User login
American College of Cardiology (ACC): Cardiovascular Conference at Snowmass
Controversies in dual antiplatelet therapy post PCI
SNOWMASS, COLO. – Wide local variation in the guideline-recommended use of low-dose aspirin as part of dual antiplatelet therapy after coronary stent implantation appears to be a prime target for a quality improvement effort.
American College of Cardiology/American Heart Association guidelines recommend aspirin at 81 mg/day along with an oral thienopyridine for maintenance therapy after percutaneous coronary intervention (PCI). This Class IIa/Level of Evidence B recommendation for preferential use of low- rather than high-dose aspirin is based upon the results of the OASIS 7 study (N. Engl. J. Med. 2010;354:1706-17) and other randomized trials that demonstrate that low- and high-dose aspirin (300-325 mg/day) are equally effective in reducing ischemic complications after PCI but that high-dose aspirin is associated with an increased risk of bleeding, Dr. Patrick T. O’Gara noted at the Annual Cardiovascular Conference at Snowmass.
Yet in a contemporary series of more than 23,000 U.S. patients enrolled in the major ongoing Dual Antiplatelet Therapy Study, only 28% were placed on low-dose aspirin at discharge after PCI; the rest got high-dose aspirin as part of their dual antiplatelet therapy (DAPT). In contrast, 90% of study participants from other countries got low-dose aspirin for their DAPT, commented Dr. O’Gara, who is ACC president-elect and professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, both in Boston.
The DAPT Study investigators determined that patient characteristics explained a mere 1.6% of the total variation in aspirin dosing. Site of enrollment accounted for 46% of the unexplained variation (Am. J. Cardiol. 201;113:1146-52).
The optimal duration of DAPT after PCI with placement of a drug-eluting stent remains unclear. Current guidelines call for at least 12 months of DAPT. The massive DAPT Study is designed to learn whether longer than 12 months is better. Participants were placed on 12 months of aspirin plus a thienopyridine, then randomized to an additional 18 months of DAPT or to aspirin plus placebo. The trial includes a variety of stents and indications for implantation. Results are expected later this year.
In the meantime, Dr. O’Gara said, the use of more than 12 months of DAPT is highly variable around the world. Studies suggest that at 3 years post-PCI, 40%-50% of North American patients remain on DAPT compared to about 10% of patients in Europe and elsewhere.
The ACC/AHA guidelines state as a relatively weak Class IIb/Level of Evidence C recommendation that continuation of DAPT beyond 12 months "may be considered" in drug-eluting stent recipients. Until the results of the DAPT Study become available to provide further guidance, however, Dr. O’Gara urged his colleagues to weigh this decision carefully on a case by case basis.
"The duration of DAPT is uncertain, but if you choose to continue therapy beyond 12 months, I think you need to be aware of the increasing number of trials that show no benefit of doing that – and an excess hazard of bleeding by doing so," he cautioned.
Dr. O’Gara cited three such major randomized trials totaling more than 6,100 patients: the Italian PRODIGY trial (Circulation 2012;125:2015-26), in which patients had near-identical rates of the 2-year composite of all-cause mortality, MI, or cerebrovascular accident regardless of whether they were randomized to 6 or 24 months of DAPT; the Korean combined REAL-LATE and ZEST-LATE trials (N. Engl. J. Med. 2010;362:1374-82), in which 12 and 24 months of DAPT resulted in similar rates of MI or cardiac death at 2 years; and EXCELLENT, in which 12 months of DAPT proved no better than 6 in terms of the combined endpoint of cardiac death, MI, or target vessel revascularization (Circulation 2012;125:505-13).
Moreover, a secondary analysis of the Korean trials found a 2.96-fold increased risk of Thrombosis in Myocardial Infarction major bleeding in patients on DAPT for longer than 12 months. And PRODIGY investigators found a 2.7-fold increased major bleeding risk with 24 as compared to 6 months of DAPT.
Further uncertainty regarding the optimal duration of DAPT comes from the OPTIMIZE trial, in which 3,119 Brazilian patients with low-risk acute coronary syndrome or stable coronary artery disease received a zotarolimus-eluting stent and were randomized to 3 or 12 months of DAPT. There was no difference between the two groups in the combined endpoint of all-cause mortality, MI, stroke, or major bleeding (JAMA 2013;310:2510-22).
"Interestingly enough, in Europe the zotarolimus-eluting stent has achieved approval for a 3-month course of dual antiplatelet therapy," Dr. O’Gara said.
He reported having no financial conflicts.
SNOWMASS, COLO. – Wide local variation in the guideline-recommended use of low-dose aspirin as part of dual antiplatelet therapy after coronary stent implantation appears to be a prime target for a quality improvement effort.
American College of Cardiology/American Heart Association guidelines recommend aspirin at 81 mg/day along with an oral thienopyridine for maintenance therapy after percutaneous coronary intervention (PCI). This Class IIa/Level of Evidence B recommendation for preferential use of low- rather than high-dose aspirin is based upon the results of the OASIS 7 study (N. Engl. J. Med. 2010;354:1706-17) and other randomized trials that demonstrate that low- and high-dose aspirin (300-325 mg/day) are equally effective in reducing ischemic complications after PCI but that high-dose aspirin is associated with an increased risk of bleeding, Dr. Patrick T. O’Gara noted at the Annual Cardiovascular Conference at Snowmass.
Yet in a contemporary series of more than 23,000 U.S. patients enrolled in the major ongoing Dual Antiplatelet Therapy Study, only 28% were placed on low-dose aspirin at discharge after PCI; the rest got high-dose aspirin as part of their dual antiplatelet therapy (DAPT). In contrast, 90% of study participants from other countries got low-dose aspirin for their DAPT, commented Dr. O’Gara, who is ACC president-elect and professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, both in Boston.
The DAPT Study investigators determined that patient characteristics explained a mere 1.6% of the total variation in aspirin dosing. Site of enrollment accounted for 46% of the unexplained variation (Am. J. Cardiol. 201;113:1146-52).
The optimal duration of DAPT after PCI with placement of a drug-eluting stent remains unclear. Current guidelines call for at least 12 months of DAPT. The massive DAPT Study is designed to learn whether longer than 12 months is better. Participants were placed on 12 months of aspirin plus a thienopyridine, then randomized to an additional 18 months of DAPT or to aspirin plus placebo. The trial includes a variety of stents and indications for implantation. Results are expected later this year.
In the meantime, Dr. O’Gara said, the use of more than 12 months of DAPT is highly variable around the world. Studies suggest that at 3 years post-PCI, 40%-50% of North American patients remain on DAPT compared to about 10% of patients in Europe and elsewhere.
The ACC/AHA guidelines state as a relatively weak Class IIb/Level of Evidence C recommendation that continuation of DAPT beyond 12 months "may be considered" in drug-eluting stent recipients. Until the results of the DAPT Study become available to provide further guidance, however, Dr. O’Gara urged his colleagues to weigh this decision carefully on a case by case basis.
"The duration of DAPT is uncertain, but if you choose to continue therapy beyond 12 months, I think you need to be aware of the increasing number of trials that show no benefit of doing that – and an excess hazard of bleeding by doing so," he cautioned.
Dr. O’Gara cited three such major randomized trials totaling more than 6,100 patients: the Italian PRODIGY trial (Circulation 2012;125:2015-26), in which patients had near-identical rates of the 2-year composite of all-cause mortality, MI, or cerebrovascular accident regardless of whether they were randomized to 6 or 24 months of DAPT; the Korean combined REAL-LATE and ZEST-LATE trials (N. Engl. J. Med. 2010;362:1374-82), in which 12 and 24 months of DAPT resulted in similar rates of MI or cardiac death at 2 years; and EXCELLENT, in which 12 months of DAPT proved no better than 6 in terms of the combined endpoint of cardiac death, MI, or target vessel revascularization (Circulation 2012;125:505-13).
Moreover, a secondary analysis of the Korean trials found a 2.96-fold increased risk of Thrombosis in Myocardial Infarction major bleeding in patients on DAPT for longer than 12 months. And PRODIGY investigators found a 2.7-fold increased major bleeding risk with 24 as compared to 6 months of DAPT.
Further uncertainty regarding the optimal duration of DAPT comes from the OPTIMIZE trial, in which 3,119 Brazilian patients with low-risk acute coronary syndrome or stable coronary artery disease received a zotarolimus-eluting stent and were randomized to 3 or 12 months of DAPT. There was no difference between the two groups in the combined endpoint of all-cause mortality, MI, stroke, or major bleeding (JAMA 2013;310:2510-22).
"Interestingly enough, in Europe the zotarolimus-eluting stent has achieved approval for a 3-month course of dual antiplatelet therapy," Dr. O’Gara said.
He reported having no financial conflicts.
SNOWMASS, COLO. – Wide local variation in the guideline-recommended use of low-dose aspirin as part of dual antiplatelet therapy after coronary stent implantation appears to be a prime target for a quality improvement effort.
American College of Cardiology/American Heart Association guidelines recommend aspirin at 81 mg/day along with an oral thienopyridine for maintenance therapy after percutaneous coronary intervention (PCI). This Class IIa/Level of Evidence B recommendation for preferential use of low- rather than high-dose aspirin is based upon the results of the OASIS 7 study (N. Engl. J. Med. 2010;354:1706-17) and other randomized trials that demonstrate that low- and high-dose aspirin (300-325 mg/day) are equally effective in reducing ischemic complications after PCI but that high-dose aspirin is associated with an increased risk of bleeding, Dr. Patrick T. O’Gara noted at the Annual Cardiovascular Conference at Snowmass.
Yet in a contemporary series of more than 23,000 U.S. patients enrolled in the major ongoing Dual Antiplatelet Therapy Study, only 28% were placed on low-dose aspirin at discharge after PCI; the rest got high-dose aspirin as part of their dual antiplatelet therapy (DAPT). In contrast, 90% of study participants from other countries got low-dose aspirin for their DAPT, commented Dr. O’Gara, who is ACC president-elect and professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, both in Boston.
The DAPT Study investigators determined that patient characteristics explained a mere 1.6% of the total variation in aspirin dosing. Site of enrollment accounted for 46% of the unexplained variation (Am. J. Cardiol. 201;113:1146-52).
The optimal duration of DAPT after PCI with placement of a drug-eluting stent remains unclear. Current guidelines call for at least 12 months of DAPT. The massive DAPT Study is designed to learn whether longer than 12 months is better. Participants were placed on 12 months of aspirin plus a thienopyridine, then randomized to an additional 18 months of DAPT or to aspirin plus placebo. The trial includes a variety of stents and indications for implantation. Results are expected later this year.
In the meantime, Dr. O’Gara said, the use of more than 12 months of DAPT is highly variable around the world. Studies suggest that at 3 years post-PCI, 40%-50% of North American patients remain on DAPT compared to about 10% of patients in Europe and elsewhere.
The ACC/AHA guidelines state as a relatively weak Class IIb/Level of Evidence C recommendation that continuation of DAPT beyond 12 months "may be considered" in drug-eluting stent recipients. Until the results of the DAPT Study become available to provide further guidance, however, Dr. O’Gara urged his colleagues to weigh this decision carefully on a case by case basis.
"The duration of DAPT is uncertain, but if you choose to continue therapy beyond 12 months, I think you need to be aware of the increasing number of trials that show no benefit of doing that – and an excess hazard of bleeding by doing so," he cautioned.
Dr. O’Gara cited three such major randomized trials totaling more than 6,100 patients: the Italian PRODIGY trial (Circulation 2012;125:2015-26), in which patients had near-identical rates of the 2-year composite of all-cause mortality, MI, or cerebrovascular accident regardless of whether they were randomized to 6 or 24 months of DAPT; the Korean combined REAL-LATE and ZEST-LATE trials (N. Engl. J. Med. 2010;362:1374-82), in which 12 and 24 months of DAPT resulted in similar rates of MI or cardiac death at 2 years; and EXCELLENT, in which 12 months of DAPT proved no better than 6 in terms of the combined endpoint of cardiac death, MI, or target vessel revascularization (Circulation 2012;125:505-13).
Moreover, a secondary analysis of the Korean trials found a 2.96-fold increased risk of Thrombosis in Myocardial Infarction major bleeding in patients on DAPT for longer than 12 months. And PRODIGY investigators found a 2.7-fold increased major bleeding risk with 24 as compared to 6 months of DAPT.
Further uncertainty regarding the optimal duration of DAPT comes from the OPTIMIZE trial, in which 3,119 Brazilian patients with low-risk acute coronary syndrome or stable coronary artery disease received a zotarolimus-eluting stent and were randomized to 3 or 12 months of DAPT. There was no difference between the two groups in the combined endpoint of all-cause mortality, MI, stroke, or major bleeding (JAMA 2013;310:2510-22).
"Interestingly enough, in Europe the zotarolimus-eluting stent has achieved approval for a 3-month course of dual antiplatelet therapy," Dr. O’Gara said.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Frailty assessment central to TAVR decision
SNOWMASS, COLO. – Transcatheter aortic valve replacement in nonsurgical candidates with severe symptomatic aortic stenosis carries a hefty price tag of $116,500 per quality-adjusted life-year gained over medical management.
That’s the bottom line in a cost-effectiveness study led by cardiologist Dr. Mark A. Hlatky. The investigators applied data on the costs and benefits of transfemoral transcatheter aortic valve replacement (TAVR) as documented in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial in their Markov model involving a hypothetical patient cohort. The estimated incremental cost-effectiveness of $116,500 per quality-adjusted life-year gained is well in excess of the $50,000 figure widely accepted by health policy makers as defining a cutoff for cost-effective therapy.
