevention efficacy – a secondary endpoint – was 89.3% for those receiving the vaccine (HZ/su); the incidence of PHN was 0.5% in the HZ/su study arm, compared with 4.9% for those who received placebo (95% CI, 22.5-99.8). The study also tracked other HZ complications as a secondary endpoint, finding efficacy of 77.8% (95% CI, 19.1–95.0). “The vaccine was highly efficacious in preventing all the secondary outcomes,” said Dr. de la Serna of the Hospital Universitario 12 de Octubre, Madrid.
The randomized, observer-blind phase 3 trial was conducted in 28 countries.Adults who received autologous HSCT were randomized 1:1 to receive HZ/su (n = 922) or placebo (n = 924) within 50-70 days of their transplant. Patients were excluded if they were expected to receive more than 6 months of anti–varicella zoster prophylaxis posttransplant, Dr. de la Serna said.
Participants received the first dose of HZ/su at the first study visit, and the second dose 30-60 days later. Patients were seen 1 month after the last vaccine dose, and then again at months 13 and 25, with telephone follow-up between the later visits. All participants were followed for at least 1 year, Dr. de la Serna said.
Episodes of HZ were confirmed by polymerase chain reaction assay, or, when samples were lacking or indeterminate, by agreement of at least three members of an ascertainment committee.
Of the two components of the HZ/su vaccine, glycoprotein E triggers both humoral immunity and activity of varicella zoster–specific CD4+ T cells; the adjuvant system – dubbed ASO1 – boosts immune response. The vaccine was approved by the Food and Drug Administration in October 2017 for use in adults aged 50 years and older.
In addition to the primary endpoint of vaccine efficacy in prevention of HZ cases during the study period, secondary objectives included monitoring vaccine reactogenicity and safety, and evaluating vaccine efficacy for the prevention of PHN and other complications of HZ.
Tertiary objectives included vaccine efficacy in preventing HZ during the first year posttransplant (vaccine efficacy 84.7%; 95% CI, 32.2-96.6), as well as efficacy in preventing hospitalizations related to HZ (vaccine efficacy 76.2%, 95% CI 61.1-86.0).
An exploratory analysis found vaccine efficacy of 71.8% for participants younger than 50 years (95% CI, 38.8 – 88.3). For patients aged 50 years and older, vaccine efficacy was 67.3% (95% CI, 52.6–77.9).
The safety of HZ/su was determined by analyzing data for all participants, but efficacy data included only those who received the second dose and did not develop HZ within a month of receiving the second vaccine dose.
In the efficacy group (n = 1,721), patients were mostly (n = 1,296) aged 50 years or older. Most patients (n = 937) received HSCT for multiple myeloma. Overall, participants were about 63% male, and 77% were of Caucasian/European ancestry.
Adverse events, solicited for the first 7 days after injections, were mostly mild and related to the local site pain and inflammation expected with an adjuvanted vaccine; HZ/su recipients also experienced more fatigue and muscle aches than did those receiving placebo. Median duration of symptoms was up to 3 days, with grade 3 events lasting up to 2 days.
Unsolicited and serious adverse events were similar between study arms, with a median safety follow-up period of 29 months. The investigators judged that no deaths were related to the vaccine, and there were no signals for increased rate of relapse or immune-mediated diseases.
The study was funded by GlaxoSmithKline; HZ/su(Shingrix) is marketed by GlaxoSmithKline. Dr. de la Serna reported being on the advisory board or receiving honoraria from multiple pharmaceutical companies.
SOURCE: de la Serna J et al. 2018 BMT Tandem Meetings, Abstract LBA2.
SALT LAKE CITY – A recently approved adjuvanted herpes zoster vaccine)(Shingrix) effectively and safely prevented herpes zoster in a population of patients with multiple myeloma and other hematologic malignancies who received autologous hematopoietic stem cell transplantation.
The use of recombinant varicella zoster virus glycoprotein E in combination with an adjuvant system gives immunosuppressed individuals who have received hematopoietic stem cell transplantation (HSCT) a safe option for prevention of herpes zoster (HZ), said Javier de la Serna, MD, PhD, speaking at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
Presenting the findings at a late-breaking abstract session, Dr. de la Serna said that for the 1,721 participants in a placebo-controlled multicenter trial who received both doses of the vaccine, the incidence of HZ for vaccine recipients was 3.0%, compared with 9.4% of placebo recipients, for a vaccine efficacy of 68.2% (95% confidence interval, 55.6-77.5; P less than 0.0001). These results met the study’s primary objective.
Postherpetic neuralgia (PHN) prevention efficacy – a secondary endpoint – was 89.3% for those receiving the vaccine (HZ/su); the incidence of PHN was 0.5% in the HZ/su study arm, compared with 4.9% for those who received placebo (95% CI, 22.5-99.8). The study also tracked other HZ complications as a secondary endpoint, finding efficacy of 77.8% (95% CI, 19.1–95.0). “The vaccine was highly efficacious in preventing all the secondary outcomes,” said Dr. de la Serna of the Hospital Universitario 12 de Octubre, Madrid.
The randomized, observer-blind phase 3 trial was conducted in 28 countries.Adults who received autologous HSCT were randomized 1:1 to receive HZ/su (n = 922) or placebo (n = 924) within 50-70 days of their transplant. Patients were excluded if they were expected to receive more than 6 months of anti–varicella zoster prophylaxis posttransplant, Dr. de la Serna said.
Participants received the first dose of HZ/su at the first study visit, and the second dose 30-60 days later. Patients were seen 1 month after the last vaccine dose, and then again at months 13 and 25, with telephone follow-up between the later visits. All participants were followed for at least 1 year, Dr. de la Serna said.
Episodes of HZ were confirmed by polymerase chain reaction assay, or, when samples were lacking or indeterminate, by agreement of at least three members of an ascertainment committee.
Of the two components of the HZ/su vaccine, glycoprotein E triggers both humoral immunity and activity of varicella zoster–specific CD4+ T cells; the adjuvant system – dubbed ASO1 – boosts immune response. The vaccine was approved by the Food and Drug Administration in October 2017 for use in adults aged 50 years and older.
In addition to the primary endpoint of vaccine efficacy in prevention of HZ cases during the study period, secondary objectives included monitoring vaccine reactogenicity and safety, and evaluating vaccine efficacy for the prevention of PHN and other complications of HZ.
Tertiary objectives included vaccine efficacy in preventing HZ during the first year posttransplant (vaccine efficacy 84.7%; 95% CI, 32.2-96.6), as well as efficacy in preventing hospitalizations related to HZ (vaccine efficacy 76.2%, 95% CI 61.1-86.0).
An exploratory analysis found vaccine efficacy of 71.8% for participants younger than 50 years (95% CI, 38.8 – 88.3). For patients aged 50 years and older, vaccine efficacy was 67.3% (95% CI, 52.6–77.9).
The safety of HZ/su was determined by analyzing data for all participants, but efficacy data included only those who received the second dose and did not develop HZ within a month of receiving the second vaccine dose.
In the efficacy group (n = 1,721), patients were mostly (n = 1,296) aged 50 years or older. Most patients (n = 937) received HSCT for multiple myeloma. Overall, participants were about 63% male, and 77% were of Caucasian/European ancestry.
Adverse events, solicited for the first 7 days after injections, were mostly mild and related to the local site pain and inflammation expected with an adjuvanted vaccine; HZ/su recipients also experienced more fatigue and muscle aches than did those receiving placebo. Median duration of symptoms was up to 3 days, with grade 3 events lasting up to 2 days.
Unsolicited and serious adverse events were similar between study arms, with a median safety follow-up period of 29 months. The investigators judged that no deaths were related to the vaccine, and there were no signals for increased rate of relapse or immune-mediated diseases.
The study was funded by GlaxoSmithKline; HZ/su(Shingrix) is marketed by GlaxoSmithKline. Dr. de la Serna reported being on the advisory board or receiving honoraria from multiple pharmaceutical companies.
SOURCE: de la Serna J et al. 2018 BMT Tandem Meetings, Abstract LBA2.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Efficacy was 68.17% for preventing herpes zoster among HSCT recipients.
Study details: A randomized, observer blind, placebo-controlled phase 3 study of 1,846 post-HSCT recipients.
Disclosures: The study was sponsored by GlaxoSmithKline. Dr. de la Serna reported relationships with multiple pharmaceutical companies.
Source: de la Serna J et al. 2018 BMT Tandem Meetings, Abstract LBA2.
HCT-CI score may predict mortality for nonmalignant disease
SALT LAKE CITY – Scores of 3 or higher on the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) are associated with an increased risk of posttransplant mortality in certain patients undergoing allogeneic HCT for nonmalignant disease, according to findings from a review of more than 4,000 patients.
The exception was in patients undergoing HCT for hemoglobinopathies, Larisa Broglie, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The findings of the study, which is the largest to date to validate the usefulness of the HCT-CI for risk assessment in HCT patients with nonmalignant disease, have important implications for patient counseling and decision making, said Dr. Broglie of the Medical College of Wisconsin, Milwaukee.
Of 4,083 children and adults who underwent a first allogeneic HCT for a nonmalignant disease between 2007 and 2014 and who had sufficient follow-up (median, 39 months), 61% had an HCT-CI score of 0, 20% had a score of 1-2, and 19% had a score of 3 or higher.
After adjustment for age, disease, donor, graft source, recipient cytomegalovirus status, and performance status, scores of 3 or greater were associated with an overall increased hazard ratio for poor survival (HRs of 1.33 for scores of 3-4 and 2.31 for scores of 5 or greater, vs. 1.0 and 1.127 for scores of 0 or 1-2, respectively), she said.
Patients with an HCT-CI score of 0 had estimated 2-year overall survival of 82.7%, compared with 80.3% for scores 1-2, 74.0% for scores 3-4, and 55.8% for scores of 5 or greater.
Patients included in this study were identified from the Center for International Blood & Marrow Transplant Research database. They ranged in age from under 1 year to 77 years but most were young; the median age was 9 years and 78% of patients were under age 20.
HCT was performed for acquired aplastic anemia in 33% of patients, immune deficiencies in 19%, hemoglobinopathies in 16%, bone marrow failure in 12%, histiocytic disorders in 11%, metabolic disease in 9%, or autoimmune disease in less than 1%, she said, noting that the most frequent comorbidities seen within the entire cohort were moderate pulmonary disease, hepatic disease, and infection requiring ongoing treatment.
The effect of HCT-CI score on survival was present regardless of conditioning intensity and graft-versus-host disease prophylaxis, but scores predicted mortality risk differently based on underlying disease, and different comorbidities predominated in each disease category, she said, explaining that this was apparent when patients were stratified by the seven represented nonmalignant disease categories to account for disease heterogeneity.
For example, HCT-CI score predicted mortality risk in patients with aplastic anemia (HRs of 1.00, 1.19, and 2.06 for scores of 0, 1-2, and 3 or greater, respectively), and in patients with immune deficiency (HRs of 1.00, 1.37, and 1.87 for scores of 0, 1-2, and 3 or greater, respectively), and the distribution of comorbidities in patients in these two disease categories was similar to that of the overall cohort.
However, HCT-CI score did not predict mortality risk in those undergoing HCT for hemoglobinopathies (HRs of 1.00, 0.46, and 0.59 for scores of 0, 1-2, and 3 or greater, respectively), Dr. Broglie said, noting that these patients had overall high survival rates regardless of HCT-CI scores, and they had comorbidities that differed from the overall cohort.
HCT is a curative treatment strategy for many patients with nonmalignant diseases but transplant-related mortality remains a concern, she said. While HCT-CI has been shown to be useful for discriminating the risks of nonrelapse and overall survival among patients with hematologic malignancies who undergo allogeneic HCT, its usefulness in patients undergoing HCT for nonmalignant diseases has been less clear.
The distinction is important, as patients with nonmalignant diseases have different pretransplant exposures and may have comorbidities specific to their underlying disease. Furthermore, transplantation approaches – including conditioning regimens and intensities – differ, she said.
“And the HCT-CI was developed to predict risk of nonrelapse mortality, but relapse in nonmalignant diseases can often be difficult to define,” she added.
The current findings demonstrate the value of the HCT-CI in nonmalignant diseases, and “offer the potential to intervene with transplantation prior to the onset of comorbidities, or with efforts to prevent comorbidities prior to transplantation,” she said, concluding that “future efforts could focus on further refining pretransplant risk assessment for patients with nonmalignant diseases, especially for patients with hemoglobinopathies and HCT-CI scores of less than 3.”
Dr. Broglie reported having no financial disclosures.
sworcester@frontlinemedcom.com
SOURCE: Broglie L et al. Abstract 16.
SALT LAKE CITY – Scores of 3 or higher on the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) are associated with an increased risk of posttransplant mortality in certain patients undergoing allogeneic HCT for nonmalignant disease, according to findings from a review of more than 4,000 patients.
The exception was in patients undergoing HCT for hemoglobinopathies, Larisa Broglie, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The findings of the study, which is the largest to date to validate the usefulness of the HCT-CI for risk assessment in HCT patients with nonmalignant disease, have important implications for patient counseling and decision making, said Dr. Broglie of the Medical College of Wisconsin, Milwaukee.
Of 4,083 children and adults who underwent a first allogeneic HCT for a nonmalignant disease between 2007 and 2014 and who had sufficient follow-up (median, 39 months), 61% had an HCT-CI score of 0, 20% had a score of 1-2, and 19% had a score of 3 or higher.
After adjustment for age, disease, donor, graft source, recipient cytomegalovirus status, and performance status, scores of 3 or greater were associated with an overall increased hazard ratio for poor survival (HRs of 1.33 for scores of 3-4 and 2.31 for scores of 5 or greater, vs. 1.0 and 1.127 for scores of 0 or 1-2, respectively), she said.
Patients with an HCT-CI score of 0 had estimated 2-year overall survival of 82.7%, compared with 80.3% for scores 1-2, 74.0% for scores 3-4, and 55.8% for scores of 5 or greater.
Patients included in this study were identified from the Center for International Blood & Marrow Transplant Research database. They ranged in age from under 1 year to 77 years but most were young; the median age was 9 years and 78% of patients were under age 20.
HCT was performed for acquired aplastic anemia in 33% of patients, immune deficiencies in 19%, hemoglobinopathies in 16%, bone marrow failure in 12%, histiocytic disorders in 11%, metabolic disease in 9%, or autoimmune disease in less than 1%, she said, noting that the most frequent comorbidities seen within the entire cohort were moderate pulmonary disease, hepatic disease, and infection requiring ongoing treatment.
The effect of HCT-CI score on survival was present regardless of conditioning intensity and graft-versus-host disease prophylaxis, but scores predicted mortality risk differently based on underlying disease, and different comorbidities predominated in each disease category, she said, explaining that this was apparent when patients were stratified by the seven represented nonmalignant disease categories to account for disease heterogeneity.
For example, HCT-CI score predicted mortality risk in patients with aplastic anemia (HRs of 1.00, 1.19, and 2.06 for scores of 0, 1-2, and 3 or greater, respectively), and in patients with immune deficiency (HRs of 1.00, 1.37, and 1.87 for scores of 0, 1-2, and 3 or greater, respectively), and the distribution of comorbidities in patients in these two disease categories was similar to that of the overall cohort.
However, HCT-CI score did not predict mortality risk in those undergoing HCT for hemoglobinopathies (HRs of 1.00, 0.46, and 0.59 for scores of 0, 1-2, and 3 or greater, respectively), Dr. Broglie said, noting that these patients had overall high survival rates regardless of HCT-CI scores, and they had comorbidities that differed from the overall cohort.
HCT is a curative treatment strategy for many patients with nonmalignant diseases but transplant-related mortality remains a concern, she said. While HCT-CI has been shown to be useful for discriminating the risks of nonrelapse and overall survival among patients with hematologic malignancies who undergo allogeneic HCT, its usefulness in patients undergoing HCT for nonmalignant diseases has been less clear.
The distinction is important, as patients with nonmalignant diseases have different pretransplant exposures and may have comorbidities specific to their underlying disease. Furthermore, transplantation approaches – including conditioning regimens and intensities – differ, she said.
“And the HCT-CI was developed to predict risk of nonrelapse mortality, but relapse in nonmalignant diseases can often be difficult to define,” she added.
The current findings demonstrate the value of the HCT-CI in nonmalignant diseases, and “offer the potential to intervene with transplantation prior to the onset of comorbidities, or with efforts to prevent comorbidities prior to transplantation,” she said, concluding that “future efforts could focus on further refining pretransplant risk assessment for patients with nonmalignant diseases, especially for patients with hemoglobinopathies and HCT-CI scores of less than 3.”
Dr. Broglie reported having no financial disclosures.
sworcester@frontlinemedcom.com
SOURCE: Broglie L et al. Abstract 16.
SALT LAKE CITY – Scores of 3 or higher on the Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) are associated with an increased risk of posttransplant mortality in certain patients undergoing allogeneic HCT for nonmalignant disease, according to findings from a review of more than 4,000 patients.
The exception was in patients undergoing HCT for hemoglobinopathies, Larisa Broglie, MD, reported at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society for Blood and Marrow Transplantation.
The findings of the study, which is the largest to date to validate the usefulness of the HCT-CI for risk assessment in HCT patients with nonmalignant disease, have important implications for patient counseling and decision making, said Dr. Broglie of the Medical College of Wisconsin, Milwaukee.
Of 4,083 children and adults who underwent a first allogeneic HCT for a nonmalignant disease between 2007 and 2014 and who had sufficient follow-up (median, 39 months), 61% had an HCT-CI score of 0, 20% had a score of 1-2, and 19% had a score of 3 or higher.
After adjustment for age, disease, donor, graft source, recipient cytomegalovirus status, and performance status, scores of 3 or greater were associated with an overall increased hazard ratio for poor survival (HRs of 1.33 for scores of 3-4 and 2.31 for scores of 5 or greater, vs. 1.0 and 1.127 for scores of 0 or 1-2, respectively), she said.
Patients with an HCT-CI score of 0 had estimated 2-year overall survival of 82.7%, compared with 80.3% for scores 1-2, 74.0% for scores 3-4, and 55.8% for scores of 5 or greater.
Patients included in this study were identified from the Center for International Blood & Marrow Transplant Research database. They ranged in age from under 1 year to 77 years but most were young; the median age was 9 years and 78% of patients were under age 20.
HCT was performed for acquired aplastic anemia in 33% of patients, immune deficiencies in 19%, hemoglobinopathies in 16%, bone marrow failure in 12%, histiocytic disorders in 11%, metabolic disease in 9%, or autoimmune disease in less than 1%, she said, noting that the most frequent comorbidities seen within the entire cohort were moderate pulmonary disease, hepatic disease, and infection requiring ongoing treatment.
The effect of HCT-CI score on survival was present regardless of conditioning intensity and graft-versus-host disease prophylaxis, but scores predicted mortality risk differently based on underlying disease, and different comorbidities predominated in each disease category, she said, explaining that this was apparent when patients were stratified by the seven represented nonmalignant disease categories to account for disease heterogeneity.
For example, HCT-CI score predicted mortality risk in patients with aplastic anemia (HRs of 1.00, 1.19, and 2.06 for scores of 0, 1-2, and 3 or greater, respectively), and in patients with immune deficiency (HRs of 1.00, 1.37, and 1.87 for scores of 0, 1-2, and 3 or greater, respectively), and the distribution of comorbidities in patients in these two disease categories was similar to that of the overall cohort.