In this cost-effectiveness analysis (Circ. Cardiovasc. Qual. Outcomes 2013;6:419-28), TAVR boosted life expectancy by roughly 11 months, from 2.08 years with medical therapy to 2.93 years. Quality-adjusted life expectancy rose from 1.19 to 1.93 years. TAVR also resulted in 1.4 fewer hospitalizations than with medical management. However, undergoing TAVR rather than medical management raised the lifetime stroke risk from 1% to 11% and increased lifetime health care costs from $83,600 to $169,100, reported the group led by Dr. Hlatky, professor of health research and policy and also professor of medicine at Stanford (Calif.) University.
"This is a fascinating study," Dr. Karen P. Alexander said at the Annual Cardiovascular Conference at Snowmass. "I think the lesson here is that futility from a cost perspective is also something that should be in the discussion" regarding TAVR vs. medical therapy in patients with inoperable aortic stenosis.
She highlighted the Hlatky study in discussing the key role frailty assessment plays in considering TAVR. The study showed that the cost-effectiveness of TAVR is greater in patients with a lower burden of noncardiac disease, which is another way saying "those who are less frail."
This conclusion underscores a statement in the 2012 American College of Cardiology/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons expert consensus document on TAVR paraphrased by Dr. Alexander: Frailty will assume central importance in patient selection for TAVR by virtue of the extensive comorbidities in this population. Existing models do not have predictive variables of interest in high-risk patients. (J. Am. Coll. Cardiol. 2012;59:1200-54).
Dr. Alexander of Duke University in Durham, N.C., said frailty is important when considering TAVR because it has been shown to be associated with increased rates of post-TAVR 30-day morbidity and mortality, prolonged hospital length of stay, and 1-year mortality.
She defined frailty as a multisystem impairment resulting in reduced physiologic reserve and increased vulnerability to stress. Frailty is a physiologic phenotype associated with slow gait, weakness, weight loss, exhaustion, and a low daily activity level.
While the degree of a patient’s frailty is an important consideration in deciding on TAVR vs. medical management, frailty per se is no contraindication to the procedure. Indeed, the prevalence of frailty as defined simply by a baseline 5-meter walk time in excess of 6 seconds was 72% among the 7,710 TAVR patients, mean age 84 years, included in the recent first report of the comprehensive national STS/ACC Transcatheter Valve Therapy Registry (JAMA 2013;310:2069-77). That’s nearly twice the 38% prevalence among community-dwelling 85-year-olds, Dr. Alexander noted, citing data from the Canadian Study of Health and Aging (CMAJ 2011;183:e487-94).
More than 20 different frailty risk scores are now in circulation. Dr. Alexander is particularly enthusiastic about the frailty risk tool developed as part of the ACC’s new Championing Care for the Patient With Aortic Stenosis Initiative. It efficiently assesses five domains of frailty – slowness, weakness, malnutrition, inactivity with loss of independence, and malnutrition – and generates a clinically useful qualitative frailty rating. A patient with a high frailty score may not have sufficient life expectancy to obtain the benefits of TAVR.
With regard to treatment futility, Dr. Alexander observed that it can be defined as either lack of medical efficacy as judged by physicians or as lack of meaningful survival as judged by a patient’s personal values. Yet one in four Americans aged 75 years or older has given little or no thought to their own wishes for end-of-life medical therapy, according to a recent Pew Research Center survey.
The telephone survey, conducted last spring, included a representative sample of 1,994 U.S. adults. While 47% of respondents aged 75 years or older indicated they had given their own wishes for end-of-life medical care a great deal of thought, 25% said they had given the matter "not much or none." Reflection on those personal wishes needs to be part of the physician/patient discussion about TAVR, according to Dr. Alexander.
With regard to general views on end-of-life therapy, 74% of surveyed individuals age 75 and up declared there should be circumstances in which a patient should be allowed to die. Another 22% said medical staff should do everything possible to save a patient’s life under all circumstances.
Dr. Alexander reported serving as a consultant to Gilead and Pozen.
SNOWMASS, COLO. – Transcatheter aortic valve replacement in nonsurgical candidates with severe symptomatic aortic stenosis carries a hefty price tag of $116,500 per quality-adjusted life-year gained over medical management.
That’s the bottom line in a cost-effectiveness study led by cardiologist Dr. Mark A. Hlatky. The investigators applied data on the costs and benefits of transfemoral transcatheter aortic valve replacement (TAVR) as documented in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial in their Markov model involving a hypothetical patient cohort. The estimated incremental cost-effectiveness of $116,500 per quality-adjusted life-year gained is well in excess of the $50,000 figure widely accepted by health policy makers as defining a cutoff for cost-effective therapy.
In this cost-effectiveness analysis (Circ. Cardiovasc. Qual. Outcomes 2013;6:419-28), TAVR boosted life expectancy by roughly 11 months, from 2.08 years with medical therapy to 2.93 years. Quality-adjusted life expectancy rose from 1.19 to 1.93 years. TAVR also resulted in 1.4 fewer hospitalizations than with medical management. However, undergoing TAVR rather than medical management raised the lifetime stroke risk from 1% to 11% and increased lifetime health care costs from $83,600 to $169,100, reported the group led by Dr. Hlatky, professor of health research and policy and also professor of medicine at Stanford (Calif.) University.
"This is a fascinating study," Dr. Karen P. Alexander said at the Annual Cardiovascular Conference at Snowmass. "I think the lesson here is that futility from a cost perspective is also something that should be in the discussion" regarding TAVR vs. medical therapy in patients with inoperable aortic stenosis.
She highlighted the Hlatky study in discussing the key role frailty assessment plays in considering TAVR. The study showed that the cost-effectiveness of TAVR is greater in patients with a lower burden of noncardiac disease, which is another way saying "those who are less frail."
This conclusion underscores a statement in the 2012 American College of Cardiology/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons expert consensus document on TAVR paraphrased by Dr. Alexander: Frailty will assume central importance in patient selection for TAVR by virtue of the extensive comorbidities in this population. Existing models do not have predictive variables of interest in high-risk patients. (J. Am. Coll. Cardiol. 2012;59:1200-54).
Dr. Alexander of Duke University in Durham, N.C., said frailty is important when considering TAVR because it has been shown to be associated with increased rates of post-TAVR 30-day morbidity and mortality, prolonged hospital length of stay, and 1-year mortality.
She defined frailty as a multisystem impairment resulting in reduced physiologic reserve and increased vulnerability to stress. Frailty is a physiologic phenotype associated with slow gait, weakness, weight loss, exhaustion, and a low daily activity level.
While the degree of a patient’s frailty is an important consideration in deciding on TAVR vs. medical management, frailty per se is no contraindication to the procedure. Indeed, the prevalence of frailty as defined simply by a baseline 5-meter walk time in excess of 6 seconds was 72% among the 7,710 TAVR patients, mean age 84 years, included in the recent first report of the comprehensive national STS/ACC Transcatheter Valve Therapy Registry (JAMA 2013;310:2069-77). That’s nearly twice the 38% prevalence among community-dwelling 85-year-olds, Dr. Alexander noted, citing data from the Canadian Study of Health and Aging (CMAJ 2011;183:e487-94).
More than 20 different frailty risk scores are now in circulation. Dr. Alexander is particularly enthusiastic about the frailty risk tool developed as part of the ACC’s new Championing Care for the Patient With Aortic Stenosis Initiative. It efficiently assesses five domains of frailty – slowness, weakness, malnutrition, inactivity with loss of independence, and malnutrition – and generates a clinically useful qualitative frailty rating. A patient with a high frailty score may not have sufficient life expectancy to obtain the benefits of TAVR.
With regard to treatment futility, Dr. Alexander observed that it can be defined as either lack of medical efficacy as judged by physicians or as lack of meaningful survival as judged by a patient’s personal values. Yet one in four Americans aged 75 years or older has given little or no thought to their own wishes for end-of-life medical therapy, according to a recent Pew Research Center survey.
The telephone survey, conducted last spring, included a representative sample of 1,994 U.S. adults. While 47% of respondents aged 75 years or older indicated they had given their own wishes for end-of-life medical care a great deal of thought, 25% said they had given the matter "not much or none." Reflection on those personal wishes needs to be part of the physician/patient discussion about TAVR, according to Dr. Alexander.
With regard to general views on end-of-life therapy, 74% of surveyed individuals age 75 and up declared there should be circumstances in which a patient should be allowed to die. Another 22% said medical staff should do everything possible to save a patient’s life under all circumstances.
Dr. Alexander reported serving as a consultant to Gilead and Pozen.
SNOWMASS, COLO. – Transcatheter aortic valve replacement in nonsurgical candidates with severe symptomatic aortic stenosis carries a hefty price tag of $116,500 per quality-adjusted life-year gained over medical management.
That’s the bottom line in a cost-effectiveness study led by cardiologist Dr. Mark A. Hlatky. The investigators applied data on the costs and benefits of transfemoral transcatheter aortic valve replacement (TAVR) as documented in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial in their Markov model involving a hypothetical patient cohort. The estimated incremental cost-effectiveness of $116,500 per quality-adjusted life-year gained is well in excess of the $50,000 figure widely accepted by health policy makers as defining a cutoff for cost-effective therapy.
In this cost-effectiveness analysis (Circ. Cardiovasc. Qual. Outcomes 2013;6:419-28), TAVR boosted life expectancy by roughly 11 months, from 2.08 years with medical therapy to 2.93 years. Quality-adjusted life expectancy rose from 1.19 to 1.93 years. TAVR also resulted in 1.4 fewer hospitalizations than with medical management. However, undergoing TAVR rather than medical management raised the lifetime stroke risk from 1% to 11% and increased lifetime health care costs from $83,600 to $169,100, reported the group led by Dr. Hlatky, professor of health research and policy and also professor of medicine at Stanford (Calif.) University.
"This is a fascinating study," Dr. Karen P. Alexander said at the Annual Cardiovascular Conference at Snowmass. "I think the lesson here is that futility from a cost perspective is also something that should be in the discussion" regarding TAVR vs. medical therapy in patients with inoperable aortic stenosis.
She highlighted the Hlatky study in discussing the key role frailty assessment plays in considering TAVR. The study showed that the cost-effectiveness of TAVR is greater in patients with a lower burden of noncardiac disease, which is another way saying "those who are less frail."
This conclusion underscores a statement in the 2012 American College of Cardiology/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons expert consensus document on TAVR paraphrased by Dr. Alexander: Frailty will assume central importance in patient selection for TAVR by virtue of the extensive comorbidities in this population. Existing models do not have predictive variables of interest in high-risk patients. (J. Am. Coll. Cardiol. 2012;59:1200-54).
Dr. Alexander of Duke University in Durham, N.C., said frailty is important when considering TAVR because it has been shown to be associated with increased rates of post-TAVR 30-day morbidity and mortality, prolonged hospital length of stay, and 1-year mortality.
She defined frailty as a multisystem impairment resulting in reduced physiologic reserve and increased vulnerability to stress. Frailty is a physiologic phenotype associated with slow gait, weakness, weight loss, exhaustion, and a low daily activity level.
While the degree of a patient’s frailty is an important consideration in deciding on TAVR vs. medical management, frailty per se is no contraindication to the procedure. Indeed, the prevalence of frailty as defined simply by a baseline 5-meter walk time in excess of 6 seconds was 72% among the 7,710 TAVR patients, mean age 84 years, included in the recent first report of the comprehensive national STS/ACC Transcatheter Valve Therapy Registry (JAMA 2013;310:2069-77). That’s nearly twice the 38% prevalence among community-dwelling 85-year-olds, Dr. Alexander noted, citing data from the Canadian Study of Health and Aging (CMAJ 2011;183:e487-94).
More than 20 different frailty risk scores are now in circulation. Dr. Alexander is particularly enthusiastic about the frailty risk tool developed as part of the ACC’s new Championing Care for the Patient With Aortic Stenosis Initiative. It efficiently assesses five domains of frailty – slowness, weakness, malnutrition, inactivity with loss of independence, and malnutrition – and generates a clinically useful qualitative frailty rating. A patient with a high frailty score may not have sufficient life expectancy to obtain the benefits of TAVR.
With regard to treatment futility, Dr. Alexander observed that it can be defined as either lack of medical efficacy as judged by physicians or as lack of meaningful survival as judged by a patient’s personal values. Yet one in four Americans aged 75 years or older has given little or no thought to their own wishes for end-of-life medical therapy, according to a recent Pew Research Center survey.
The telephone survey, conducted last spring, included a representative sample of 1,994 U.S. adults. While 47% of respondents aged 75 years or older indicated they had given their own wishes for end-of-life medical care a great deal of thought, 25% said they had given the matter "not much or none." Reflection on those personal wishes needs to be part of the physician/patient discussion about TAVR, according to Dr. Alexander.
With regard to general views on end-of-life therapy, 74% of surveyed individuals age 75 and up declared there should be circumstances in which a patient should be allowed to die. Another 22% said medical staff should do everything possible to save a patient’s life under all circumstances.
Dr. Alexander reported serving as a consultant to Gilead and Pozen.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
What’s new in non-STEMI management
SNOWMASS, COLO. – An early invasive strategy is particularly beneficial in octogenarians with non–ST-segment elevation myocardial infarction, according to a recent study involving close to 1 million NSTEMI patients aged 80 years or older.
The very eldest are an understudied segment of the NSTEMI population, for whom an initial conservative strategy has been the dominant approach in daily practice.
"This is an important study. We can see that as you get older and older, by virtue of the fact that you have more and more coronary disease, probably you’re going to be better off with an invasive strategy, all other things being equal," Dr. David R. Holmes Jr. commented in highlighting the study at the Annual Cardiovascular Conference at Snowmass.