However, HCT-CI score did not predict mortality risk in those undergoing HCT for hemoglobinopathies (HRs of 1.00, 0.46, and 0.59 for scores of 0, 1-2, and 3 or greater, respectively), Dr. Broglie said, noting that these patients had overall high survival rates regardless of HCT-CI scores, and they had comorbidities that differed from the overall cohort.
HCT is a curative treatment strategy for many patients with nonmalignant diseases but transplant-related mortality remains a concern, she said. While HCT-CI has been shown to be useful for discriminating the risks of nonrelapse and overall survival among patients with hematologic malignancies who undergo allogeneic HCT, its usefulness in patients undergoing HCT for nonmalignant diseases has been less clear.
The distinction is important, as patients with nonmalignant diseases have different pretransplant exposures and may have comorbidities specific to their underlying disease. Furthermore, transplantation approaches – including conditioning regimens and intensities – differ, she said.
“And the HCT-CI was developed to predict risk of nonrelapse mortality, but relapse in nonmalignant diseases can often be difficult to define,” she added.
The current findings demonstrate the value of the HCT-CI in nonmalignant diseases, and “offer the potential to intervene with transplantation prior to the onset of comorbidities, or with efforts to prevent comorbidities prior to transplantation,” she said, concluding that “future efforts could focus on further refining pretransplant risk assessment for patients with nonmalignant diseases, especially for patients with hemoglobinopathies and HCT-CI scores of less than 3.”
Dr. Broglie reported having no financial disclosures.
sworcester@frontlinemedcom.com
SOURCE: Broglie L et al. Abstract 16.
REPORTING FROM THE 2018 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Hazard ratios for poor survival were 1.33 for scores of 3-4 and 2.31 for scores of 5 or greater, compared with 1.0 and 1.127 for scores of 0 or 1-2, respectively.
Study details: A review of 4,083 patients from the CIBMTR database.
Disclosures: Dr. Broglie reported having no financial disclosures.
Source: Broglie L et al. Abstract 16.
Promising results with expanded UCB product
SALT LAKE CITY—An expanded umbilical cord blood (UCB) product can produce favorable outcomes as a stand-alone graft, according to a presentation at the 2018 BMT Tandem Meetings.
The product, MGTA-456, provided “rapid and durable” engraftment in patients with hematologic malignancies, according to John E. Wagner, MD, of the University of Minnesota in Minneapolis.
He also said MGTA-456 “preserved the clinical benefits” of UCB transplant, including low rates of graft-vs-host disease (GVHD) and high overall survival (OS).
Dr Wagner presented these results as one of the “Best Abstracts” at this year’s BMT Tandem Meetings (abstract 4). The research was supported by Novartis and Magenta Therapeutics.
MGTA-456 is developed by dividing a UCB unit into a CD34- portion and a CD34+ portion, then expanding the CD34+ portion for 15 days via culture with an aryl hydrocarbon receptor antagonist (SR-1), stem cell factor, FLT3 ligand, interleukin-6, and thrombopoietin.
In a previous study,* MGTA-456 enhanced hematopoietic recovery when given as half of a double UCB transplant.
With the current research, Dr Wagner and his colleagues evaluated MGTA-456 as a stand-alone graft. The team conducted two phase 2 trials of MGTA-456, one in which patients received myeloablative conditioning (MAC) and one in which patients received non-myeloablative conditioning (NMAC).
Treatment
Each trial included 10 patients with a high-risk hematologic malignancy and a partially HLA-matched UCB unit. In each trial, 1 patient could not receive MGTA-456 due to low expansion.
So 9 patients received MAC—cyclophosphamide (CY) at 60 mg/kg/day on days -6 and -5, fludarabine (FLU) at 25 mg/m2/day on days -7 to -5, and total body irradiation (TBI) at 1320 cGy on days -4 to -1.
And 9 patients received NMAC—CY at 50 mg/kg on day -6, FLU at 40 mg/m2/day on days -6 to -2, and TBI at 200 cGy on day -1. Some patients who had not received recent chemotherapy also received antithymocyte globulin as part of their conditioning regimen.
For MAC recipients, the median expansion of CD34+ cells was 406-fold (range, 162-1643). The median CD34 cell dose they received was 16.2 x 106/kg.
For NMAC recipients, the median expansion of CD34+ cells was 274-fold (range, 42-527). The median CD34 cell dose they received was 13.4 x 106/kg.
All patients received cyclosporine and mycophenolate mofetil as GVHD prophylaxis.
Dr Wagner and his colleagues compared outcomes in these MGTA-456 recipients to outcomes in historical control subjects—151 patients who received MAC and 132 who received NMAC.
MAC recipients
The 9 MAC/MGTA-456 recipients had a median age of 25 (range, 15-53). Seven of the patients had acute leukemia, 1 had myelodysplastic syndrome (MDS), and 1 had lymphoma.
Eleven percent of patients had high-risk disease, 89% were cytomegalovirus seropositive, and 89% had a Karnofsky performance score of 90 to 100.
The only significant difference between the MGTA-456 recipients and historical controls was weight. The median weight was 93.8 kg (range, 41-107) for MGTA-456 recipients and 66.7 kg (range, 11-136) for controls (P=0.04).
The MGTA-456 recipients had superior hematopoietic recovery compared to historical controls.
The rate of neutrophil engraftment was 100% for MGTA-456 recipients and 89% for controls. The median time to neutrophil engraftment was 14 days and 23 days, respectively (P<0.01).
The rate of platelet engraftment was 89% for MGTA-456 recipients and 71% for controls. The median time to platelet engraftment was 46 days and 64 days, respectively (P=0.01).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 22% for MGTA-456 recipients and 24% for controls (P=0.78). The incidence of chronic GVHD at 1 year was 11% and 21%, respectively (P=0.48).
The 2-year OS rate was 67% in MGTA-456 recipients and 55% in controls (P=0.59).
NMAC recipients
There were significant differences between the 9 NMAC/MGTA-456 recipients and the 132 NMAC historical controls when it came to age (P=0.03), disease type (P<0.01), and disease status (P=0.03).
The median age was 65 (range, 29-70) for MGTA-456 recipients and 53 (range, 6-72) for historical controls. The median weights were 93.4 kg (range, 55-111) and 81.4 kg (range, 22-145), respectively.
Diagnoses among MGTA-456 recipients included acute leukemia (n=1), MDS (n=4), chronic leukemia (n=1), lymphoma (n=1), and “other” (n=2). Diagnoses among historical controls included acute leukemia (n=61), MDS (n=25), chronic leukemia (n=9), lymphoma (n=35), and “other” (n=2).
Eighty-nine percent of MGTA-456 recipients and 49% of historical controls had high-risk disease. Sixty-seven percent and 64%, respectively, were cytomegalovirus seropositive. Sixty-seven percent and 85%, respectively, had a Karnofsky performance score of 90 to 100.
NMAC recipients who received MGTA-456 had superior neutrophil recovery but platelet recovery that was comparable to that of historical controls.
The rate of neutrophil engraftment was 100% in MGTA-456 recipients and 95% in historical controls. The median time to neutrophil engraftment was 7 days and 15 days, respectively (P<0.01).
The rate of platelet engraftment was 56% for MGTA-456 recipients and 77% for historical controls. The median time to platelet engraftment was 107 days and 47 days, respectively (P=0.19).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 43% for MGTA-456 recipients and 15% for controls (P=0.11). The incidence of chronic GVHD at 1 year was 0% and 19%, respectively (P=0.17).
The 2-year OS rate was 44% in MGTA-456 recipients and 49% in controls (P=0.80).
*Wagner JE Jr et al; Phase I/II Trial of StemRegenin-1 Expanded Umbilical Cord Blood Hematopoietic Stem Cells Supports Testing as a Stand-Alone Graft. Cell Stem Cell 2016; 18(1):144-155.
SALT LAKE CITY—An expanded umbilical cord blood (UCB) product can produce favorable outcomes as a stand-alone graft, according to a presentation at the 2018 BMT Tandem Meetings.
The product, MGTA-456, provided “rapid and durable” engraftment in patients with hematologic malignancies, according to John E. Wagner, MD, of the University of Minnesota in Minneapolis.
He also said MGTA-456 “preserved the clinical benefits” of UCB transplant, including low rates of graft-vs-host disease (GVHD) and high overall survival (OS).
Dr Wagner presented these results as one of the “Best Abstracts” at this year’s BMT Tandem Meetings (abstract 4). The research was supported by Novartis and Magenta Therapeutics.
MGTA-456 is developed by dividing a UCB unit into a CD34- portion and a CD34+ portion, then expanding the CD34+ portion for 15 days via culture with an aryl hydrocarbon receptor antagonist (SR-1), stem cell factor, FLT3 ligand, interleukin-6, and thrombopoietin.
In a previous study,* MGTA-456 enhanced hematopoietic recovery when given as half of a double UCB transplant.
With the current research, Dr Wagner and his colleagues evaluated MGTA-456 as a stand-alone graft. The team conducted two phase 2 trials of MGTA-456, one in which patients received myeloablative conditioning (MAC) and one in which patients received non-myeloablative conditioning (NMAC).
Treatment
Each trial included 10 patients with a high-risk hematologic malignancy and a partially HLA-matched UCB unit. In each trial, 1 patient could not receive MGTA-456 due to low expansion.
So 9 patients received MAC—cyclophosphamide (CY) at 60 mg/kg/day on days -6 and -5, fludarabine (FLU) at 25 mg/m2/day on days -7 to -5, and total body irradiation (TBI) at 1320 cGy on days -4 to -1.
And 9 patients received NMAC—CY at 50 mg/kg on day -6, FLU at 40 mg/m2/day on days -6 to -2, and TBI at 200 cGy on day -1. Some patients who had not received recent chemotherapy also received antithymocyte globulin as part of their conditioning regimen.
For MAC recipients, the median expansion of CD34+ cells was 406-fold (range, 162-1643). The median CD34 cell dose they received was 16.2 x 106/kg.
For NMAC recipients, the median expansion of CD34+ cells was 274-fold (range, 42-527). The median CD34 cell dose they received was 13.4 x 106/kg.
All patients received cyclosporine and mycophenolate mofetil as GVHD prophylaxis.
Dr Wagner and his colleagues compared outcomes in these MGTA-456 recipients to outcomes in historical control subjects—151 patients who received MAC and 132 who received NMAC.
MAC recipients
The 9 MAC/MGTA-456 recipients had a median age of 25 (range, 15-53). Seven of the patients had acute leukemia, 1 had myelodysplastic syndrome (MDS), and 1 had lymphoma.
Eleven percent of patients had high-risk disease, 89% were cytomegalovirus seropositive, and 89% had a Karnofsky performance score of 90 to 100.
The only significant difference between the MGTA-456 recipients and historical controls was weight. The median weight was 93.8 kg (range, 41-107) for MGTA-456 recipients and 66.7 kg (range, 11-136) for controls (P=0.04).
The MGTA-456 recipients had superior hematopoietic recovery compared to historical controls.
The rate of neutrophil engraftment was 100% for MGTA-456 recipients and 89% for controls. The median time to neutrophil engraftment was 14 days and 23 days, respectively (P<0.01).
The rate of platelet engraftment was 89% for MGTA-456 recipients and 71% for controls. The median time to platelet engraftment was 46 days and 64 days, respectively (P=0.01).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 22% for MGTA-456 recipients and 24% for controls (P=0.78). The incidence of chronic GVHD at 1 year was 11% and 21%, respectively (P=0.48).
The 2-year OS rate was 67% in MGTA-456 recipients and 55% in controls (P=0.59).
NMAC recipients
There were significant differences between the 9 NMAC/MGTA-456 recipients and the 132 NMAC historical controls when it came to age (P=0.03), disease type (P<0.01), and disease status (P=0.03).
The median age was 65 (range, 29-70) for MGTA-456 recipients and 53 (range, 6-72) for historical controls. The median weights were 93.4 kg (range, 55-111) and 81.4 kg (range, 22-145), respectively.
Diagnoses among MGTA-456 recipients included acute leukemia (n=1), MDS (n=4), chronic leukemia (n=1), lymphoma (n=1), and “other” (n=2). Diagnoses among historical controls included acute leukemia (n=61), MDS (n=25), chronic leukemia (n=9), lymphoma (n=35), and “other” (n=2).
Eighty-nine percent of MGTA-456 recipients and 49% of historical controls had high-risk disease. Sixty-seven percent and 64%, respectively, were cytomegalovirus seropositive. Sixty-seven percent and 85%, respectively, had a Karnofsky performance score of 90 to 100.
NMAC recipients who received MGTA-456 had superior neutrophil recovery but platelet recovery that was comparable to that of historical controls.
The rate of neutrophil engraftment was 100% in MGTA-456 recipients and 95% in historical controls. The median time to neutrophil engraftment was 7 days and 15 days, respectively (P<0.01).
The rate of platelet engraftment was 56% for MGTA-456 recipients and 77% for historical controls. The median time to platelet engraftment was 107 days and 47 days, respectively (P=0.19).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 43% for MGTA-456 recipients and 15% for controls (P=0.11). The incidence of chronic GVHD at 1 year was 0% and 19%, respectively (P=0.17).
The 2-year OS rate was 44% in MGTA-456 recipients and 49% in controls (P=0.80).
*Wagner JE Jr et al; Phase I/II Trial of StemRegenin-1 Expanded Umbilical Cord Blood Hematopoietic Stem Cells Supports Testing as a Stand-Alone Graft. Cell Stem Cell 2016; 18(1):144-155.
SALT LAKE CITY—An expanded umbilical cord blood (UCB) product can produce favorable outcomes as a stand-alone graft, according to a presentation at the 2018 BMT Tandem Meetings.
The product, MGTA-456, provided “rapid and durable” engraftment in patients with hematologic malignancies, according to John E. Wagner, MD, of the University of Minnesota in Minneapolis.
He also said MGTA-456 “preserved the clinical benefits” of UCB transplant, including low rates of graft-vs-host disease (GVHD) and high overall survival (OS).
Dr Wagner presented these results as one of the “Best Abstracts” at this year’s BMT Tandem Meetings (abstract 4). The research was supported by Novartis and Magenta Therapeutics.
MGTA-456 is developed by dividing a UCB unit into a CD34- portion and a CD34+ portion, then expanding the CD34+ portion for 15 days via culture with an aryl hydrocarbon receptor antagonist (SR-1), stem cell factor, FLT3 ligand, interleukin-6, and thrombopoietin.
In a previous study,* MGTA-456 enhanced hematopoietic recovery when given as half of a double UCB transplant.
With the current research, Dr Wagner and his colleagues evaluated MGTA-456 as a stand-alone graft. The team conducted two phase 2 trials of MGTA-456, one in which patients received myeloablative conditioning (MAC) and one in which patients received non-myeloablative conditioning (NMAC).
Treatment
Each trial included 10 patients with a high-risk hematologic malignancy and a partially HLA-matched UCB unit. In each trial, 1 patient could not receive MGTA-456 due to low expansion.
So 9 patients received MAC—cyclophosphamide (CY) at 60 mg/kg/day on days -6 and -5, fludarabine (FLU) at 25 mg/m2/day on days -7 to -5, and total body irradiation (TBI) at 1320 cGy on days -4 to -1.
And 9 patients received NMAC—CY at 50 mg/kg on day -6, FLU at 40 mg/m2/day on days -6 to -2, and TBI at 200 cGy on day -1. Some patients who had not received recent chemotherapy also received antithymocyte globulin as part of their conditioning regimen.
For MAC recipients, the median expansion of CD34+ cells was 406-fold (range, 162-1643). The median CD34 cell dose they received was 16.2 x 106/kg.
For NMAC recipients, the median expansion of CD34+ cells was 274-fold (range, 42-527). The median CD34 cell dose they received was 13.4 x 106/kg.
All patients received cyclosporine and mycophenolate mofetil as GVHD prophylaxis.
Dr Wagner and his colleagues compared outcomes in these MGTA-456 recipients to outcomes in historical control subjects—151 patients who received MAC and 132 who received NMAC.
MAC recipients
The 9 MAC/MGTA-456 recipients had a median age of 25 (range, 15-53). Seven of the patients had acute leukemia, 1 had myelodysplastic syndrome (MDS), and 1 had lymphoma.
Eleven percent of patients had high-risk disease, 89% were cytomegalovirus seropositive, and 89% had a Karnofsky performance score of 90 to 100.
The only significant difference between the MGTA-456 recipients and historical controls was weight. The median weight was 93.8 kg (range, 41-107) for MGTA-456 recipients and 66.7 kg (range, 11-136) for controls (P=0.04).
The MGTA-456 recipients had superior hematopoietic recovery compared to historical controls.
The rate of neutrophil engraftment was 100% for MGTA-456 recipients and 89% for controls. The median time to neutrophil engraftment was 14 days and 23 days, respectively (P<0.01).
The rate of platelet engraftment was 89% for MGTA-456 recipients and 71% for controls. The median time to platelet engraftment was 46 days and 64 days, respectively (P=0.01).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 22% for MGTA-456 recipients and 24% for controls (P=0.78). The incidence of chronic GVHD at 1 year was 11% and 21%, respectively (P=0.48).
The 2-year OS rate was 67% in MGTA-456 recipients and 55% in controls (P=0.59).
NMAC recipients
There were significant differences between the 9 NMAC/MGTA-456 recipients and the 132 NMAC historical controls when it came to age (P=0.03), disease type (P<0.01), and disease status (P=0.03).
The median age was 65 (range, 29-70) for MGTA-456 recipients and 53 (range, 6-72) for historical controls. The median weights were 93.4 kg (range, 55-111) and 81.4 kg (range, 22-145), respectively.
Diagnoses among MGTA-456 recipients included acute leukemia (n=1), MDS (n=4), chronic leukemia (n=1), lymphoma (n=1), and “other” (n=2). Diagnoses among historical controls included acute leukemia (n=61), MDS (n=25), chronic leukemia (n=9), lymphoma (n=35), and “other” (n=2).
Eighty-nine percent of MGTA-456 recipients and 49% of historical controls had high-risk disease. Sixty-seven percent and 64%, respectively, were cytomegalovirus seropositive. Sixty-seven percent and 85%, respectively, had a Karnofsky performance score of 90 to 100.
NMAC recipients who received MGTA-456 had superior neutrophil recovery but platelet recovery that was comparable to that of historical controls.
The rate of neutrophil engraftment was 100% in MGTA-456 recipients and 95% in historical controls. The median time to neutrophil engraftment was 7 days and 15 days, respectively (P<0.01).
The rate of platelet engraftment was 56% for MGTA-456 recipients and 77% for historical controls. The median time to platelet engraftment was 107 days and 47 days, respectively (P=0.19).
There was no significant difference between MGTA-456 recipients and historical controls when it came to GVHD or OS.
The incidence of grade 3-4 acute GVHD at 100 days was 43% for MGTA-456 recipients and 15% for controls (P=0.11). The incidence of chronic GVHD at 1 year was 0% and 19%, respectively (P=0.17).
The 2-year OS rate was 44% in MGTA-456 recipients and 49% in controls (P=0.80).