The study included 968,542 octogenarians hospitalized with NSTEMI during 2003-2010 and entered into the Nationwide Inpatient Sample. Eighty-three percent were managed via an initial conservative approach, with coronary angiography performed only in the event of hemodynamic or electrical instability, refractory angina despite optimal medical therapy, or a test result indicative of high risk. The other 17% underwent an early invasive approach, with angiography within 48 hours of presentation.
Octogenarians managed via an early invasive strategy were more often younger, obese, smokers, dyslipidemic, hypertensive, white, and male, and more likely to have known vascular disease. In a multivariate analysis adjusted for potential confounders, the early invasive strategy group had a 34% reduction in in-hospital mortality compared with the conservatively managed group. They also had a 37% lower rate of acute ischemic stroke, a 40% reduction in intracranial hemorrhage, a 37% lower risk of gastrointestinal bleeding, and a shorter length of stay by an average of half a day. On the other side of the ledger, they had a 2.1-fold increased rate of cardiogenic shock (Am. J. Med. 2013;126:1076-83).
Does time to cath lab matter?
Another recent study looked at the optimal time frame for taking an NSTEMI patient to the cardiac catheterization laboratory as part of an invasive strategy. This was a meta-analysis of seven randomized controlled trials totaling 5,370 NSTEMI patients, along with four observational studies with more than 77,000 NSTEMI patients. The conclusion: There is as yet no persuasive evidence that the time interval makes a difference in outcomes (Ann. Intern. Med. 2013;158:261-70).
"That’s the data that’s available. It doesn’t matter how quickly you get the patient to the cath lab within that first period of time. You just need to take them, whether it’s in 2 hours, 6 hours, or 18 hours," Dr. Holmes said.
This has important implications as we think about systems of care. If somebody comes into the hospital late on a Friday night, do you have to take them to the cath lab Friday night, or can you wait electively and take them tomorrow or potentially even Monday morning when everybody’s there?" commented Dr. Holmes, professor of medicine at the Mayo Clinic in Rochester, Minn.
GRACE and CRUSADE
The cornerstone of decision making as to whether to opt for an invasive versus a conservative strategy in a given NSTEMI patient involves application of a formal risk score. A plethora of these risk scoring systems are in use today. Which is the best choice for a cardiologist as an aid to decision making? A meta-analysis involving 36 studies with nearly 117,000 NSTEMI patients has concluded that the GRACE (Global Registry of Acute Cardiac Events) risk score (JAMA 2004;291:2727-33) is the best of the pack. It significantly outperformed the TIMI score, which is the other widely used scoring system, as well as others less widely known (Contemp. Clin. Trials 2012:33:507-14).
"GRACE looks like it performs better. We’ll need better ones in the future, of course. But at the present time, select GRACE for risk stratification," advised the cardiologist, adding that a Grace score app is available.
Despite the fact that physicians are diagnosing and treating NSTEMI earlier in its course, in large part because of the widespread use of troponin assays in the emergency department, NSTEMI is still associated with substantial long-term morbidity and mortality, particularly in the elderly. This was underscored in a recent analysis of 19,336 NSTEMI patients aged 65 years or older who underwent early catheterization and were included in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry.
Twenty-one percent of patients received medical management alone, 60.8% underwent percutaneous coronary intervention, and 18.2% had coronary artery bypass graft surgery. The 5-year unadjusted all-cause mortality rate was 50% in the medically managed group, 33.5% in older patients who underwent PCI, and 24.2% in those who underwent CABG surgery. The unadjusted 5-year rate of a composite of death, readmission for MI, or readmission for stroke was 62.4% with medical management, 44.9% with PCI, and 33% with CABG. The investigators concluded that long-term outcomes in elderly NSTEMI patients appear to be better in this large registry when revascularization is accomplished via CABG than with PCI. This sets the stage for future confirmatory trials (Circ. Cardiovasc. Qual. Outcomes 2013;6:323-32).
Dr. Holmes noted that the incidence of NSTEMI has climbed steadily while that of STEMI has declined over the past couple of decades, not just in the United States but worldwide. In Australia, for example, during 1993-2010 the adjusted incidence of NSTEMI increased by a whopping 315%, from 67 to 182 cases per 100,000 person-years, while the adjusted incidence of STEMI fell by 30% (Am. J. Cardiol. 2013;112:169-73).
"NSTEMI is clearly an annuity for all of cardiology," Dr. Holmes said. "The growth rate is increasing and it will continue to increase as we get older."
He reported having no conflicts of interest.
These studies collectively offer guidance in key management decisions for an invasive strategy for our NSTEMI patients, namely, the factor of age, the impact of timing, and risk stratification scores. Currently, the "less is more" approach is often taken for octogenarians, but a large sample size from this registry shows better results across a spectrum of outcomes even while adjusting for cofounders. This should prompt a reevaluation of current practice. Although the timing of an invasive approach in STEMI is defined in prior studies, this large meta-analysis tells us that timing in NSTEMI does not correlate with outcomes as long as angiography is pursued at some point in time, a very important conclusion.
Finally, although TIMI scoring systems are used at most institutions, the GRACE score performed even better, a surprising finding.
Taken in sum, these key studies should be followed up by randomized controlled trials to definitively answer these important questions for our NSTEMI patients.
Dr. Hiren Shah is an assistant professor of medicine in the Feinberg School of Medicine, Northwestern University, Chicago, and a medical director of the Medicine and Cardiac Telemetry Hospitalist Unit at Northwestern Memorial Hospital. He is on the advisory board of Hospitalist News.
These studies collectively offer guidance in key management decisions for an invasive strategy for our NSTEMI patients, namely, the factor of age, the impact of timing, and risk stratification scores. Currently, the "less is more" approach is often taken for octogenarians, but a large sample size from this registry shows better results across a spectrum of outcomes even while adjusting for cofounders. This should prompt a reevaluation of current practice. Although the timing of an invasive approach in STEMI is defined in prior studies, this large meta-analysis tells us that timing in NSTEMI does not correlate with outcomes as long as angiography is pursued at some point in time, a very important conclusion.
Finally, although TIMI scoring systems are used at most institutions, the GRACE score performed even better, a surprising finding.
Taken in sum, these key studies should be followed up by randomized controlled trials to definitively answer these important questions for our NSTEMI patients.
Dr. Hiren Shah is an assistant professor of medicine in the Feinberg School of Medicine, Northwestern University, Chicago, and a medical director of the Medicine and Cardiac Telemetry Hospitalist Unit at Northwestern Memorial Hospital. He is on the advisory board of Hospitalist News.
These studies collectively offer guidance in key management decisions for an invasive strategy for our NSTEMI patients, namely, the factor of age, the impact of timing, and risk stratification scores. Currently, the "less is more" approach is often taken for octogenarians, but a large sample size from this registry shows better results across a spectrum of outcomes even while adjusting for cofounders. This should prompt a reevaluation of current practice. Although the timing of an invasive approach in STEMI is defined in prior studies, this large meta-analysis tells us that timing in NSTEMI does not correlate with outcomes as long as angiography is pursued at some point in time, a very important conclusion.
Finally, although TIMI scoring systems are used at most institutions, the GRACE score performed even better, a surprising finding.
Taken in sum, these key studies should be followed up by randomized controlled trials to definitively answer these important questions for our NSTEMI patients.
Dr. Hiren Shah is an assistant professor of medicine in the Feinberg School of Medicine, Northwestern University, Chicago, and a medical director of the Medicine and Cardiac Telemetry Hospitalist Unit at Northwestern Memorial Hospital. He is on the advisory board of Hospitalist News.
SNOWMASS, COLO. – An early invasive strategy is particularly beneficial in octogenarians with non–ST-segment elevation myocardial infarction, according to a recent study involving close to 1 million NSTEMI patients aged 80 years or older.
The very eldest are an understudied segment of the NSTEMI population, for whom an initial conservative strategy has been the dominant approach in daily practice.
"This is an important study. We can see that as you get older and older, by virtue of the fact that you have more and more coronary disease, probably you’re going to be better off with an invasive strategy, all other things being equal," Dr. David R. Holmes Jr. commented in highlighting the study at the Annual Cardiovascular Conference at Snowmass.
The study included 968,542 octogenarians hospitalized with NSTEMI during 2003-2010 and entered into the Nationwide Inpatient Sample. Eighty-three percent were managed via an initial conservative approach, with coronary angiography performed only in the event of hemodynamic or electrical instability, refractory angina despite optimal medical therapy, or a test result indicative of high risk. The other 17% underwent an early invasive approach, with angiography within 48 hours of presentation.
Octogenarians managed via an early invasive strategy were more often younger, obese, smokers, dyslipidemic, hypertensive, white, and male, and more likely to have known vascular disease. In a multivariate analysis adjusted for potential confounders, the early invasive strategy group had a 34% reduction in in-hospital mortality compared with the conservatively managed group. They also had a 37% lower rate of acute ischemic stroke, a 40% reduction in intracranial hemorrhage, a 37% lower risk of gastrointestinal bleeding, and a shorter length of stay by an average of half a day. On the other side of the ledger, they had a 2.1-fold increased rate of cardiogenic shock (Am. J. Med. 2013;126:1076-83).
Does time to cath lab matter?
Another recent study looked at the optimal time frame for taking an NSTEMI patient to the cardiac catheterization laboratory as part of an invasive strategy. This was a meta-analysis of seven randomized controlled trials totaling 5,370 NSTEMI patients, along with four observational studies with more than 77,000 NSTEMI patients. The conclusion: There is as yet no persuasive evidence that the time interval makes a difference in outcomes (Ann. Intern. Med. 2013;158:261-70).
"That’s the data that’s available. It doesn’t matter how quickly you get the patient to the cath lab within that first period of time. You just need to take them, whether it’s in 2 hours, 6 hours, or 18 hours," Dr. Holmes said.
This has important implications as we think about systems of care. If somebody comes into the hospital late on a Friday night, do you have to take them to the cath lab Friday night, or can you wait electively and take them tomorrow or potentially even Monday morning when everybody’s there?" commented Dr. Holmes, professor of medicine at the Mayo Clinic in Rochester, Minn.
GRACE and CRUSADE
The cornerstone of decision making as to whether to opt for an invasive versus a conservative strategy in a given NSTEMI patient involves application of a formal risk score. A plethora of these risk scoring systems are in use today. Which is the best choice for a cardiologist as an aid to decision making? A meta-analysis involving 36 studies with nearly 117,000 NSTEMI patients has concluded that the GRACE (Global Registry of Acute Cardiac Events) risk score (JAMA 2004;291:2727-33) is the best of the pack. It significantly outperformed the TIMI score, which is the other widely used scoring system, as well as others less widely known (Contemp. Clin. Trials 2012:33:507-14).
"GRACE looks like it performs better. We’ll need better ones in the future, of course. But at the present time, select GRACE for risk stratification," advised the cardiologist, adding that a Grace score app is available.
Despite the fact that physicians are diagnosing and treating NSTEMI earlier in its course, in large part because of the widespread use of troponin assays in the emergency department, NSTEMI is still associated with substantial long-term morbidity and mortality, particularly in the elderly. This was underscored in a recent analysis of 19,336 NSTEMI patients aged 65 years or older who underwent early catheterization and were included in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry.
Twenty-one percent of patients received medical management alone, 60.8% underwent percutaneous coronary intervention, and 18.2% had coronary artery bypass graft surgery. The 5-year unadjusted all-cause mortality rate was 50% in the medically managed group, 33.5% in older patients who underwent PCI, and 24.2% in those who underwent CABG surgery. The unadjusted 5-year rate of a composite of death, readmission for MI, or readmission for stroke was 62.4% with medical management, 44.9% with PCI, and 33% with CABG. The investigators concluded that long-term outcomes in elderly NSTEMI patients appear to be better in this large registry when revascularization is accomplished via CABG than with PCI. This sets the stage for future confirmatory trials (Circ. Cardiovasc. Qual. Outcomes 2013;6:323-32).
Dr. Holmes noted that the incidence of NSTEMI has climbed steadily while that of STEMI has declined over the past couple of decades, not just in the United States but worldwide. In Australia, for example, during 1993-2010 the adjusted incidence of NSTEMI increased by a whopping 315%, from 67 to 182 cases per 100,000 person-years, while the adjusted incidence of STEMI fell by 30% (Am. J. Cardiol. 2013;112:169-73).
"NSTEMI is clearly an annuity for all of cardiology," Dr. Holmes said. "The growth rate is increasing and it will continue to increase as we get older."
He reported having no conflicts of interest.
SNOWMASS, COLO. – An early invasive strategy is particularly beneficial in octogenarians with non–ST-segment elevation myocardial infarction, according to a recent study involving close to 1 million NSTEMI patients aged 80 years or older.
The very eldest are an understudied segment of the NSTEMI population, for whom an initial conservative strategy has been the dominant approach in daily practice.
"This is an important study. We can see that as you get older and older, by virtue of the fact that you have more and more coronary disease, probably you’re going to be better off with an invasive strategy, all other things being equal," Dr. David R. Holmes Jr. commented in highlighting the study at the Annual Cardiovascular Conference at Snowmass.
The study included 968,542 octogenarians hospitalized with NSTEMI during 2003-2010 and entered into the Nationwide Inpatient Sample. Eighty-three percent were managed via an initial conservative approach, with coronary angiography performed only in the event of hemodynamic or electrical instability, refractory angina despite optimal medical therapy, or a test result indicative of high risk. The other 17% underwent an early invasive approach, with angiography within 48 hours of presentation.