*Wagner JE Jr et al; Phase I/II Trial of StemRegenin-1 Expanded Umbilical Cord Blood Hematopoietic Stem Cells Supports Testing as a Stand-Alone Graft. Cell Stem Cell 2016; 18(1):144-155.
Outcomes appear similar with MAC and RIC
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
SALT LAKE CITY—New research suggests outcomes may be similar whether patients receive myeloablative conditioning (MAC) or reduced-intensity conditioning (RIC) prior to haploidentical peripheral blood stem cell transplant (haploPBSCT) with post-transplant cyclophosphamide (PTCy).
Results from 2 parallel, phase 2 trials showed that MAC-PTCy-haploPBSCT and RIC-PTCy-haploPBSCT produced comparable rates of engraftment, acute and chronic graft-versus host disease (GVHD), relapse, and non-relapse mortality (NRM).
Rates of overall survival (OS) and event-free survival (EFS) were significantly higher in the MAC group. However, the fact that some RIC recipients had received prior allogeneic transplants—and none of the MAC recipients had—appeared to play a role in survival outcomes.
Junichi Sugita, MD, PhD, of Hokkaido University in Sapporo, Japan, presented these results at the 2018 BMT Tandem Meetings (abstract 50*).
To compare MAC and RIC in the context of PTCy-haploPBSCT, Dr Sugita and his colleagues conducted 2 parallel studies—JSCT Haplo 14 MAC and JSCT Haplo 14 RIC.
Patients
There were 50 patients in the MAC trial and 77 in the RIC trial. They had median ages of 36 (range, 17 to 60) and 58 (range, 22 to 65), respectively (P<0.01). There was a greater percentage of male patients among MAC recipients (82% vs 62%, P=0.028).
Diagnoses were similar between the groups and included:
- Acute myeloid leukemia—23 MAC, 34 RIC
- Acute lymphoblastic leukemia—11 MAC, 14 RIC
- Myelodysplastic syndromes/myeloproliferative neoplasms—6 MAC, 12 RIC
- Lymphoma—6 MAC, 14 RIC
- “Other”—4 MAC, 3 RIC.
Forty-eight percent (n=24) of MAC recipients and 58% (n=45) of RIC recipients were not in remission at transplant (P=0.48). There were no significant differences in disease risk index (P=0.34).
Thirty-nine percent of RIC recipients (n=30) had a history of allogeneic transplant, but none of the MAC recipients did (P<0.01).
Conditioning and prophylaxis
There were 2 MAC regimens. One consisted of fludarabine (Flu, 30 mg/m2/day on days -6 to -4) plus total body irradiation (TBI, 12 Gy on days -3 to -1). The other consisted of Flu (30 mg/m2/day on days -6 to -2), busulfan (BU, 3.2 mg/kg/day on days -6 to -3), and TBI (4 Gy on day -1).
The RIC regimen consisted of Flu (30 mg/m2/day on days -6 to -2), BU (3.2 mg/kg/day on days -4 to -3), and TBI (4 Gy on day -1).
All patients received GVHD prophylaxis consisting of cyclophosphamide (50 mg/kg/day on days 3 and 4), tacrolimus (days 5 to 180), and mycophenolate mofetil (days 5 to 60).
Graft
Siblings were the most common donors for MAC recipients (50%, n=25), followed by parents (28%, n=14), children (16%, n=8), and “other” donors (6%, n=3).
Children were the most common donors for RIC recipients (60%, n=46), followed by siblings (33%, n=25), and parents (8%, n=6).
There was no significant difference between MAC and RIC recipients when it came to human leukocyte antigen matching, cytomegalovirus serostatus, or CD34 cell dose.
However, there was a significant difference in donor-recipient gender matching (P=0.033).
Fifty-two percent (n=26) of MAC recipients and 62% (n=48) of RIC recipients had a donor-recipient gender match. Forty-two percent (n=21) and 22% (n=17), respectively, had female donor to male recipient.
Engraftment and GVHD
“Hematopoietic recovery was similar between MAC and RIC,” Dr Sugita said.
The cumulative incidence of neutrophil engraftment was 98% in MAC recipients and 94% in RIC recipients. The median time to neutrophil engraftment was 17 days and 18 days, respectively (P=0.10).
The cumulative incidence of platelet engraftment was 84% in the MAC recipients and 74% in the RIC recipients. The median time to platelet engraftment was 31 days and 37 days, respectively (P=0.32).
“Complete chimerism was achieved in all engrafted patients,” Dr Sugita noted.
There was no significant difference between MAC and RIC recipients when it came to acute or chronic GVHD.
At day 100, the cumulative incidence of grade 2-4 acute GVHD was 18% in the MAC group and 14% in the RIC group (P=0.52). Grade 3-4 acute GVHD was 8% and 5%, respectively (P=0.52).
At 2 years, the cumulative incidence of all-grade chronic GVHD was 36% in the MAC group and 27% in the RIC group (P=0.24). Moderate to severe chronic GVHD was 20% in both groups (P=1.0).
Relapse and survival
There was no significant between-group difference in NRM or relapse.
The cumulative incidence of NRM at 2 years was 20% in the RIC group and 10% in the MAC group (P=0.15). The cumulative incidence of relapse at 2 years was 45% and 36%, respectively (P=0.32).
Survival was superior in the MAC recipients. The 2-year OS was 68% in the MAC group and 44% in the RIC group (P=0.02). The 2-year EFS was 54% and 35%, respectively (P=0.04).
However, survival appeared to be affected by history of allogeneic transplant.
“Patients with a history of prior allogenic SCT have significantly worse overall survival and event-free survival,” Dr Sugita said.
Two-year OS was 31% in RIC recipients with a history of transplant and 52% in RIC recipients without a history of transplant (P=0.04). The OS was 68% in MAC recipients, all of whom had no history of transplant.
Two-year EFS was 21%, 44%, and 54%, respectively (P=0.02 for difference between 2 RIC groups).
In a multivariate analysis, conditioning regimen was not a significant predictor of NRM. The hazard ratio (HR) for RIC was 1.13 (P=0.85).
Likewise, conditioning regimen was not a significant predictor of relapse (HR=0.81, P=0.53), OS (HR=0.85, P=0.66), or EFS (HR=0.73, P=0.34).
“Our results indicate that both MAC and RIC are valid options for PTCy-haplo,” Dr Sugita said in closing.
“Ideally, a more precise comparison of MAC and RIC should be studied further in the setting of, if possible, a randomized trial.”
*Data in the abstract differs from the presentation.
HSCT approach provides ‘excellent’ survival in FA
SALT LAKE CITY—A “risk-adjusted” approach leads to “excellent” survival in patients with Fanconi anemia (FA) undergoing alternative donor hematopoietic stem cell transplant (HSCT), according to a speaker at the 2018 BMT Tandem Meetings.
All FA patients who received personalized doses of busulfan in place of total body irradiation (TBI) were alive and disease-free after undergoing HSCT for bone marrow failure or myelodysplastic syndrome (MDS).
None of the patients developed graft-vs-host disease (GVHD), and the most common toxicity was viral infection.
Parinda A. Mehta, MD, of Cincinnati Children’s Hospital Medical Center in Ohio, presented these results at this year’s BMT Tandem Meetings as abstract 109.*
“We all know that inherent chemotherapy and radiation sensitivity makes transplant for patients with Fanconi anemia quite challenging,” Dr Mehta began. “In our recently published, prospective, multi-institutional study, we showed excellent outcomes of alternative donor transplant in patients with Fanconi anemia without using radiation.”
“In that study,** TBI was replaced by pharmacokinetically adjusted busulfan. It proved that, yes, we can do alternative donor transplant successfully without radiation by showing an overall survival of 80% for a total of 45 patients. We were quite ecstatic to see these numbers.”
The study also showed that younger patients fared better with this regimen, and younger patients did best with the lowest dose of busulfan tested (0.6 mg/kg vs 0.8 to 1.0 mg/kg). In addition, patients who underwent HSCT for bone marrow failure had better outcomes than patients who had MDS.
This led Dr Mehta and her colleagues to hypothesize that adjusting busulfan dosing based on a patient’s age and disease status at HSCT could minimize toxicity and improve outcomes.
Patients
The researchers tested their theory in 22 FA patients. They had a median age of 7 (range, 4-27), and most (n=13) were female.
Twelve patients had pancytopenia, 6 had severe single-lineage cytopenia, 3 had low-grade MDS, and 1 patient had acute myeloid leukemia (AML).
Eighteen patients had a history of transfusions, and 3 had a history of androgen use.
Treatment
The preparative regimen consisted of 4 doses of busulfan (every 12 hours on day -7 to -6), followed by cyclophosphamide at 10 mg/kg/day (on day -5 to -2), fludarabine at 35 mg/m2/day (on day -5 to -2), and rabbit antithymocyte globulin at 2.5 mg/kg/day (on day -5 to -2).
Busulfan doses were adjusted according to age and disease status.
Children (age 18 and younger) with bone marrow failure received busulfan at 0.6 to 0.8 mg/kg. Children with MDS/AML received busulfan at 0.8 to 1.0 mg/kg. Adults (19 and older) received the lowest dose of busulfan—0.4 mg/kg—regardless of disease status.
“At the first sight, this will look counterintuitive . . . ,” Dr Mehta said. “However, based on our previous experience, in general and also from results of our previous study, this was specifically designed to avoid upfront TRM [transplant-related mortality] for these adult patients.”
All 22 patients received CD34-selected, T-cell-depleted peripheral blood stem cells from unrelated donors. Eleven patients received a fully matched graft (10/10), 8 patients had a 9/10 match, and 3 had an 8/10 match.
The median number of CD34+ cells/kg was 23.9 x 106 (range, 4.9-76.6), and the median number of CD3 cells/kg was 1 x 104 (range, 0.003-3.1).