Octogenarians managed via an early invasive strategy were more often younger, obese, smokers, dyslipidemic, hypertensive, white, and male, and more likely to have known vascular disease. In a multivariate analysis adjusted for potential confounders, the early invasive strategy group had a 34% reduction in in-hospital mortality compared with the conservatively managed group. They also had a 37% lower rate of acute ischemic stroke, a 40% reduction in intracranial hemorrhage, a 37% lower risk of gastrointestinal bleeding, and a shorter length of stay by an average of half a day. On the other side of the ledger, they had a 2.1-fold increased rate of cardiogenic shock (Am. J. Med. 2013;126:1076-83).
Does time to cath lab matter?
Another recent study looked at the optimal time frame for taking an NSTEMI patient to the cardiac catheterization laboratory as part of an invasive strategy. This was a meta-analysis of seven randomized controlled trials totaling 5,370 NSTEMI patients, along with four observational studies with more than 77,000 NSTEMI patients. The conclusion: There is as yet no persuasive evidence that the time interval makes a difference in outcomes (Ann. Intern. Med. 2013;158:261-70).
"That’s the data that’s available. It doesn’t matter how quickly you get the patient to the cath lab within that first period of time. You just need to take them, whether it’s in 2 hours, 6 hours, or 18 hours," Dr. Holmes said.
This has important implications as we think about systems of care. If somebody comes into the hospital late on a Friday night, do you have to take them to the cath lab Friday night, or can you wait electively and take them tomorrow or potentially even Monday morning when everybody’s there?" commented Dr. Holmes, professor of medicine at the Mayo Clinic in Rochester, Minn.
GRACE and CRUSADE
The cornerstone of decision making as to whether to opt for an invasive versus a conservative strategy in a given NSTEMI patient involves application of a formal risk score. A plethora of these risk scoring systems are in use today. Which is the best choice for a cardiologist as an aid to decision making? A meta-analysis involving 36 studies with nearly 117,000 NSTEMI patients has concluded that the GRACE (Global Registry of Acute Cardiac Events) risk score (JAMA 2004;291:2727-33) is the best of the pack. It significantly outperformed the TIMI score, which is the other widely used scoring system, as well as others less widely known (Contemp. Clin. Trials 2012:33:507-14).
"GRACE looks like it performs better. We’ll need better ones in the future, of course. But at the present time, select GRACE for risk stratification," advised the cardiologist, adding that a Grace score app is available.
Despite the fact that physicians are diagnosing and treating NSTEMI earlier in its course, in large part because of the widespread use of troponin assays in the emergency department, NSTEMI is still associated with substantial long-term morbidity and mortality, particularly in the elderly. This was underscored in a recent analysis of 19,336 NSTEMI patients aged 65 years or older who underwent early catheterization and were included in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry.
Twenty-one percent of patients received medical management alone, 60.8% underwent percutaneous coronary intervention, and 18.2% had coronary artery bypass graft surgery. The 5-year unadjusted all-cause mortality rate was 50% in the medically managed group, 33.5% in older patients who underwent PCI, and 24.2% in those who underwent CABG surgery. The unadjusted 5-year rate of a composite of death, readmission for MI, or readmission for stroke was 62.4% with medical management, 44.9% with PCI, and 33% with CABG. The investigators concluded that long-term outcomes in elderly NSTEMI patients appear to be better in this large registry when revascularization is accomplished via CABG than with PCI. This sets the stage for future confirmatory trials (Circ. Cardiovasc. Qual. Outcomes 2013;6:323-32).
Dr. Holmes noted that the incidence of NSTEMI has climbed steadily while that of STEMI has declined over the past couple of decades, not just in the United States but worldwide. In Australia, for example, during 1993-2010 the adjusted incidence of NSTEMI increased by a whopping 315%, from 67 to 182 cases per 100,000 person-years, while the adjusted incidence of STEMI fell by 30% (Am. J. Cardiol. 2013;112:169-73).
"NSTEMI is clearly an annuity for all of cardiology," Dr. Holmes said. "The growth rate is increasing and it will continue to increase as we get older."
He reported having no conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Calculate an STS score before all aortic valve replacements
SNOWMASS, COLO. – The Society of Thoracic Surgeons Predicted Risk of Mortality score draws criticism when it’s used to help decide whether a patient should undergo surgical or transcatheter aortic valve replacement, because the algorithm excludes plenty of information pertinent to that task. Yet for now it’s an indispensible tool for cardiologists and surgeons alike, Dr. Vinod H. Thourani asserted at the Annual Cardiovascular Conference at Snowmass.
"Calculate an STS score for all patients, as annoying as it is. The goal should be to fit the patient with the best operation, not to force the patient into one technique or the other. The STS score is the only thing we have right now. Work is underway on a new TAVR risk scoring system, but it’s not ready yet," said Dr. Thourani, associate director of cardiothoracic surgery at Emory University, Atlanta.
The STS score was originally developed to predict the risk of mortality in coronary artery bypass graft (CABG) patients. But despite the score’s limitations when applied to patients requiring aortic valve replacement, a new analysis of the massive STS national database demonstrates that the tool is surprisingly accurate for this purpose.
"In reality, the STS score does a pretty good job of predicting what you’re going to do in open surgery. Everybody poo-poos the score, but here we’ve got data on 142,000 patients undergoing isolated surgical aortic valve replacement, and it’s actually pretty close. So I think you can use the STS score for prediction of surgical valve mortality," according to Dr. Thourani.
Among the 141,905 patients in the STS database who underwent isolated surgical aortic valve replacement (SAVR) during roughly the past 6 years, 6% were high risk as defined by an STS predicted risk of mortality score greater than 8%. Another 14% were intermediate risk, with an STS score of 4%-8%. The remaining 80% were low risk, with an STS score of less than 4%.
In a soon-to-be-published report by Dr. Thourani and his coinvestigators, the median postoperative length of stay was 6.0 days in the group with a low-risk STS score, 8.0 days in the intermediate-risk patients, and 9.0 days in those with an STS score greater than 8%. Actual national in-hospital mortality in SAVR patients with an STS score of less than 4% was 1.4%, whereas the mean and median STS for predicted in-hospital mortality in this cohort was 1.7% and 1.5%, respectively. In-hospital mortality in the intermediate-risk group was 5.1%; the mean and median STS scores in this group were 5.5% and 5.2%. And in the high-risk group, in-hospital mortality was 11.8%, compared with 13.7% and 11.2% mean and median predicted rates based on STS scores.
At Emory and other multidisciplinary heart centers around the country, patients needing aortic valve replacement who have an STS score below 4% typically get SAVR with either a stented or sutureless valve. Intermediate-risk patients – those with an STS score of 4%-8% – get SAVR or are enrolled in a mid-risk TAVR clinical trial, provided it’s an option at that site. High-risk patients with an STS score greater than 8% have the option of an open or mini-SAVR, although Dr. Thourani said most of his high-risk patients now undergo TAVR. Extremely high-risk patients having an STS score greater than 15% aren’t candidates for surgery; their options are commercially available TAVR or palliation via balloon valvuloplasty and/or medical therapy.
Patients in need of aortic valve replacement who present to a multidisciplinary heart center undergo an extensive battery of tests aimed at helping the team decide whether SAVR or TAVR is best for that individual. These tests assess relevant factors not included in the STS score algorithm. For example, frailty assessment is not incorporated in the STS score, yet most patients in need of a new aortic valve are elderly. At Emory, patients being evaluated for aortic valve replacement undergo five different measures of frailty: gait speed, grip strength, activities of daily living assessment, nutrition, and the mini–mental status examination. If someone fails three of these five measures, Dr. Thourani rules out the option of SAVR.
Other routine tests include a computed tomography (CT) scan to evaluate the ascending aorta and femoral and iliac arteries for calcification, echocardiography to determine annular sizing, carotid duplex ultrasound, pulmonary function tests, and cardiac catheterization.
TAVR is the best option for patients with porcelain aorta, a hostile chest due to prior radiation therapy, end-stage renal disease, severe lung disease, advanced liver disease, prior CABG surgery with an internal mammary artery graft crossing the midline, more than two prior sternotomies, or moderate dementia.
Dementia is a major issue for patients in their 80s with aortic stenosis warranting valve replacement. Mildly demented patients are suitable for either SAVR or TAVR. Those with severe dementia aren’t candidates for either procedure and are best managed with medication or balloon valvuloplasty.
"We no longer operate on patients with moderate dementia. They sundown really badly. We’ve gone to TAVR in these patients," Dr. Thourani said.
He reported serving as a consultant to Edwards Lifesciences, Sorin, and St. Jude Medical.
SNOWMASS, COLO. – The Society of Thoracic Surgeons Predicted Risk of Mortality score draws criticism when it’s used to help decide whether a patient should undergo surgical or transcatheter aortic valve replacement, because the algorithm excludes plenty of information pertinent to that task. Yet for now it’s an indispensible tool for cardiologists and surgeons alike, Dr. Vinod H. Thourani asserted at the Annual Cardiovascular Conference at Snowmass.
"Calculate an STS score for all patients, as annoying as it is. The goal should be to fit the patient with the best operation, not to force the patient into one technique or the other. The STS score is the only thing we have right now. Work is underway on a new TAVR risk scoring system, but it’s not ready yet," said Dr. Thourani, associate director of cardiothoracic surgery at Emory University, Atlanta.
The STS score was originally developed to predict the risk of mortality in coronary artery bypass graft (CABG) patients. But despite the score’s limitations when applied to patients requiring aortic valve replacement, a new analysis of the massive STS national database demonstrates that the tool is surprisingly accurate for this purpose.
"In reality, the STS score does a pretty good job of predicting what you’re going to do in open surgery. Everybody poo-poos the score, but here we’ve got data on 142,000 patients undergoing isolated surgical aortic valve replacement, and it’s actually pretty close. So I think you can use the STS score for prediction of surgical valve mortality," according to Dr. Thourani.
Among the 141,905 patients in the STS database who underwent isolated surgical aortic valve replacement (SAVR) during roughly the past 6 years, 6% were high risk as defined by an STS predicted risk of mortality score greater than 8%. Another 14% were intermediate risk, with an STS score of 4%-8%. The remaining 80% were low risk, with an STS score of less than 4%.
In a soon-to-be-published report by Dr. Thourani and his coinvestigators, the median postoperative length of stay was 6.0 days in the group with a low-risk STS score, 8.0 days in the intermediate-risk patients, and 9.0 days in those with an STS score greater than 8%. Actual national in-hospital mortality in SAVR patients with an STS score of less than 4% was 1.4%, whereas the mean and median STS for predicted in-hospital mortality in this cohort was 1.7% and 1.5%, respectively. In-hospital mortality in the intermediate-risk group was 5.1%; the mean and median STS scores in this group were 5.5% and 5.2%. And in the high-risk group, in-hospital mortality was 11.8%, compared with 13.7% and 11.2% mean and median predicted rates based on STS scores.
At Emory and other multidisciplinary heart centers around the country, patients needing aortic valve replacement who have an STS score below 4% typically get SAVR with either a stented or sutureless valve. Intermediate-risk patients – those with an STS score of 4%-8% – get SAVR or are enrolled in a mid-risk TAVR clinical trial, provided it’s an option at that site. High-risk patients with an STS score greater than 8% have the option of an open or mini-SAVR, although Dr. Thourani said most of his high-risk patients now undergo TAVR. Extremely high-risk patients having an STS score greater than 15% aren’t candidates for surgery; their options are commercially available TAVR or palliation via balloon valvuloplasty and/or medical therapy.
Patients in need of aortic valve replacement who present to a multidisciplinary heart center undergo an extensive battery of tests aimed at helping the team decide whether SAVR or TAVR is best for that individual. These tests assess relevant factors not included in the STS score algorithm. For example, frailty assessment is not incorporated in the STS score, yet most patients in need of a new aortic valve are elderly. At Emory, patients being evaluated for aortic valve replacement undergo five different measures of frailty: gait speed, grip strength, activities of daily living assessment, nutrition, and the mini–mental status examination. If someone fails three of these five measures, Dr. Thourani rules out the option of SAVR.
Other routine tests include a computed tomography (CT) scan to evaluate the ascending aorta and femoral and iliac arteries for calcification, echocardiography to determine annular sizing, carotid duplex ultrasound, pulmonary function tests, and cardiac catheterization.
TAVR is the best option for patients with porcelain aorta, a hostile chest due to prior radiation therapy, end-stage renal disease, severe lung disease, advanced liver disease, prior CABG surgery with an internal mammary artery graft crossing the midline, more than two prior sternotomies, or moderate dementia.
Dementia is a major issue for patients in their 80s with aortic stenosis warranting valve replacement. Mildly demented patients are suitable for either SAVR or TAVR. Those with severe dementia aren’t candidates for either procedure and are best managed with medication or balloon valvuloplasty.
"We no longer operate on patients with moderate dementia. They sundown really badly. We’ve gone to TAVR in these patients," Dr. Thourani said.
He reported serving as a consultant to Edwards Lifesciences, Sorin, and St. Jude Medical.
SNOWMASS, COLO. – The Society of Thoracic Surgeons Predicted Risk of Mortality score draws criticism when it’s used to help decide whether a patient should undergo surgical or transcatheter aortic valve replacement, because the algorithm excludes plenty of information pertinent to that task. Yet for now it’s an indispensible tool for cardiologists and surgeons alike, Dr. Vinod H. Thourani asserted at the Annual Cardiovascular Conference at Snowmass.
"Calculate an STS score for all patients, as annoying as it is. The goal should be to fit the patient with the best operation, not to force the patient into one technique or the other. The STS score is the only thing we have right now. Work is underway on a new TAVR risk scoring system, but it’s not ready yet," said Dr. Thourani, associate director of cardiothoracic surgery at Emory University, Atlanta.
The STS score was originally developed to predict the risk of mortality in coronary artery bypass graft (CABG) patients. But despite the score’s limitations when applied to patients requiring aortic valve replacement, a new analysis of the massive STS national database demonstrates that the tool is surprisingly accurate for this purpose.
"In reality, the STS score does a pretty good job of predicting what you’re going to do in open surgery. Everybody poo-poos the score, but here we’ve got data on 142,000 patients undergoing isolated surgical aortic valve replacement, and it’s actually pretty close. So I think you can use the STS score for prediction of surgical valve mortality," according to Dr. Thourani.
Among the 141,905 patients in the STS database who underwent isolated surgical aortic valve replacement (SAVR) during roughly the past 6 years, 6% were high risk as defined by an STS predicted risk of mortality score greater than 8%. Another 14% were intermediate risk, with an STS score of 4%-8%. The remaining 80% were low risk, with an STS score of less than 4%.
In a soon-to-be-published report by Dr. Thourani and his coinvestigators, the median postoperative length of stay was 6.0 days in the group with a low-risk STS score, 8.0 days in the intermediate-risk patients, and 9.0 days in those with an STS score greater than 8%. Actual national in-hospital mortality in SAVR patients with an STS score of less than 4% was 1.4%, whereas the mean and median STS for predicted in-hospital mortality in this cohort was 1.7% and 1.5%, respectively. In-hospital mortality in the intermediate-risk group was 5.1%; the mean and median STS scores in this group were 5.5% and 5.2%. And in the high-risk group, in-hospital mortality was 11.8%, compared with 13.7% and 11.2% mean and median predicted rates based on STS scores.
At Emory and other multidisciplinary heart centers around the country, patients needing aortic valve replacement who have an STS score below 4% typically get SAVR with either a stented or sutureless valve. Intermediate-risk patients – those with an STS score of 4%-8% – get SAVR or are enrolled in a mid-risk TAVR clinical trial, provided it’s an option at that site. High-risk patients with an STS score greater than 8% have the option of an open or mini-SAVR, although Dr. Thourani said most of his high-risk patients now undergo TAVR. Extremely high-risk patients having an STS score greater than 15% aren’t candidates for surgery; their options are commercially available TAVR or palliation via balloon valvuloplasty and/or medical therapy.
Patients in need of aortic valve replacement who present to a multidisciplinary heart center undergo an extensive battery of tests aimed at helping the team decide whether SAVR or TAVR is best for that individual. These tests assess relevant factors not included in the STS score algorithm. For example, frailty assessment is not incorporated in the STS score, yet most patients in need of a new aortic valve are elderly. At Emory, patients being evaluated for aortic valve replacement undergo five different measures of frailty: gait speed, grip strength, activities of daily living assessment, nutrition, and the mini–mental status examination. If someone fails three of these five measures, Dr. Thourani rules out the option of SAVR.
Other routine tests include a computed tomography (CT) scan to evaluate the ascending aorta and femoral and iliac arteries for calcification, echocardiography to determine annular sizing, carotid duplex ultrasound, pulmonary function tests, and cardiac catheterization.
TAVR is the best option for patients with porcelain aorta, a hostile chest due to prior radiation therapy, end-stage renal disease, severe lung disease, advanced liver disease, prior CABG surgery with an internal mammary artery graft crossing the midline, more than two prior sternotomies, or moderate dementia.
Dementia is a major issue for patients in their 80s with aortic stenosis warranting valve replacement. Mildly demented patients are suitable for either SAVR or TAVR. Those with severe dementia aren’t candidates for either procedure and are best managed with medication or balloon valvuloplasty.
"We no longer operate on patients with moderate dementia. They sundown really badly. We’ve gone to TAVR in these patients," Dr. Thourani said.
He reported serving as a consultant to Edwards Lifesciences, Sorin, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Aldosterone agonists earn new respect in HF guidelines
SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
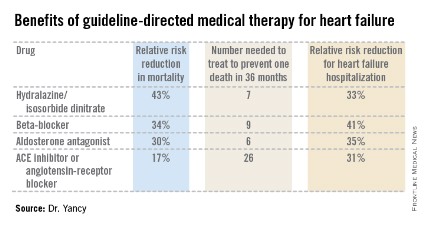
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).

"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the abbreviation GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis.
Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-239).
Dr. Yancy reported having no financial conflicts.
Dr. Jun Chiong, FCCP, comments: The new 2013 ACCF/AHA Guideline for the Management of Heart Failure provides a fresh and comprehensive guide to evaluation and management of heart failure patients. The guideline has new areas that are going to be quite helpful for the providers. The indications for aldosterone antagonists are broadened for symptomatic HFpEF patients NYHA class II, III, and IV patients. Creatinine values needed to be = 2.5 mg/dL in men or= 2.0 mg/dL in women, and potassium =5.0 mEq/L are highlighted along with the necessity for careful monitoring of potassium, renal function, and diuretic dosing at initiation follow-up. Routine combined use of an ACE inhibitor, ARB, and aldosterone antagonist is considered potentially harmful and is not recommended.
SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).

"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the abbreviation GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis.
Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-239).
Dr. Yancy reported having no financial conflicts.
Dr. Jun Chiong, FCCP, comments: The new 2013 ACCF/AHA Guideline for the Management of Heart Failure provides a fresh and comprehensive guide to evaluation and management of heart failure patients. The guideline has new areas that are going to be quite helpful for the providers. The indications for aldosterone antagonists are broadened for symptomatic HFpEF patients NYHA class II, III, and IV patients. Creatinine values needed to be = 2.5 mg/dL in men or= 2.0 mg/dL in women, and potassium =5.0 mEq/L are highlighted along with the necessity for careful monitoring of potassium, renal function, and diuretic dosing at initiation follow-up. Routine combined use of an ACE inhibitor, ARB, and aldosterone antagonist is considered potentially harmful and is not recommended.
SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).

"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the abbreviation GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis.
Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-239).
Dr. Yancy reported having no financial conflicts.
Dr. Jun Chiong, FCCP, comments: The new 2013 ACCF/AHA Guideline for the Management of Heart Failure provides a fresh and comprehensive guide to evaluation and management of heart failure patients. The guideline has new areas that are going to be quite helpful for the providers. The indications for aldosterone antagonists are broadened for symptomatic HFpEF patients NYHA class II, III, and IV patients. Creatinine values needed to be = 2.5 mg/dL in men or= 2.0 mg/dL in women, and potassium =5.0 mEq/L are highlighted along with the necessity for careful monitoring of potassium, renal function, and diuretic dosing at initiation follow-up. Routine combined use of an ACE inhibitor, ARB, and aldosterone antagonist is considered potentially harmful and is not recommended.
Minimalist transfemoral TAVR winning surgical converts
SNOWMASS, COLO. – Familiarity with the option of minimalist transfemoral transcatheter aortic valve replacement is causing some top surgeons to broaden their use of nonsurgical valve replacement.
"This minimalist transfemoral TAVR is something we’ve done quite a lot of. As a surgeon, I sort of hate to say it, but this to me has made a huge difference in whether I make a patient surgical or transcatheter," Dr. Vinod H. Thourani said at the Annual Cardiovascular Conference at Snowmass.
"It’s me and a cardiology resident doing a minimalist transfemoral TAVR in the cath lab in an awake patient with fentanyl and Versed [midazolam] and a 14- to 24-French sheath. There’s no incision and the patients don’t go to the ICU. Thirty to forty percent of them go straight to their private room after their valve is implanted, if their groin is okay in the postop cath lab area," explained Dr. Thourani, associate director of cardiothoracic surgery at Emory University, Atlanta.
In 200 patients who’ve undergone the procedure at the hands of Dr. Thourani and his Emory colleagues, there has been zero in-hospital mortality. Most patients are home in 2-3 days.
On the other hand, the surgical approach is seeing advances as well, he continued. One technologic development he’s particularly enthusiastic about is the surgical sutureless valve.
"This is a whole new class of valves. My cardiologists, when I call them and tell them I put a sutureless valve in their patient, have no clue what we’re talking about," according to the surgeon.
Two major U.S. clinical trials are ongoing for the investigational sutureless Sorin Perceval and Edwards Intuity valves. These truly sutureless valves are crimped. The surgeon performs an open sternotomy, cross clamps the aorta, makes an aortotomy, then telescopes the valve down through the aortotomy. The Intuity valve is deployed via a brief balloon inflation to size it properly. The Perceval valve contains nitinol, so all that the surgeon has to do is put warm saline on it and the valve starts working.
"On my last Edwards Intuity valve, just last week, the cross clamp time was 35 minutes. Just to give you some perspective, the cross clamp time for a stented valve is 60-65 minutes and about 90 minutes for a stentless valve," Dr. Thourani explained.
He serves as a consultant to Edwards Lifesciences, Sorin, and St. Jude Medical.
SNOWMASS, COLO. – Familiarity with the option of minimalist transfemoral transcatheter aortic valve replacement is causing some top surgeons to broaden their use of nonsurgical valve replacement.
"This minimalist transfemoral TAVR is something we’ve done quite a lot of. As a surgeon, I sort of hate to say it, but this to me has made a huge difference in whether I make a patient surgical or transcatheter," Dr. Vinod H. Thourani said at the Annual Cardiovascular Conference at Snowmass.
"It’s me and a cardiology resident doing a minimalist transfemoral TAVR in the cath lab in an awake patient with fentanyl and Versed [midazolam] and a 14- to 24-French sheath. There’s no incision and the patients don’t go to the ICU. Thirty to forty percent of them go straight to their private room after their valve is implanted, if their groin is okay in the postop cath lab area," explained Dr. Thourani, associate director of cardiothoracic surgery at Emory University, Atlanta.
In 200 patients who’ve undergone the procedure at the hands of Dr. Thourani and his Emory colleagues, there has been zero in-hospital mortality. Most patients are home in 2-3 days.
On the other hand, the surgical approach is seeing advances as well, he continued. One technologic development he’s particularly enthusiastic about is the surgical sutureless valve.
"This is a whole new class of valves. My cardiologists, when I call them and tell them I put a sutureless valve in their patient, have no clue what we’re talking about," according to the surgeon.
Two major U.S. clinical trials are ongoing for the investigational sutureless Sorin Perceval and Edwards Intuity valves. These truly sutureless valves are crimped. The surgeon performs an open sternotomy, cross clamps the aorta, makes an aortotomy, then telescopes the valve down through the aortotomy. The Intuity valve is deployed via a brief balloon inflation to size it properly. The Perceval valve contains nitinol, so all that the surgeon has to do is put warm saline on it and the valve starts working.
"On my last Edwards Intuity valve, just last week, the cross clamp time was 35 minutes. Just to give you some perspective, the cross clamp time for a stented valve is 60-65 minutes and about 90 minutes for a stentless valve," Dr. Thourani explained.
He serves as a consultant to Edwards Lifesciences, Sorin, and St. Jude Medical.
SNOWMASS, COLO. – Familiarity with the option of minimalist transfemoral transcatheter aortic valve replacement is causing some top surgeons to broaden their use of nonsurgical valve replacement.
"This minimalist transfemoral TAVR is something we’ve done quite a lot of. As a surgeon, I sort of hate to say it, but this to me has made a huge difference in whether I make a patient surgical or transcatheter," Dr. Vinod H. Thourani said at the Annual Cardiovascular Conference at Snowmass.
"It’s me and a cardiology resident doing a minimalist transfemoral TAVR in the cath lab in an awake patient with fentanyl and Versed [midazolam] and a 14- to 24-French sheath. There’s no incision and the patients don’t go to the ICU. Thirty to forty percent of them go straight to their private room after their valve is implanted, if their groin is okay in the postop cath lab area," explained Dr. Thourani, associate director of cardiothoracic surgery at Emory University, Atlanta.
In 200 patients who’ve undergone the procedure at the hands of Dr. Thourani and his Emory colleagues, there has been zero in-hospital mortality. Most patients are home in 2-3 days.
On the other hand, the surgical approach is seeing advances as well, he continued. One technologic development he’s particularly enthusiastic about is the surgical sutureless valve.
"This is a whole new class of valves. My cardiologists, when I call them and tell them I put a sutureless valve in their patient, have no clue what we’re talking about," according to the surgeon.
Two major U.S. clinical trials are ongoing for the investigational sutureless Sorin Perceval and Edwards Intuity valves. These truly sutureless valves are crimped. The surgeon performs an open sternotomy, cross clamps the aorta, makes an aortotomy, then telescopes the valve down through the aortotomy. The Intuity valve is deployed via a brief balloon inflation to size it properly. The Perceval valve contains nitinol, so all that the surgeon has to do is put warm saline on it and the valve starts working.
"On my last Edwards Intuity valve, just last week, the cross clamp time was 35 minutes. Just to give you some perspective, the cross clamp time for a stented valve is 60-65 minutes and about 90 minutes for a stentless valve," Dr. Thourani explained.
He serves as a consultant to Edwards Lifesciences, Sorin, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Physician/patient communication on ICDs deemed problematic
SNOWMASS, COLO. – Cardiologist-patient discussions at the time of decision making about implantable cardioverter-defibrillator therapy are fraught with a disturbing degree of misrepresentation and omission, according to a recent study involving patient focus groups and formal scrutiny of observed physician-patient interactions.
"Our study demonstrates that patient-physician communication about ICDs is characterized by patient misinformation and a lack of attention to psychosocial and long-term risks by the prescribing physicians. ... Training of cardiologists on information exchange with patients may promote informed decision making and preempt threats to patient quality of life," concluded Dr. Paul J. Hauptman and his coinvestigators at St. Louis University.