T-cell depletion was the only GVHD prophylaxis used.
Patients with MDS/AML could receive azacitidine at day 42 after HSCT, an option intended to prevent relapse in these patients.
Toxicity
There were no cases of acute or chronic GVHD.
Toxicities included infections (n=24), oral mucositis (n=14), hyperbilirubinemia (n=2), pulmonary hemorrhage (n=1), and sinusoidal obstruction syndrome (n=1).
There were 20 viral infections, 4 bacterial infections, and no fungal infections. Viral infections included BK virus (n=7), cytomegalovirus (n=6), Epstein-Barr virus (n=6), and adenovirus (n=1).
Dr Mehta noted that viral infections are “not unexpected in a T-cell-depleted graft setting.”
“Because we know this complication [can occur], and we worry about our patients, one of the things that, in recent years, we have done is, we manufacture viral-specific CTLs [cytotoxic T lymphocytes] for all of these patients ahead of time whenever possible,” she said.
“To give you an example, 19 out of these 20 patients’ viral infections—or rather, viremias—are completely under control with the use of either antivirals or donor-specific CTLs, including a third-party CTL in one of the patients.”
Response and survival
All 22 patients engrafted. The median time to neutrophil engraftment was 9 days (range, 8-10), and the median time to platelet engraftment was 16 days (range, 11-40).
Twenty-one of the 22 patients (95%) were alive and disease-free at last follow-up. The median follow-up was 21 months (range, 6-44).
The single AML patient achieved remission but died of post-transplant lymphoproliferative disorder (PTLD) on day 202 after HSCT. Dr Mehta said this was due to partial loss of follow-up and noncompliance with medical recommendations during PTLD treatment.
The AML patient also had “significant upfront toxicity” but “recovered very nicely,” according to Dr Mehta. He had severe mucositis, herpetic stomatitis, and sinusoidal obstruction syndrome that responded to defibrotide.
“Overall, we are quite excited to see 95% overall survival for this cohort and conclude that the current risk-adjusted approach leads to excellent overall survival and disease-free survival in patients undergoing alternative donor transplant either for marrow failure or MDS/AML,” Dr Mehta said.
“Enrollment is ongoing, and we hope to see continued success in patients with MDS/AML as well as in adult patients.”
*Data in the abstract differ from the presentation.
**Mehta PA et al. Radiation-free, alternative donor HCT for Fanconi anemia patients: results from a prospective multi-institutional study. Blood 2017; doi: https://doi.org/10.1182/blood-2016-09-743112.
SALT LAKE CITY—A “risk-adjusted” approach leads to “excellent” survival in patients with Fanconi anemia (FA) undergoing alternative donor hematopoietic stem cell transplant (HSCT), according to a speaker at the 2018 BMT Tandem Meetings.
All FA patients who received personalized doses of busulfan in place of total body irradiation (TBI) were alive and disease-free after undergoing HSCT for bone marrow failure or myelodysplastic syndrome (MDS).
None of the patients developed graft-vs-host disease (GVHD), and the most common toxicity was viral infection.
Parinda A. Mehta, MD, of Cincinnati Children’s Hospital Medical Center in Ohio, presented these results at this year’s BMT Tandem Meetings as abstract 109.*
“We all know that inherent chemotherapy and radiation sensitivity makes transplant for patients with Fanconi anemia quite challenging,” Dr Mehta began. “In our recently published, prospective, multi-institutional study, we showed excellent outcomes of alternative donor transplant in patients with Fanconi anemia without using radiation.”
“In that study,** TBI was replaced by pharmacokinetically adjusted busulfan. It proved that, yes, we can do alternative donor transplant successfully without radiation by showing an overall survival of 80% for a total of 45 patients. We were quite ecstatic to see these numbers.”
The study also showed that younger patients fared better with this regimen, and younger patients did best with the lowest dose of busulfan tested (0.6 mg/kg vs 0.8 to 1.0 mg/kg). In addition, patients who underwent HSCT for bone marrow failure had better outcomes than patients who had MDS.
This led Dr Mehta and her colleagues to hypothesize that adjusting busulfan dosing based on a patient’s age and disease status at HSCT could minimize toxicity and improve outcomes.
Patients
The researchers tested their theory in 22 FA patients. They had a median age of 7 (range, 4-27), and most (n=13) were female.
Twelve patients had pancytopenia, 6 had severe single-lineage cytopenia, 3 had low-grade MDS, and 1 patient had acute myeloid leukemia (AML).
Eighteen patients had a history of transfusions, and 3 had a history of androgen use.
Treatment
The preparative regimen consisted of 4 doses of busulfan (every 12 hours on day -7 to -6), followed by cyclophosphamide at 10 mg/kg/day (on day -5 to -2), fludarabine at 35 mg/m2/day (on day -5 to -2), and rabbit antithymocyte globulin at 2.5 mg/kg/day (on day -5 to -2).
Busulfan doses were adjusted according to age and disease status.
Children (age 18 and younger) with bone marrow failure received busulfan at 0.6 to 0.8 mg/kg. Children with MDS/AML received busulfan at 0.8 to 1.0 mg/kg. Adults (19 and older) received the lowest dose of busulfan—0.4 mg/kg—regardless of disease status.
“At the first sight, this will look counterintuitive . . . ,” Dr Mehta said. “However, based on our previous experience, in general and also from results of our previous study, this was specifically designed to avoid upfront TRM [transplant-related mortality] for these adult patients.”
All 22 patients received CD34-selected, T-cell-depleted peripheral blood stem cells from unrelated donors. Eleven patients received a fully matched graft (10/10), 8 patients had a 9/10 match, and 3 had an 8/10 match.
The median number of CD34+ cells/kg was 23.9 x 106 (range, 4.9-76.6), and the median number of CD3 cells/kg was 1 x 104 (range, 0.003-3.1).
T-cell depletion was the only GVHD prophylaxis used.
Patients with MDS/AML could receive azacitidine at day 42 after HSCT, an option intended to prevent relapse in these patients.
Toxicity
There were no cases of acute or chronic GVHD.
Toxicities included infections (n=24), oral mucositis (n=14), hyperbilirubinemia (n=2), pulmonary hemorrhage (n=1), and sinusoidal obstruction syndrome (n=1).
There were 20 viral infections, 4 bacterial infections, and no fungal infections. Viral infections included BK virus (n=7), cytomegalovirus (n=6), Epstein-Barr virus (n=6), and adenovirus (n=1).
Dr Mehta noted that viral infections are “not unexpected in a T-cell-depleted graft setting.”
“Because we know this complication [can occur], and we worry about our patients, one of the things that, in recent years, we have done is, we manufacture viral-specific CTLs [cytotoxic T lymphocytes] for all of these patients ahead of time whenever possible,” she said.
“To give you an example, 19 out of these 20 patients’ viral infections—or rather, viremias—are completely under control with the use of either antivirals or donor-specific CTLs, including a third-party CTL in one of the patients.”
Response and survival
All 22 patients engrafted. The median time to neutrophil engraftment was 9 days (range, 8-10), and the median time to platelet engraftment was 16 days (range, 11-40).
Twenty-one of the 22 patients (95%) were alive and disease-free at last follow-up. The median follow-up was 21 months (range, 6-44).
The single AML patient achieved remission but died of post-transplant lymphoproliferative disorder (PTLD) on day 202 after HSCT. Dr Mehta said this was due to partial loss of follow-up and noncompliance with medical recommendations during PTLD treatment.
The AML patient also had “significant upfront toxicity” but “recovered very nicely,” according to Dr Mehta. He had severe mucositis, herpetic stomatitis, and sinusoidal obstruction syndrome that responded to defibrotide.
“Overall, we are quite excited to see 95% overall survival for this cohort and conclude that the current risk-adjusted approach leads to excellent overall survival and disease-free survival in patients undergoing alternative donor transplant either for marrow failure or MDS/AML,” Dr Mehta said.
“Enrollment is ongoing, and we hope to see continued success in patients with MDS/AML as well as in adult patients.”
*Data in the abstract differ from the presentation.
**Mehta PA et al. Radiation-free, alternative donor HCT for Fanconi anemia patients: results from a prospective multi-institutional study. Blood 2017; doi: https://doi.org/10.1182/blood-2016-09-743112.
SALT LAKE CITY—A “risk-adjusted” approach leads to “excellent” survival in patients with Fanconi anemia (FA) undergoing alternative donor hematopoietic stem cell transplant (HSCT), according to a speaker at the 2018 BMT Tandem Meetings.
All FA patients who received personalized doses of busulfan in place of total body irradiation (TBI) were alive and disease-free after undergoing HSCT for bone marrow failure or myelodysplastic syndrome (MDS).
None of the patients developed graft-vs-host disease (GVHD), and the most common toxicity was viral infection.
Parinda A. Mehta, MD, of Cincinnati Children’s Hospital Medical Center in Ohio, presented these results at this year’s BMT Tandem Meetings as abstract 109.*
“We all know that inherent chemotherapy and radiation sensitivity makes transplant for patients with Fanconi anemia quite challenging,” Dr Mehta began. “In our recently published, prospective, multi-institutional study, we showed excellent outcomes of alternative donor transplant in patients with Fanconi anemia without using radiation.”
“In that study,** TBI was replaced by pharmacokinetically adjusted busulfan. It proved that, yes, we can do alternative donor transplant successfully without radiation by showing an overall survival of 80% for a total of 45 patients. We were quite ecstatic to see these numbers.”
The study also showed that younger patients fared better with this regimen, and younger patients did best with the lowest dose of busulfan tested (0.6 mg/kg vs 0.8 to 1.0 mg/kg). In addition, patients who underwent HSCT for bone marrow failure had better outcomes than patients who had MDS.
This led Dr Mehta and her colleagues to hypothesize that adjusting busulfan dosing based on a patient’s age and disease status at HSCT could minimize toxicity and improve outcomes.
Patients
The researchers tested their theory in 22 FA patients. They had a median age of 7 (range, 4-27), and most (n=13) were female.
Twelve patients had pancytopenia, 6 had severe single-lineage cytopenia, 3 had low-grade MDS, and 1 patient had acute myeloid leukemia (AML).
Eighteen patients had a history of transfusions, and 3 had a history of androgen use.
Treatment
The preparative regimen consisted of 4 doses of busulfan (every 12 hours on day -7 to -6), followed by cyclophosphamide at 10 mg/kg/day (on day -5 to -2), fludarabine at 35 mg/m2/day (on day -5 to -2), and rabbit antithymocyte globulin at 2.5 mg/kg/day (on day -5 to -2).
Busulfan doses were adjusted according to age and disease status.
Children (age 18 and younger) with bone marrow failure received busulfan at 0.6 to 0.8 mg/kg. Children with MDS/AML received busulfan at 0.8 to 1.0 mg/kg. Adults (19 and older) received the lowest dose of busulfan—0.4 mg/kg—regardless of disease status.
“At the first sight, this will look counterintuitive . . . ,” Dr Mehta said. “However, based on our previous experience, in general and also from results of our previous study, this was specifically designed to avoid upfront TRM [transplant-related mortality] for these adult patients.”
All 22 patients received CD34-selected, T-cell-depleted peripheral blood stem cells from unrelated donors. Eleven patients received a fully matched graft (10/10), 8 patients had a 9/10 match, and 3 had an 8/10 match.
The median number of CD34+ cells/kg was 23.9 x 106 (range, 4.9-76.6), and the median number of CD3 cells/kg was 1 x 104 (range, 0.003-3.1).
T-cell depletion was the only GVHD prophylaxis used.
Patients with MDS/AML could receive azacitidine at day 42 after HSCT, an option intended to prevent relapse in these patients.
Toxicity
There were no cases of acute or chronic GVHD.
Toxicities included infections (n=24), oral mucositis (n=14), hyperbilirubinemia (n=2), pulmonary hemorrhage (n=1), and sinusoidal obstruction syndrome (n=1).
There were 20 viral infections, 4 bacterial infections, and no fungal infections. Viral infections included BK virus (n=7), cytomegalovirus (n=6), Epstein-Barr virus (n=6), and adenovirus (n=1).
Dr Mehta noted that viral infections are “not unexpected in a T-cell-depleted graft setting.”
“Because we know this complication [can occur], and we worry about our patients, one of the things that, in recent years, we have done is, we manufacture viral-specific CTLs [cytotoxic T lymphocytes] for all of these patients ahead of time whenever possible,” she said.
“To give you an example, 19 out of these 20 patients’ viral infections—or rather, viremias—are completely under control with the use of either antivirals or donor-specific CTLs, including a third-party CTL in one of the patients.”
Response and survival
All 22 patients engrafted. The median time to neutrophil engraftment was 9 days (range, 8-10), and the median time to platelet engraftment was 16 days (range, 11-40).
Twenty-one of the 22 patients (95%) were alive and disease-free at last follow-up. The median follow-up was 21 months (range, 6-44).
The single AML patient achieved remission but died of post-transplant lymphoproliferative disorder (PTLD) on day 202 after HSCT. Dr Mehta said this was due to partial loss of follow-up and noncompliance with medical recommendations during PTLD treatment.
The AML patient also had “significant upfront toxicity” but “recovered very nicely,” according to Dr Mehta. He had severe mucositis, herpetic stomatitis, and sinusoidal obstruction syndrome that responded to defibrotide.
“Overall, we are quite excited to see 95% overall survival for this cohort and conclude that the current risk-adjusted approach leads to excellent overall survival and disease-free survival in patients undergoing alternative donor transplant either for marrow failure or MDS/AML,” Dr Mehta said.
“Enrollment is ongoing, and we hope to see continued success in patients with MDS/AML as well as in adult patients.”
*Data in the abstract differ from the presentation.
**Mehta PA et al. Radiation-free, alternative donor HCT for Fanconi anemia patients: results from a prospective multi-institutional study. Blood 2017; doi: https://doi.org/10.1182/blood-2016-09-743112.
Study confirms higher risk of infection with CB transplant
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
SALT LAKE CITY—Results of a large, retrospective analysis support the notion that patients who receive cord blood (CB) transplants have a higher risk of infection than other hematopoietic stem cell transplant (HSCT) recipients.
Investigators found that CB recipients had a significantly higher risk of bacterial, viral, and fungal infections in the early post-transplant period than patients who received peripheral blood (PB) or bone marrow (BM) transplants.
In addition, CB recipients had longer hospital stays, higher inpatient costs, and greater inpatient mortality than PB and BM recipients.
Amandeep Godara, MD, of Tufts Medical Center in Boston, Massachusetts, presented these results at the 2018 BMT Tandem Meetings (abstract 30*).
“Infections are considered more common in cord blood transplant recipients based on some prior retrospective analyses,” Dr Godara noted. “But there is limited data comparing these infectious complications between cord blood transplant and peripheral blood/bone marrow stem cell transplants during the inpatient stay for the stem cell transplant.”
With this in mind, Dr Godara and his colleagues analyzed data from the Healthcare Cost and Utilization Project National Inpatient Sample. This database covers 46 US states and contains data from more than 7 million hospital stays each year.
The investigators searched the database for hospital admissions for HSCT from 2002 to 2014. They identified 2979 CB transplants and 56,845 PB or BM transplants.
The CB recipients had a median age of 48, and 55% were male. Fifty-nine percent were white, 18% Hispanic, 13% black, 5% Asian, and 5% “other.” Sixty-six percent of patients had acute leukemia, 18% non-Hodgkin lymphoma, 5% Hodgkin lymphoma, and 11% “other” diseases.
The PB/BM recipients had a median age of 45, and 58% were male. Seventy-nine percent were white, 8% Hispanic, 6% black, 3% Asian, and 4% “other.” Sixty-one percent of patients had acute leukemia, 16% non-Hodgkin lymphoma, 4% Hodgkin lymphoma, and 19% “other” diseases.
Results
Dr Godara and his colleagues compared the rates and types of infection from the time of HSCT to hospital discharge in CB and PB/BM recipients. The team also compared early inpatient mortality, the cost of hospitalization, and the length of hospital stay.
“[W]e observed a higher risk for infections in cord blood transplant patients compared to peripheral blood and bone marrow stem cell transplant patients, and this risk for infection extended through a wide spectrum of pathogens,” Dr Godara said.
“We also observed a higher all-cause inpatient mortality in cord blood transplant compared to peripheral blood and bone marrow transplant, especially in patients who had bacterial sepsis or invasive fungal infection.”
The rate of bacterial sepsis was 34.87% in CB recipients and 20.20% in PB/BM recipients (P<0.0001). Rates of viral infection were 20.05% and 8.19%, respectively (P<0.0001). And rates of invasive fungal infection were 12.87% and 7.89% (P<0.0001).
There was a similar distribution of bacterial infections in CB and PB/BM recipients. The most common was pneumonia (47% and 41%, respectively), followed by abdominal infections (29% and 31%, respectively), urinary tract infections (17% and 21%, respectively), central line-associated bloodstream infections (4% and 6%, respectively), and acute sinusitis (3% and 1%, respectively).
The rate of Clostridium difficile infection was significantly higher in CB recipients than PB/BM recipients—11.75% and 8.90%, respectively (P=0.02). However, there was no significant difference in mortality related to C. difficile—14% and 10%, respectively (P=0.3).
On the other hand, all-cause inpatient mortality was significantly higher in CB recipients than PB/BM recipients—16% and 7%, respectively (P<0.0001).
Inpatient mortality rates were significantly higher for CB recipients with bacterial sepsis (33% vs 23%, P=0.001) and invasive fungal infections (29% vs 16%, P=0.0045) but not viral infections (19% vs 17%, P=0.5).
The median length of hospital stay was 36 days for CB recipients and 25 days for PB/BM recipients. The mean inpatient charges were $448,892 and $250,437 respectively.
*Data in the abstract differ from the presentation.
Team identifies biomarkers for cGVHD in kids
SALT LAKE CITY—Researchers say they have identified prognostic biomarkers for chronic graft-vs-host disease (cGVHD) in children.
The group found that recent thymic emigrants (RTEs) and regulatory T cells expressing CD31 and CD45RA (Treg RTEs) were significantly lower at day 100 after transplant in patients who developed cGVHD.
Because prior research indicated that RTEs are higher in adults with cGVHD, the researchers concluded that thymic function may play a bigger role in cGVHD development for children than for adults.
Geoff D.E. Cuvelier, MD, of CancerCare Manitoba in Winnipeg, Canada, presented these findings at the 2018 BMT Tandem Meetings (abstract 104).
“Our group became interested in these populations of recent thymic emigrants when 2 adult studies1,2 . . . showed that higher proportions of recent thymic emigrants at day 100 were prognostic for the development of chronic graft-vs-host disease,” Dr Cuvelier said.
This led his group to evaluate whether RTEs (CD4+CD45RA+CD31+ T cells), as well as Treg RTEs—Tregs (CD4+CD25+CD127Low) that co-express naïve and recently emigrated markers (CD45RA+CD31+)—are prognostic for pediatric cGVHD at day 100 after allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers’ study enrolled patients younger than 18 years of age who underwent allo-HSCT to treat malignant and non-malignant diseases. There were 144 patients who had 1 year of follow-up after allo-HSCT.
Thirty-seven of the patients (25.7%) had cGVHD, and 34 (23.6%) had late acute GVHD (post-day 100). The remaining 73 patients (50.7%) had neither cGVHD nor late acute GVHD, so they served as controls.
Twenty cases of cGVHD were severe, 12 were moderate, and 5 were mild. cGVHD was initially diagnosed at a mean of 192 days post-transplant. The median number of organ systems involved was 3 (range, 1-6). Seventeen patients (46%) had overlap syndrome.
The researchers found that RTEs as a percentage of CD4 T cells were significantly lower at day 100 in patients with cGVHD than in controls—7.8% and 13.5%, respectively (P=0.007). The difference between controls and patients with late acute GVHD was not significant—13.5% and 9.4%, respectively (P=0.08).
Treg RTEs as a percentage of all Tregs were also significantly lower at day 100 in patients with cGVHD than in controls—6.4% and 13.2%, respectively (P=0.002). Again, the difference between controls and patients with late acute GVHD was not significant—13.2% and 9.1%, respectively (P=0.06).
However, further analysis revealed that percentages of RTEs and Treg RTEs were significantly lower at day 100 in patients who developed any type of GVHD after day 100.
The percentage of RTEs was 13.5% in controls and 8.5% in patients with any GVHD after day 100 (P=0.009). The percentage of Treg RTEs was 13.2% and 7.6%, respectively (P=0.004).
“Both recent thymic emigrants and Treg RTEs at day 100 are prognostic biomarkers for chronic graft-vs-host disease in children in this large, multi-institutional, prospective trial,” Dr Cuvelier said in closing.
“Unlike adults, in children, RTEs are proportionally lower, not higher, in patients that later develop chronic GVHD compared to no chronic GVHD. This may suggest that thymic dysfunction and thymic output may play a greater role in chronic GVHD development in children compared to adults.”
To expand upon this research, Dr Cuvelier and his colleagues are planning to begin model building using prognostic cellular and plasma biomarkers at day 100 to determine high-risk profiles for cGVHD.
1. Greinix HT et al; CD19+CD21low B Cells and CD4+CD45RA+CD31+ T Cells Correlate with First Diagnosis of Chronic Graft-versus-Host Disease. BBMT 2015; 21(2):250-258.
2. Li AM et al. An Early Naïve T Cell Population Lacking PD1 Expression at Day 100 As A Prognostic Biomarker of Chronic GVHD. TSS 2017; 210.6.
SALT LAKE CITY—Researchers say they have identified prognostic biomarkers for chronic graft-vs-host disease (cGVHD) in children.
The group found that recent thymic emigrants (RTEs) and regulatory T cells expressing CD31 and CD45RA (Treg RTEs) were significantly lower at day 100 after transplant in patients who developed cGVHD.
Because prior research indicated that RTEs are higher in adults with cGVHD, the researchers concluded that thymic function may play a bigger role in cGVHD development for children than for adults.
Geoff D.E. Cuvelier, MD, of CancerCare Manitoba in Winnipeg, Canada, presented these findings at the 2018 BMT Tandem Meetings (abstract 104).
“Our group became interested in these populations of recent thymic emigrants when 2 adult studies1,2 . . . showed that higher proportions of recent thymic emigrants at day 100 were prognostic for the development of chronic graft-vs-host disease,” Dr Cuvelier said.
This led his group to evaluate whether RTEs (CD4+CD45RA+CD31+ T cells), as well as Treg RTEs—Tregs (CD4+CD25+CD127Low) that co-express naïve and recently emigrated markers (CD45RA+CD31+)—are prognostic for pediatric cGVHD at day 100 after allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers’ study enrolled patients younger than 18 years of age who underwent allo-HSCT to treat malignant and non-malignant diseases. There were 144 patients who had 1 year of follow-up after allo-HSCT.
Thirty-seven of the patients (25.7%) had cGVHD, and 34 (23.6%) had late acute GVHD (post-day 100). The remaining 73 patients (50.7%) had neither cGVHD nor late acute GVHD, so they served as controls.
Twenty cases of cGVHD were severe, 12 were moderate, and 5 were mild. cGVHD was initially diagnosed at a mean of 192 days post-transplant. The median number of organ systems involved was 3 (range, 1-6). Seventeen patients (46%) had overlap syndrome.
The researchers found that RTEs as a percentage of CD4 T cells were significantly lower at day 100 in patients with cGVHD than in controls—7.8% and 13.5%, respectively (P=0.007). The difference between controls and patients with late acute GVHD was not significant—13.5% and 9.4%, respectively (P=0.08).
Treg RTEs as a percentage of all Tregs were also significantly lower at day 100 in patients with cGVHD than in controls—6.4% and 13.2%, respectively (P=0.002). Again, the difference between controls and patients with late acute GVHD was not significant—13.2% and 9.1%, respectively (P=0.06).
However, further analysis revealed that percentages of RTEs and Treg RTEs were significantly lower at day 100 in patients who developed any type of GVHD after day 100.
The percentage of RTEs was 13.5% in controls and 8.5% in patients with any GVHD after day 100 (P=0.009). The percentage of Treg RTEs was 13.2% and 7.6%, respectively (P=0.004).
“Both recent thymic emigrants and Treg RTEs at day 100 are prognostic biomarkers for chronic graft-vs-host disease in children in this large, multi-institutional, prospective trial,” Dr Cuvelier said in closing.
“Unlike adults, in children, RTEs are proportionally lower, not higher, in patients that later develop chronic GVHD compared to no chronic GVHD. This may suggest that thymic dysfunction and thymic output may play a greater role in chronic GVHD development in children compared to adults.”
To expand upon this research, Dr Cuvelier and his colleagues are planning to begin model building using prognostic cellular and plasma biomarkers at day 100 to determine high-risk profiles for cGVHD.
1. Greinix HT et al; CD19+CD21low B Cells and CD4+CD45RA+CD31+ T Cells Correlate with First Diagnosis of Chronic Graft-versus-Host Disease. BBMT 2015; 21(2):250-258.
2. Li AM et al. An Early Naïve T Cell Population Lacking PD1 Expression at Day 100 As A Prognostic Biomarker of Chronic GVHD. TSS 2017; 210.6.
SALT LAKE CITY—Researchers say they have identified prognostic biomarkers for chronic graft-vs-host disease (cGVHD) in children.
The group found that recent thymic emigrants (RTEs) and regulatory T cells expressing CD31 and CD45RA (Treg RTEs) were significantly lower at day 100 after transplant in patients who developed cGVHD.
Because prior research indicated that RTEs are higher in adults with cGVHD, the researchers concluded that thymic function may play a bigger role in cGVHD development for children than for adults.
Geoff D.E. Cuvelier, MD, of CancerCare Manitoba in Winnipeg, Canada, presented these findings at the 2018 BMT Tandem Meetings (abstract 104).
“Our group became interested in these populations of recent thymic emigrants when 2 adult studies1,2 . . . showed that higher proportions of recent thymic emigrants at day 100 were prognostic for the development of chronic graft-vs-host disease,” Dr Cuvelier said.
This led his group to evaluate whether RTEs (CD4+CD45RA+CD31+ T cells), as well as Treg RTEs—Tregs (CD4+CD25+CD127Low) that co-express naïve and recently emigrated markers (CD45RA+CD31+)—are prognostic for pediatric cGVHD at day 100 after allogeneic hematopoietic stem cell transplant (allo-HSCT).
The researchers’ study enrolled patients younger than 18 years of age who underwent allo-HSCT to treat malignant and non-malignant diseases. There were 144 patients who had 1 year of follow-up after allo-HSCT.
Thirty-seven of the patients (25.7%) had cGVHD, and 34 (23.6%) had late acute GVHD (post-day 100). The remaining 73 patients (50.7%) had neither cGVHD nor late acute GVHD, so they served as controls.
Twenty cases of cGVHD were severe, 12 were moderate, and 5 were mild. cGVHD was initially diagnosed at a mean of 192 days post-transplant. The median number of organ systems involved was 3 (range, 1-6). Seventeen patients (46%) had overlap syndrome.
The researchers found that RTEs as a percentage of CD4 T cells were significantly lower at day 100 in patients with cGVHD than in controls—7.8% and 13.5%, respectively (P=0.007). The difference between controls and patients with late acute GVHD was not significant—13.5% and 9.4%, respectively (P=0.08).
Treg RTEs as a percentage of all Tregs were also significantly lower at day 100 in patients with cGVHD than in controls—6.4% and 13.2%, respectively (P=0.002). Again, the difference between controls and patients with late acute GVHD was not significant—13.2% and 9.1%, respectively (P=0.06).
However, further analysis revealed that percentages of RTEs and Treg RTEs were significantly lower at day 100 in patients who developed any type of GVHD after day 100.
The percentage of RTEs was 13.5% in controls and 8.5% in patients with any GVHD after day 100 (P=0.009). The percentage of Treg RTEs was 13.2% and 7.6%, respectively (P=0.004).
“Both recent thymic emigrants and Treg RTEs at day 100 are prognostic biomarkers for chronic graft-vs-host disease in children in this large, multi-institutional, prospective trial,” Dr Cuvelier said in closing.
“Unlike adults, in children, RTEs are proportionally lower, not higher, in patients that later develop chronic GVHD compared to no chronic GVHD. This may suggest that thymic dysfunction and thymic output may play a greater role in chronic GVHD development in children compared to adults.”
To expand upon this research, Dr Cuvelier and his colleagues are planning to begin model building using prognostic cellular and plasma biomarkers at day 100 to determine high-risk profiles for cGVHD.
1. Greinix HT et al; CD19+CD21low B Cells and CD4+CD45RA+CD31+ T Cells Correlate with First Diagnosis of Chronic Graft-versus-Host Disease. BBMT 2015; 21(2):250-258.
2. Li AM et al. An Early Naïve T Cell Population Lacking PD1 Expression at Day 100 As A Prognostic Biomarker of Chronic GVHD. TSS 2017; 210.6.