At the Annual Cardiovascular Conference at Snowmass, Dr. Clyde W. Yancy highlighted the Hauptman study for shining a spotlight on an area in which the quality of communication with patients apparently leaves much to be desired. The study has drawn interest at the federally funded Patient-Centered Outcomes Research Institute (PCORI), where Dr. Yancy, a former president of the American Heart Association, is part of the leadership. Dr. Joe V. Selby, PCORI executive director, recently announced plans to spend roughly $1 billion on patient-centered comparative effectiveness research projects over the next 2 years.
The Hauptman study involved eight focus groups with a total of 41 ICD recipients in three different metropolitan areas as well as observation of 11 cardiologists as they each conducted two discussions about ICDs with individual device candidates.
Trained observers faulted 18 of the 22 cardiologist-patient interviews because the cardiologists didn’t address, minimized, or outright denied quality of life issues and the long-term consequences of ICD therapy, including increased risks for anxiety and depression as well as for inappropriate shocks.
Among the actual statements by cardiologists extracted from the physician-patient discussions were these: "The ICD will only go off if you are in VT/VF," "Inadvertent shock is not detrimental," "Inappropriate shock ... almost never happens," and "These devices are well tested and rarely have problems, so don’t worry about it." Cardiologists frequently compared the ICD to a seat belt, a safety net, or "an ambulance that follows you around." The first mention of a quality of life issue occurred on average halfway through the preimplantation discussions, which averaged 24 minutes in length. Although an increased prevalence of depression secondary to inappropriate ICD discharge or change in body image has been well documented in multiple studies, this possibility was discussed in only 1 of the 22 physician-patient interactions.
"No cardiologist discussed the epidemiological or clinical data on the prevalence of actual lifesaving ICD shocks, the prevalence of patients who ever require a shock, or the risk for death, despite ICD shock," the investigators noted (JAMA Intern. Med. 2013;173:571-7).
In the 2-hour-long patient focus groups, which were conducted with a different population than in the observed cardiologist-patient discussions, only 2 of 41 patients with ICDs could recall preimplantation mention of the possibility of depression or other emotional consequences of having an ICD. Only 5 of 41 patients could recall having a preimplantation discussion about inappropriate shocks. Two remembered mention of the possibility of device recalls.
The small sample size is a limitation of this study. Nevertheless, these rather disheartening data constitute some of the little evidence available on the information exchange between patients and cardiologists surrounding decision-making about ICDs, noted Dr. Yancy, professor of medicine and of medical social sciences as well as chief of cardiology at Northwestern University, Chicago.
"It just continues to be very startling that when you sit down with patients and understand what prism they’re using to see the data, you see information like this," he commented.
Another speaker, Dr. Bernard J. Gersh, was less circumspect. He was left shaking his head following Dr. Yancy’s overview of the Hauptman study findings.
"I was absolutely flabbergasted by the ICD patient information data. I was amazed and disappointed," said Dr. Gersh, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Yancy reported having no financial conflicts. Dr. Gersh is on the advisory boards of St. Jude Medical and Boston Scientific.
SNOWMASS, COLO. – Cardiologist-patient discussions at the time of decision making about implantable cardioverter-defibrillator therapy are fraught with a disturbing degree of misrepresentation and omission, according to a recent study involving patient focus groups and formal scrutiny of observed physician-patient interactions.
"Our study demonstrates that patient-physician communication about ICDs is characterized by patient misinformation and a lack of attention to psychosocial and long-term risks by the prescribing physicians. ... Training of cardiologists on information exchange with patients may promote informed decision making and preempt threats to patient quality of life," concluded Dr. Paul J. Hauptman and his coinvestigators at St. Louis University.
At the Annual Cardiovascular Conference at Snowmass, Dr. Clyde W. Yancy highlighted the Hauptman study for shining a spotlight on an area in which the quality of communication with patients apparently leaves much to be desired. The study has drawn interest at the federally funded Patient-Centered Outcomes Research Institute (PCORI), where Dr. Yancy, a former president of the American Heart Association, is part of the leadership. Dr. Joe V. Selby, PCORI executive director, recently announced plans to spend roughly $1 billion on patient-centered comparative effectiveness research projects over the next 2 years.
The Hauptman study involved eight focus groups with a total of 41 ICD recipients in three different metropolitan areas as well as observation of 11 cardiologists as they each conducted two discussions about ICDs with individual device candidates.
Trained observers faulted 18 of the 22 cardiologist-patient interviews because the cardiologists didn’t address, minimized, or outright denied quality of life issues and the long-term consequences of ICD therapy, including increased risks for anxiety and depression as well as for inappropriate shocks.
Among the actual statements by cardiologists extracted from the physician-patient discussions were these: "The ICD will only go off if you are in VT/VF," "Inadvertent shock is not detrimental," "Inappropriate shock ... almost never happens," and "These devices are well tested and rarely have problems, so don’t worry about it." Cardiologists frequently compared the ICD to a seat belt, a safety net, or "an ambulance that follows you around." The first mention of a quality of life issue occurred on average halfway through the preimplantation discussions, which averaged 24 minutes in length. Although an increased prevalence of depression secondary to inappropriate ICD discharge or change in body image has been well documented in multiple studies, this possibility was discussed in only 1 of the 22 physician-patient interactions.
"No cardiologist discussed the epidemiological or clinical data on the prevalence of actual lifesaving ICD shocks, the prevalence of patients who ever require a shock, or the risk for death, despite ICD shock," the investigators noted (JAMA Intern. Med. 2013;173:571-7).
In the 2-hour-long patient focus groups, which were conducted with a different population than in the observed cardiologist-patient discussions, only 2 of 41 patients with ICDs could recall preimplantation mention of the possibility of depression or other emotional consequences of having an ICD. Only 5 of 41 patients could recall having a preimplantation discussion about inappropriate shocks. Two remembered mention of the possibility of device recalls.
The small sample size is a limitation of this study. Nevertheless, these rather disheartening data constitute some of the little evidence available on the information exchange between patients and cardiologists surrounding decision-making about ICDs, noted Dr. Yancy, professor of medicine and of medical social sciences as well as chief of cardiology at Northwestern University, Chicago.
"It just continues to be very startling that when you sit down with patients and understand what prism they’re using to see the data, you see information like this," he commented.
Another speaker, Dr. Bernard J. Gersh, was less circumspect. He was left shaking his head following Dr. Yancy’s overview of the Hauptman study findings.
"I was absolutely flabbergasted by the ICD patient information data. I was amazed and disappointed," said Dr. Gersh, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Yancy reported having no financial conflicts. Dr. Gersh is on the advisory boards of St. Jude Medical and Boston Scientific.
SNOWMASS, COLO. – Cardiologist-patient discussions at the time of decision making about implantable cardioverter-defibrillator therapy are fraught with a disturbing degree of misrepresentation and omission, according to a recent study involving patient focus groups and formal scrutiny of observed physician-patient interactions.
"Our study demonstrates that patient-physician communication about ICDs is characterized by patient misinformation and a lack of attention to psychosocial and long-term risks by the prescribing physicians. ... Training of cardiologists on information exchange with patients may promote informed decision making and preempt threats to patient quality of life," concluded Dr. Paul J. Hauptman and his coinvestigators at St. Louis University.
At the Annual Cardiovascular Conference at Snowmass, Dr. Clyde W. Yancy highlighted the Hauptman study for shining a spotlight on an area in which the quality of communication with patients apparently leaves much to be desired. The study has drawn interest at the federally funded Patient-Centered Outcomes Research Institute (PCORI), where Dr. Yancy, a former president of the American Heart Association, is part of the leadership. Dr. Joe V. Selby, PCORI executive director, recently announced plans to spend roughly $1 billion on patient-centered comparative effectiveness research projects over the next 2 years.
The Hauptman study involved eight focus groups with a total of 41 ICD recipients in three different metropolitan areas as well as observation of 11 cardiologists as they each conducted two discussions about ICDs with individual device candidates.
Trained observers faulted 18 of the 22 cardiologist-patient interviews because the cardiologists didn’t address, minimized, or outright denied quality of life issues and the long-term consequences of ICD therapy, including increased risks for anxiety and depression as well as for inappropriate shocks.
Among the actual statements by cardiologists extracted from the physician-patient discussions were these: "The ICD will only go off if you are in VT/VF," "Inadvertent shock is not detrimental," "Inappropriate shock ... almost never happens," and "These devices are well tested and rarely have problems, so don’t worry about it." Cardiologists frequently compared the ICD to a seat belt, a safety net, or "an ambulance that follows you around." The first mention of a quality of life issue occurred on average halfway through the preimplantation discussions, which averaged 24 minutes in length. Although an increased prevalence of depression secondary to inappropriate ICD discharge or change in body image has been well documented in multiple studies, this possibility was discussed in only 1 of the 22 physician-patient interactions.
"No cardiologist discussed the epidemiological or clinical data on the prevalence of actual lifesaving ICD shocks, the prevalence of patients who ever require a shock, or the risk for death, despite ICD shock," the investigators noted (JAMA Intern. Med. 2013;173:571-7).
In the 2-hour-long patient focus groups, which were conducted with a different population than in the observed cardiologist-patient discussions, only 2 of 41 patients with ICDs could recall preimplantation mention of the possibility of depression or other emotional consequences of having an ICD. Only 5 of 41 patients could recall having a preimplantation discussion about inappropriate shocks. Two remembered mention of the possibility of device recalls.
The small sample size is a limitation of this study. Nevertheless, these rather disheartening data constitute some of the little evidence available on the information exchange between patients and cardiologists surrounding decision-making about ICDs, noted Dr. Yancy, professor of medicine and of medical social sciences as well as chief of cardiology at Northwestern University, Chicago.
"It just continues to be very startling that when you sit down with patients and understand what prism they’re using to see the data, you see information like this," he commented.
Another speaker, Dr. Bernard J. Gersh, was less circumspect. He was left shaking his head following Dr. Yancy’s overview of the Hauptman study findings.
"I was absolutely flabbergasted by the ICD patient information data. I was amazed and disappointed," said Dr. Gersh, professor of medicine at the Mayo Clinic in Rochester, Minn.
Dr. Yancy reported having no financial conflicts. Dr. Gersh is on the advisory boards of St. Jude Medical and Boston Scientific.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Latest heart failure guidelines break new ground
SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).

"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the acronym GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis. Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-e239).
Dr. Yancy reported having no financial conflicts.
SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).

"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the acronym GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis. Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-e239).
Dr. Yancy reported having no financial conflicts.
SNOWMASS, COLO. – The latest heart failure guidelines from the American College of Cardiology/American Heart Association place a new emphasis on aldosterone antagonists as a central aspect of the management of symptomatic or previously symptomatic heart failure with reduced ejection fraction – while underscoring important caveats to their use.
Aldosterone antagonist therapy earns the strongest possible designation in the guidelines: a Class I/Level of Evidence A recommendation. This is based on data from multiple randomized trials showing that, used appropriately, these agents result in a 30% relative risk reduction in mortality and a 35% reduction in the relative risk of heart failure hospitalization, with a number needed to treat for 36 months of just six patients to prevent one additional death. Those figures place the aldosterone antagonists on a par with the other Class I/A heart failure medications – beta-blockers, ACE inhibitors or angiotensin receptor blockers, and hydralazine/isosorbide dinitrate in African Americans – in terms of benefits (see chart).

"These data are quite striking," Dr. Clyde W. Yancy observed in presenting highlights of the 2013 ACC/AHA guidelines at the Annual Cardiovascular Conference at Snowmass.
"For many years, we’ve functioned in a space where we thought there’s not that much we can do for heart failure, and I would now argue stridently against that. You can see the incredibly low numbers needed to treat here. Only a handful of patients need to be exposed to these therapies to derive a significant benefit on mortality. These are data we should incorporate in our clinical practice without exclusion," declared Dr. Yancy, who chaired the heart failure guideline-writing committee.
The important caveat regarding the aldosterone antagonists is that they should be used only in patients with an estimated glomerular filtration rate greater than 30 mL/min per 1.73 m2 and a serum potassium level below 5.0 mEq/dL. Otherwise that Class I/A recommendation plummets to III/B, meaning the treatment is inappropriate and potentially harmful, continued Dr. Yancy, professor of medicine and of medical social sciences and chief of cardiology at Northwestern University, Chicago.
The guidelines emphasize the imperative to implement what has come to be termed guideline-directed medical therapy, known by the acronym GDMT. The panel found persuasive an analysis showing that heart failure patients with reduced ejection fraction who were on two of seven evidence-based, guideline-directed management interventions had an adjusted 38% reduction in 2-year mortality risk compared with those on none or one, while those on three interventions had a 62% decrease in the odds of mortality and patients on four or more had mortality reductions of about 70% (J. Am. Heart Assoc. 2012;1:16-26).
The seven interventions are beta-blockers, ACE inhibitors or ARBs, aldosterone antagonists, anticoagulation for atrial fibrillation, cardiac resynchronization therapy, implantable cardioverter-defibrillators, and heart failure education for eligible patients.
The guidelines advise strongly against the combined use of an ACE inhibitor and ARB. It’s an either/or treatment strategy. Studies indicate there is no additive benefit with the combination, only an increased risk of side effects.
An important innovation in the guidelines is the new prominence afforded to heart failure with preserved ejection fraction, known as HFpEF (pronounced heff-peff).
"What’s most different in the new heart failure guidelines is that we have uploaded HFpEF to the front page," said Dr. Yancy. "We want you to appreciate how important it is. We recognize that there’s no evidence-based intervention that changes its natural history; rather, the focus is on identification and treatment of the comorbidities. It’s important to emphasize that this is a novel way of thinking about heart failure for a very important iteration of that disease."
Among the other highlights of the guidelines is a clarification of the current role for biomarker-guided heart failure therapy. B-type natriuretic peptide (BNP) or N-terminal pro-BNP measurements are deemed useful in making the diagnosis of heart failure as well as in establishing prognosis. Serial measurements can be used to titrate GDMT to optimal doses. But there are as yet no data to show that using the biomarkers to titrate GDMT to higher doses improves mortality.
The 2013 ACC/AHA Guideline for the Management of Heart Failure was developed in collaboration with the American Academy of Family Physicians, the American College of Chest Physicians, the Heart Rhythm Society, and the International Society for Heart and Lung Transplantation (J. Am. Coll. Cardiol. 2013;62:e147-e239).
Dr. Yancy reported having no financial conflicts.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Beta-blockers lose luster for hypertension therapy
SNOWMASS, COLO. – Beta-blockers have lost their decades-long status as first-line therapy for hypertension.
"Generally, I think there is a consensus that beta-blockers are a poor choice for uncomplicated hypertension," Dr. Clive Rosendorff observed at the Annual Cardiovascular Conference at Snowmass.
Abundant evidence indicates that beta-blockers provide less protection against stroke, MI, and overall mortality than other classes of antihypertensive agents. They offer less renal protection than ramipril and achieve less regression of left ventricular hypertrophy than other antihypertensive drugs.
Moreover, as was shown in the Conduit Artery Function Evaluation (CAFE) study, beta-blockers have what has been termed "pseudo-antihypertensive efficacy": that is, they fail to reduce central aortic blood pressure to the same extent they lower systolic blood pressure, which may explain why they are less cardioprotective than other antihypertensive drugs. They also are associated with an increase in insulin resistance, reduced exercise tolerance, weight gain, and a high rate of withdrawal because of side effects, said Dr. Rosendorff, professor of medicine at Mount Sinai School of Medicine, New York.
Dr. Rosdendorff chaired the joint American College of Cardiology/American Heart Association/American Society for Hypertension committee that wrote the soon-to-be-released revised scientific statement on the treatment of hypertension in the prevention and management of ischemic heart disease. He also chaired the 2007 AHA scientific statement on the subject (Circulation 2007;115:2761-88).
One of the most persuasive pieces of evidence of the shortcomings of beta-blockers as first-line agents for uncomplicated hypertension to appear since the release of the 2007 AHA scientific statement was a meta-analysis of six meta-analyses. The six meta-analyses incorporated a total of 26 randomized trials of beta-blockers versus placebo. The conclusion: beta-blockers were no better than placebo in preventing MI or mortality, although they did result in a 16%-22% relative reduction in stroke risk (J. Am. Coll. Cardiol. 2007;50:563-72).
This meta-meta-analysis also included three meta-analyses of comparative trials of beta-blockers versus diuretics and three meta-analyses of beta-blockers compared with other drugs. Beta-blockers turned out to be significantly worse than the other antihypertensive agents in terms of the three endpoints of MI, stroke, and mortality.
A caveat: these clinical trials and meta-analyses were nearly all restricted to atenolol and short-acting metoprolol.
"We don’t have any comparable data for newer beta-blockers. Carvedilol has never been looked at from the point of view of outcomes in hypertension. Bisoprolol likewise, and nabivolol, too. It’s possible that the paradigm might be changed quite considerably when we have data to support the use of these newer beta-blockers in the treatment of hypertension," the cardiologist said.
Dr. Rosendorff noted that he wasn’t at liberty to discuss the recommendations of the forthcoming ACC/AHA/ASH scientific statement in advance of its release. He stressed that his comments on the drawbacks of beta-blockers for uncomplicated hypertension represented his own views and not necessarily the panel’s.
Of note, however, is that the recently published report of the Eighth Joint National Committee (JNC 8) doesn’t list beta-blockers among the four classes of antihypertensive medications recommended for the initial treatment of hypertension (JAMA 2014;311:507-20).
Dr. Rosendorff reported having no financial conflicts of interest.
SNOWMASS, COLO. – Beta-blockers have lost their decades-long status as first-line therapy for hypertension.
"Generally, I think there is a consensus that beta-blockers are a poor choice for uncomplicated hypertension," Dr. Clive Rosendorff observed at the Annual Cardiovascular Conference at Snowmass.
Abundant evidence indicates that beta-blockers provide less protection against stroke, MI, and overall mortality than other classes of antihypertensive agents. They offer less renal protection than ramipril and achieve less regression of left ventricular hypertrophy than other antihypertensive drugs.
Moreover, as was shown in the Conduit Artery Function Evaluation (CAFE) study, beta-blockers have what has been termed "pseudo-antihypertensive efficacy": that is, they fail to reduce central aortic blood pressure to the same extent they lower systolic blood pressure, which may explain why they are less cardioprotective than other antihypertensive drugs. They also are associated with an increase in insulin resistance, reduced exercise tolerance, weight gain, and a high rate of withdrawal because of side effects, said Dr. Rosendorff, professor of medicine at Mount Sinai School of Medicine, New York.
Dr. Rosdendorff chaired the joint American College of Cardiology/American Heart Association/American Society for Hypertension committee that wrote the soon-to-be-released revised scientific statement on the treatment of hypertension in the prevention and management of ischemic heart disease. He also chaired the 2007 AHA scientific statement on the subject (Circulation 2007;115:2761-88).
One of the most persuasive pieces of evidence of the shortcomings of beta-blockers as first-line agents for uncomplicated hypertension to appear since the release of the 2007 AHA scientific statement was a meta-analysis of six meta-analyses. The six meta-analyses incorporated a total of 26 randomized trials of beta-blockers versus placebo. The conclusion: beta-blockers were no better than placebo in preventing MI or mortality, although they did result in a 16%-22% relative reduction in stroke risk (J. Am. Coll. Cardiol. 2007;50:563-72).
This meta-meta-analysis also included three meta-analyses of comparative trials of beta-blockers versus diuretics and three meta-analyses of beta-blockers compared with other drugs. Beta-blockers turned out to be significantly worse than the other antihypertensive agents in terms of the three endpoints of MI, stroke, and mortality.
A caveat: these clinical trials and meta-analyses were nearly all restricted to atenolol and short-acting metoprolol.
"We don’t have any comparable data for newer beta-blockers. Carvedilol has never been looked at from the point of view of outcomes in hypertension. Bisoprolol likewise, and nabivolol, too. It’s possible that the paradigm might be changed quite considerably when we have data to support the use of these newer beta-blockers in the treatment of hypertension," the cardiologist said.
Dr. Rosendorff noted that he wasn’t at liberty to discuss the recommendations of the forthcoming ACC/AHA/ASH scientific statement in advance of its release. He stressed that his comments on the drawbacks of beta-blockers for uncomplicated hypertension represented his own views and not necessarily the panel’s.
Of note, however, is that the recently published report of the Eighth Joint National Committee (JNC 8) doesn’t list beta-blockers among the four classes of antihypertensive medications recommended for the initial treatment of hypertension (JAMA 2014;311:507-20).
Dr. Rosendorff reported having no financial conflicts of interest.
SNOWMASS, COLO. – Beta-blockers have lost their decades-long status as first-line therapy for hypertension.
"Generally, I think there is a consensus that beta-blockers are a poor choice for uncomplicated hypertension," Dr. Clive Rosendorff observed at the Annual Cardiovascular Conference at Snowmass.
Abundant evidence indicates that beta-blockers provide less protection against stroke, MI, and overall mortality than other classes of antihypertensive agents. They offer less renal protection than ramipril and achieve less regression of left ventricular hypertrophy than other antihypertensive drugs.
Moreover, as was shown in the Conduit Artery Function Evaluation (CAFE) study, beta-blockers have what has been termed "pseudo-antihypertensive efficacy": that is, they fail to reduce central aortic blood pressure to the same extent they lower systolic blood pressure, which may explain why they are less cardioprotective than other antihypertensive drugs. They also are associated with an increase in insulin resistance, reduced exercise tolerance, weight gain, and a high rate of withdrawal because of side effects, said Dr. Rosendorff, professor of medicine at Mount Sinai School of Medicine, New York.
Dr. Rosdendorff chaired the joint American College of Cardiology/American Heart Association/American Society for Hypertension committee that wrote the soon-to-be-released revised scientific statement on the treatment of hypertension in the prevention and management of ischemic heart disease. He also chaired the 2007 AHA scientific statement on the subject (Circulation 2007;115:2761-88).
One of the most persuasive pieces of evidence of the shortcomings of beta-blockers as first-line agents for uncomplicated hypertension to appear since the release of the 2007 AHA scientific statement was a meta-analysis of six meta-analyses. The six meta-analyses incorporated a total of 26 randomized trials of beta-blockers versus placebo. The conclusion: beta-blockers were no better than placebo in preventing MI or mortality, although they did result in a 16%-22% relative reduction in stroke risk (J. Am. Coll. Cardiol. 2007;50:563-72).
This meta-meta-analysis also included three meta-analyses of comparative trials of beta-blockers versus diuretics and three meta-analyses of beta-blockers compared with other drugs. Beta-blockers turned out to be significantly worse than the other antihypertensive agents in terms of the three endpoints of MI, stroke, and mortality.
A caveat: these clinical trials and meta-analyses were nearly all restricted to atenolol and short-acting metoprolol.
"We don’t have any comparable data for newer beta-blockers. Carvedilol has never been looked at from the point of view of outcomes in hypertension. Bisoprolol likewise, and nabivolol, too. It’s possible that the paradigm might be changed quite considerably when we have data to support the use of these newer beta-blockers in the treatment of hypertension," the cardiologist said.
Dr. Rosendorff noted that he wasn’t at liberty to discuss the recommendations of the forthcoming ACC/AHA/ASH scientific statement in advance of its release. He stressed that his comments on the drawbacks of beta-blockers for uncomplicated hypertension represented his own views and not necessarily the panel’s.
Of note, however, is that the recently published report of the Eighth Joint National Committee (JNC 8) doesn’t list beta-blockers among the four classes of antihypertensive medications recommended for the initial treatment of hypertension (JAMA 2014;311:507-20).
Dr. Rosendorff reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Latest studies fine-tune ACC/AHA dietary guidelines
SNOWMASS, COLO. – Recent large studies validate and fine-tune the 2013 American Heart Association/American College of Cardiology guidelines on diet and lifestyle management to reduce cardiovascular risk.
The guidelines recommend a dietary pattern that emphasizes fruits and vegetables, whole grains, legumes, fish, poultry, nuts and vegetable oils for fat, and restricted consumption of saturated and trans fats, sugar, sodium, and red meat. It’s a dietary pattern evocative of the Mediterranean or DASH-type diet (J. Am. Coll. Cardiol. 2014 Jan. 28 [doi:10.1016/j.jacc.2013.11.003]).
"There’s nothing particularly controversial here. I support all these recommendations," Dr. Robert A. Vogel commented at the Annual Cardiovascular Conference at Snowmass.
A fair number of important studies bearing on the topic of diet and longevity have appeared since the AHA/ACC guidelines were developed. Dr. Vogel shared highlights of these randomized and cohort studies, some of which were published in journals most physicians don’t read regularly.
• Fruits and veggies: Conventional dietary guidance has emphasized the importance of eating a wide range of fruits and vegetables.
"You’ve been told to eat vegetables and fruits of every different color. Variety is the cornerstone of dietary advice, right? Wrong!" said Dr. Vogel, a cardiologist at the University of Colorado, Denver.
He cited a prospective study of the independent roles of quantity and variety in vegetable and fruit consumption in association with incident coronary heart disease in 71,141 women and 42,135 men participating in the Nurses’ Health Study and the Health Professionals Follow-Up Study. During follow-up there were 2,582 documented cases of CHD in women and 3,607 in men. In a multivariate analysis, subjects in the highest quintile of daily fruit and vegetable consumption had a 17% lower risk of CHD. The absolute quantity of fruit and vegetable intake, but not the variety, was associated with a significantly lower risk of CHD. (Am. J. Clin. Nutr. 2013;98:1514-23).
• Nuts: In a separate analysis of more than 3 million person-years of prospective follow-up data from the Nurses’ Health Study and the Health Professionals Follow-Up Study, increasing consumption of nuts was associated with a stepwise reduction in all-cause mortality. People who consumed nuts less than once a week had a statistically significant 7% reduction in the risk of total mortality, compared with those who didn’t eat nuts. Subjects who ate nuts once per week had an 11% reduction in risk; those who ate nuts 2-4 times per week had a 13% reduction; nut eaters 5 or 6 times per week had a 15% reduction in risk; and subjects who ate nuts 7 or more times per week had a 20% reduction in the risk of total mortality. Also, significant inverse relationships were seen between nut intake and specific common causes of death, including cancer, heart disease, and pulmonary disease.
Investigators reanalyzed the data separately for consumption of tree nuts and peanuts, which are actually legumes. The mortality risk reduction was the same for both (N. Engl. J. Med. 2013;369:2001-11).
"Peanuts are not nuts, but they work like nuts," Dr. Vogel observed.
• Meat: An analysis of 448,568 participants in the EPIC (European Prospective Investigation into Cancer and Nutrition) trial, 26,344 of whom have died, showed what investigators termed "a moderate positive association" between processed meat consumption and mortality, especially deaths from cardiovascular disease and cancer. In a multivariate analysis, daily consumption of red meat at an average of 160 g or more – that’s 5.6 oz. – was independently associated with 14% higher all-cause mortality than in individuals who consumed an average of 10-19.9/day.
The association was more striking for processed meat, such as salami: Subjects who ate an average of 5.6 oz/day had 44% greater all-cause mortality. The investigators estimated that if all study participants limited their processed meat consumption to less than 20 g/day, 3.3% of deaths could be prevented (BMC Med. 2013;11:63 [doi:10.1186/1741-7015-11-63]).
The EPIC findings call to mind an earlier study by investigators at Loma Linda (Calif.) University, who reviewed six prospective cohort studies and concluded that very low meat consumption – less than once weekly – was associated with increased longevity, but that how long subjects had been on such a diet was a key factor. Individuals who had at least a 20-year history of very low meat intake lived an average of 3.6 years longer than those who had adopted the dietary practice more recently (Am. J. Clin. Nutr. 2003;78:526S-532S).
"When you make the changes to adopt a healthier lifestyle substantially matters in terms of longevity. It’s great to change your diet after your first non-ST-elevation MI, but in fact you want to do it before," Dr. Vogel observed.
• Which components of the Mediterranean diet are most beneficial? Greek investigators involved in the EPIC study addressed this question in 23,349 subjects followed for a mean of 8.5 years, during which 1,075 deaths occurred. Greater adherence to the Mediterranean diet was associated with larger reductions in total mortality. By analyzing Mediterranean diet adherence scores, the investigators determined that 16% of the mortality benefit was attributable to high vegetable consumption, 11% to high fruit and nut intake, 10% to legume consumption, 24% was from moderate alcohol consumption, 17% to low intake of meats, and just 11% to fats and oils having a high monounsaturated-to-saturated lipid ratio (BMJ 2009;338:b2337).
"We think that the Mediterranean diet is olive oil, but probably olive oil is good because you put it on a salad; and fruits and vegetables are the best part of a diet," the cardiologist said.
• How to maximize longevity: "If I had one recommendation based upon all the data I’ve reviewed," Dr. Vogel said, "it would be to become a pesco-vegetarian. They in fact are the longest-living Americans. That’s a vegetarian diet with the addition of fish."
Seventh-Day Adventists as a group have the longest life expectancy among all Americans. And analysis of 73,308 Seventh-day Adventists participating in the Adventist Health Study 2 showed that during a mean follow-up of 5.8 years, the adjusted risk of all-cause mortality was 12% lower among all vegetarians than in non-vegetarians, and 19% lower in the subgroup composed of pesco-vegetarians (JAMA Intern. Med. 2013;173:1230-8).
Dr. Vogel serves as a consultant to the Pritikin Longevity Center.
SNOWMASS, COLO. – Recent large studies validate and fine-tune the 2013 American Heart Association/American College of Cardiology guidelines on diet and lifestyle management to reduce cardiovascular risk.
The guidelines recommend a dietary pattern that emphasizes fruits and vegetables, whole grains, legumes, fish, poultry, nuts and vegetable oils for fat, and restricted consumption of saturated and trans fats, sugar, sodium, and red meat. It’s a dietary pattern evocative of the Mediterranean or DASH-type diet (J. Am. Coll. Cardiol. 2014 Jan. 28 [doi:10.1016/j.jacc.2013.11.003]).
"There’s nothing particularly controversial here. I support all these recommendations," Dr. Robert A. Vogel commented at the Annual Cardiovascular Conference at Snowmass.
A fair number of important studies bearing on the topic of diet and longevity have appeared since the AHA/ACC guidelines were developed. Dr. Vogel shared highlights of these randomized and cohort studies, some of which were published in journals most physicians don’t read regularly.
• Fruits and veggies: Conventional dietary guidance has emphasized the importance of eating a wide range of fruits and vegetables.
"You’ve been told to eat vegetables and fruits of every different color. Variety is the cornerstone of dietary advice, right? Wrong!" said Dr. Vogel, a cardiologist at the University of Colorado, Denver.
He cited a prospective study of the independent roles of quantity and variety in vegetable and fruit consumption in association with incident coronary heart disease in 71,141 women and 42,135 men participating in the Nurses’ Health Study and the Health Professionals Follow-Up Study. During follow-up there were 2,582 documented cases of CHD in women and 3,607 in men. In a multivariate analysis, subjects in the highest quintile of daily fruit and vegetable consumption had a 17% lower risk of CHD. The absolute quantity of fruit and vegetable intake, but not the variety, was associated with a significantly lower risk of CHD. (Am. J. Clin. Nutr. 2013;98:1514-23).
• Nuts: In a separate analysis of more than 3 million person-years of prospective follow-up data from the Nurses’ Health Study and the Health Professionals Follow-Up Study, increasing consumption of nuts was associated with a stepwise reduction in all-cause mortality. People who consumed nuts less than once a week had a statistically significant 7% reduction in the risk of total mortality, compared with those who didn’t eat nuts. Subjects who ate nuts once per week had an 11% reduction in risk; those who ate nuts 2-4 times per week had a 13% reduction; nut eaters 5 or 6 times per week had a 15% reduction in risk; and subjects who ate nuts 7 or more times per week had a 20% reduction in the risk of total mortality. Also, significant inverse relationships were seen between nut intake and specific common causes of death, including cancer, heart disease, and pulmonary disease.
Investigators reanalyzed the data separately for consumption of tree nuts and peanuts, which are actually legumes. The mortality risk reduction was the same for both (N. Engl. J. Med. 2013;369:2001-11).
"Peanuts are not nuts, but they work like nuts," Dr. Vogel observed.
• Meat: An analysis of 448,568 participants in the EPIC (European Prospective Investigation into Cancer and Nutrition) trial, 26,344 of whom have died, showed what investigators termed "a moderate positive association" between processed meat consumption and mortality, especially deaths from cardiovascular disease and cancer. In a multivariate analysis, daily consumption of red meat at an average of 160 g or more – that’s 5.6 oz. – was independently associated with 14% higher all-cause mortality than in individuals who consumed an average of 10-19.9/day.
The association was more striking for processed meat, such as salami: Subjects who ate an average of 5.6 oz/day had 44% greater all-cause mortality. The investigators estimated that if all study participants limited their processed meat consumption to less than 20 g/day, 3.3% of deaths could be prevented (BMC Med. 2013;11:63 [doi:10.1186/1741-7015-11-63]).
The EPIC findings call to mind an earlier study by investigators at Loma Linda (Calif.) University, who reviewed six prospective cohort studies and concluded that very low meat consumption – less than once weekly – was associated with increased longevity, but that how long subjects had been on such a diet was a key factor. Individuals who had at least a 20-year history of very low meat intake lived an average of 3.6 years longer than those who had adopted the dietary practice more recently (Am. J. Clin. Nutr. 2003;78:526S-532S).
"When you make the changes to adopt a healthier lifestyle substantially matters in terms of longevity. It’s great to change your diet after your first non-ST-elevation MI, but in fact you want to do it before," Dr. Vogel observed.
• Which components of the Mediterranean diet are most beneficial? Greek investigators involved in the EPIC study addressed this question in 23,349 subjects followed for a mean of 8.5 years, during which 1,075 deaths occurred. Greater adherence to the Mediterranean diet was associated with larger reductions in total mortality. By analyzing Mediterranean diet adherence scores, the investigators determined that 16% of the mortality benefit was attributable to high vegetable consumption, 11% to high fruit and nut intake, 10% to legume consumption, 24% was from moderate alcohol consumption, 17% to low intake of meats, and just 11% to fats and oils having a high monounsaturated-to-saturated lipid ratio (BMJ 2009;338:b2337).
"We think that the Mediterranean diet is olive oil, but probably olive oil is good because you put it on a salad; and fruits and vegetables are the best part of a diet," the cardiologist said.
• How to maximize longevity: "If I had one recommendation based upon all the data I’ve reviewed," Dr. Vogel said, "it would be to become a pesco-vegetarian. They in fact are the longest-living Americans. That’s a vegetarian diet with the addition of fish."
Seventh-Day Adventists as a group have the longest life expectancy among all Americans. And analysis of 73,308 Seventh-day Adventists participating in the Adventist Health Study 2 showed that during a mean follow-up of 5.8 years, the adjusted risk of all-cause mortality was 12% lower among all vegetarians than in non-vegetarians, and 19% lower in the subgroup composed of pesco-vegetarians (JAMA Intern. Med. 2013;173:1230-8).
Dr. Vogel serves as a consultant to the Pritikin Longevity Center.
SNOWMASS, COLO. – Recent large studies validate and fine-tune the 2013 American Heart Association/American College of Cardiology guidelines on diet and lifestyle management to reduce cardiovascular risk.
The guidelines recommend a dietary pattern that emphasizes fruits and vegetables, whole grains, legumes, fish, poultry, nuts and vegetable oils for fat, and restricted consumption of saturated and trans fats, sugar, sodium, and red meat. It’s a dietary pattern evocative of the Mediterranean or DASH-type diet (J. Am. Coll. Cardiol. 2014 Jan. 28 [doi:10.1016/j.jacc.2013.11.003]).
"There’s nothing particularly controversial here. I support all these recommendations," Dr. Robert A. Vogel commented at the Annual Cardiovascular Conference at Snowmass.
A fair number of important studies bearing on the topic of diet and longevity have appeared since the AHA/ACC guidelines were developed. Dr. Vogel shared highlights of these randomized and cohort studies, some of which were published in journals most physicians don’t read regularly.
• Fruits and veggies: Conventional dietary guidance has emphasized the importance of eating a wide range of fruits and vegetables.
"You’ve been told to eat vegetables and fruits of every different color. Variety is the cornerstone of dietary advice, right? Wrong!" said Dr. Vogel, a cardiologist at the University of Colorado, Denver.
He cited a prospective study of the independent roles of quantity and variety in vegetable and fruit consumption in association with incident coronary heart disease in 71,141 women and 42,135 men participating in the Nurses’ Health Study and the Health Professionals Follow-Up Study. During follow-up there were 2,582 documented cases of CHD in women and 3,607 in men. In a multivariate analysis, subjects in the highest quintile of daily fruit and vegetable consumption had a 17% lower risk of CHD. The absolute quantity of fruit and vegetable intake, but not the variety, was associated with a significantly lower risk of CHD. (Am. J. Clin. Nutr. 2013;98:1514-23).
• Nuts: In a separate analysis of more than 3 million person-years of prospective follow-up data from the Nurses’ Health Study and the Health Professionals Follow-Up Study, increasing consumption of nuts was associated with a stepwise reduction in all-cause mortality. People who consumed nuts less than once a week had a statistically significant 7% reduction in the risk of total mortality, compared with those who didn’t eat nuts. Subjects who ate nuts once per week had an 11% reduction in risk; those who ate nuts 2-4 times per week had a 13% reduction; nut eaters 5 or 6 times per week had a 15% reduction in risk; and subjects who ate nuts 7 or more times per week had a 20% reduction in the risk of total mortality. Also, significant inverse relationships were seen between nut intake and specific common causes of death, including cancer, heart disease, and pulmonary disease.
Investigators reanalyzed the data separately for consumption of tree nuts and peanuts, which are actually legumes. The mortality risk reduction was the same for both (N. Engl. J. Med. 2013;369:2001-11).
"Peanuts are not nuts, but they work like nuts," Dr. Vogel observed.
• Meat: An analysis of 448,568 participants in the EPIC (European Prospective Investigation into Cancer and Nutrition) trial, 26,344 of whom have died, showed what investigators termed "a moderate positive association" between processed meat consumption and mortality, especially deaths from cardiovascular disease and cancer. In a multivariate analysis, daily consumption of red meat at an average of 160 g or more – that’s 5.6 oz. – was independently associated with 14% higher all-cause mortality than in individuals who consumed an average of 10-19.9/day.
The association was more striking for processed meat, such as salami: Subjects who ate an average of 5.6 oz/day had 44% greater all-cause mortality. The investigators estimated that if all study participants limited their processed meat consumption to less than 20 g/day, 3.3% of deaths could be prevented (BMC Med. 2013;11:63 [doi:10.1186/1741-7015-11-63]).
The EPIC findings call to mind an earlier study by investigators at Loma Linda (Calif.) University, who reviewed six prospective cohort studies and concluded that very low meat consumption – less than once weekly – was associated with increased longevity, but that how long subjects had been on such a diet was a key factor. Individuals who had at least a 20-year history of very low meat intake lived an average of 3.6 years longer than those who had adopted the dietary practice more recently (Am. J. Clin. Nutr. 2003;78:526S-532S).
"When you make the changes to adopt a healthier lifestyle substantially matters in terms of longevity. It’s great to change your diet after your first non-ST-elevation MI, but in fact you want to do it before," Dr. Vogel observed.
• Which components of the Mediterranean diet are most beneficial? Greek investigators involved in the EPIC study addressed this question in 23,349 subjects followed for a mean of 8.5 years, during which 1,075 deaths occurred. Greater adherence to the Mediterranean diet was associated with larger reductions in total mortality. By analyzing Mediterranean diet adherence scores, the investigators determined that 16% of the mortality benefit was attributable to high vegetable consumption, 11% to high fruit and nut intake, 10% to legume consumption, 24% was from moderate alcohol consumption, 17% to low intake of meats, and just 11% to fats and oils having a high monounsaturated-to-saturated lipid ratio (BMJ 2009;338:b2337).
"We think that the Mediterranean diet is olive oil, but probably olive oil is good because you put it on a salad; and fruits and vegetables are the best part of a diet," the cardiologist said.
• How to maximize longevity: "If I had one recommendation based upon all the data I’ve reviewed," Dr. Vogel said, "it would be to become a pesco-vegetarian. They in fact are the longest-living Americans. That’s a vegetarian diet with the addition of fish."
Seventh-Day Adventists as a group have the longest life expectancy among all Americans. And analysis of 73,308 Seventh-day Adventists participating in the Adventist Health Study 2 showed that during a mean follow-up of 5.8 years, the adjusted risk of all-cause mortality was 12% lower among all vegetarians than in non-vegetarians, and 19% lower in the subgroup composed of pesco-vegetarians (JAMA Intern. Med. 2013;173:1230-8).
Dr. Vogel serves as a consultant to the Pritikin Longevity Center.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS