User login
Repeat BAL Advised With Prolonged Therapy for Ventilator-Associated Pneumonia
HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
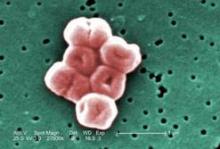
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.
HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.
HOUSTON – Repeat bronchoalveolar lavage should be considered for tailoring the duration of antibiotic therapy and for reassessing resistance profiles in patients with ventilator-associated pneumonia from infection with non–lactose fermenting gram-negative bacilli.
New clinical evidence endorses prolonged antibiotic therapy in these patients. Importantly, the findings also indicate that these patients have persistent primary infections, rather than recurrent infections, as has been previously suggested, Dr. Gina R. Shirah reported at Annual Congress of the Society for Critical Care Medicine.
The distinction between persistent and recurrent infection is important, she emphasized, as the former may signal drug resistance in some patients. For this reason, repeat bronchoalveolar lavage (BAL) should be considered during therapy, both to tailor duration of antibiotics and reassess for changes in resistance profiles.
The American Thoracic Society recommends an 8-day antimicrobial treatment protocol for ventilator-associated pneumonia (VAP) but advises a longer course of therapy in patients with non–lactose fermenting gram-negative rods (NLF-GNR), which include Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia (Am. J. Respir. Crit. Care Med. 2005;171:388-416). The recommendation is based on the findings of a pioneering randomized study by the PneumA Trial Group that showed 8-day treatment to be as effective as 15-day treatment except in a subgroup of patients with NLF-GNR, in whom they observed higher recurrence rates (JAMA 2003;290:2588-98).
Dr. Shirah and her fellow researchers at the Maricopa Integrated Health System in Phoenix, including lead investigator Dr. Tammy Kopelman, conducted a study that indicates 8-day antibiotic regimens were associated with persistent primary infections, not recurrent infections, in patients with gram-negative bacilli.
The researchers retrospectively studied patients at a level I trauma center admitted over a 4½-year time period. They examined data for all ventilator-associated pneumonia patients who were diagnosed via bronchoalveolar lavage – and who underwent subsequent BAL during the antimicrobial treatment course. Based upon initial BAL pathogen, the patients were classified into two groups: those with NLF-GNR and those with all other pathogens, including Enterobacteriaceae, methicillin-resistant Staphylococcus aureus, and community-acquired Haemophilus spp, methicillin-sensitive S. aureus, and Streptococcus spp. They were then further divided based on whether the repeat BAL was conducted within fewer than 8 days of appropriate antibiotic therapy or at day 8 or later, Dr. Shirah said. "Persistent primary infection was defined as a less than 2-log 10 decrease of the initial species on subsequent bronchoalveolar lavage," she explained.
Of the 77 surgical intensive care unit patients who met the study criteria, 99% received appropriate empiric therapy, said Dr. Shirah. The average subsequent BAL performance was on day 7 (range, 3-14 days), with 37 patients undergoing the procedure after 8 days of therapy; of those, 13 patients were in the NLF-GNR group. Within that group, persistent primary infection after more than 8 days of appropriate antimicrobial therapy was reported in nine of the patients (69%) – seven with P. aeruginosa and two with A. baumannii.
By comparison, only two patients in the second group (8%) – both with Enterobacteriaceae – had evidence of persistent primary infection, representing a statistically significant difference, she said. "Importantly, in the [NLF-GNB] group, 56% of the pathogens obtained on repeat BAL remained sensitive to the treatment antibiotics, so nearly half of the patients required alternative antibiotic treatment."
The investigators also sought to determine whether persistent infection could have been predicted. They separated patients into three groups based on treatment status: treated (microbiologic cure on subsequent BAL); persistently infected antimicrobial sensitive; and persistently infected antimicrobial resistant. A comparison of clinical parameters across the groups showed that although there was some variation in white blood cell count, temperature, and ventilator needs "none of the differences were statistically significant," and thus not predictive of short-course treatment success or persistent infection, Dr. Shirah said.
The data strongly support the conclusion that a shortened course of antibiotics in patients with VAP caused by NLF-GNR will frequently lead to a persistent primary infection, said Dr. Shirah, noting that, in the case of NLF-GNR, "changes in antibiotic profiles are common and without reliable clinical indicators." For this reason, she stressed, repeat BAL should be considered during therapy, both to tailor duration of antibiotics and to reassess for changes in resistance profiles.
"Eight days is simply not enough," Dr. Shirah said.
On behalf of her coinvestigators and herself, Dr. Shirah reported no conflicts of interest with respect to this study.
FROM THE ANNUAL CONGRESS OF THE SOCIETY FOR CRITICAL CARE MEDICINE
Major Finding: Repeat bronchoalveolar lavage (BAL) of 37 patients after 8 days of appropriate antimicrobial therapy indicated that 69% patients with non–lactose fermenting gram-negative rods had persistent primary infection, compared with 8% patients with all other pathogens.
Data Source: Results came from a retrospective study of 77 patients with BAL-diagnosed ventilator-associated pneumonia who underwent repeat BAL while on antibiotic therapy at a level 1 trauma center.
Disclosures: The investigators reported having no relevant financial disclosures.
RAP Scores Guide Ultrasonography for VTE in Trauma Patients
HOUSTON – Nearly 30% of trauma patients who were identified upon admission as being high risk for venous thromboembolism using a validated risk assessment tool went on to develop the thrombotic condition during their ICU stay, a study has shown.
Importantly, the deep vein thromboses in most of these patients were asymptomatic and might have gone undetected with potentially life-threatening consequences but for periodic ultrasound screening, Dr. Chad Thorson reported at the annual congress of the Society of Critical Care Medicine.
"Routine venous thromboembolism screening in the trauma population has been widely debated, and there currently is no protocol for it," according to Dr. Thorson of the Ryder Trauma Center at the University of Miami. Although the principal diagnostic screening tool – venous duplex ultrasound (VDU) – is not considered cost effective for screening all trauma patients, the investigators sought to determine whether prescreening trauma patients using the risk assessment profile (RAP) would yield a cohort of high- risk patients in whom increased vigilance and VDU screening are warranted (J. Trauma 1997;42:100-3).
Toward this end, all patients admitted to the Ryder Center’s level 1 trauma intensive care unit from November 2009 through January 2012 were prospectively screened with RAP, which stratifies an individual’s venous thromboembolism (VTE) risk based on underlying conditions, iatrogenic factors, injury-related factors, and age, within 24 hours of admission.
"Patients with [RAP] scores of 10 or higher received bilateral lower-extremity venous duplex ultrasounds at the time of admission and then weekly throughout their ICU stay," Dr. Thorson said, noting that logistic regression was performed on risk factors to identify independent predictors of VTE development. Among the risk factors considered were RAP score, RAP score higher than 20, femoral central venous catheterization for more than 24 hours, operative intervention duration longer than 2 hours, lower-extremity fracture, pelvic fracture, and spinal cord injury with paraplegia.
Of 534 trauma ICU admissions during the study period, 106 patients (mean age, 47 years) were identified as high risk based on their RAP score. Blunt trauma was the primary mechanism of injury in 79% of the population, and the mean injury severity score of the predominantly male (74%) high-risk population was 30, said Dr. Thorson.
Routine VDU screening identified 30 VTEs, including 20 that were asymptomatic and 10 that were symptomatic, despite the patients having received thromboprophylaxis (heparin 5,000 U every 8 hours or dalteparin 5,000 U daily), Dr. Thorson reported. Four of the symptomatic events were pulmonary emboli, and of the asymptomatic VTEs, six were identified on admission, seven were identified within the first week of admission, and four were identified within 2 weeks of admission, he said.
A comparison of those who did and did not develop VTEs showed significant differences in the number of risk factors, overall RAP score, and RAP score greater than 20, Dr. Thorson reported. Specifically, those in the non-VTE group averaged five risk factors compared with seven in the VTE group, and the respective median RAP scores were 14 and 19, he said. In addition, 6 patients in the non-VTE and 11 in the VTE group had RAP scores higher than 20. In the stepwise logistic regression analysis, RAP score and a combination of pelvic fracture and prolonged operative intervention were independent predictors of VTE development, he said.
Prescreening trauma patients with RAP is useful for identifying patients at increased risk of VTE who may be candidates for increased surveillance, according to Dr. Thorson. "There is plenty of debate with regard to the utility and cost effectiveness of routine screening, as well as the benefit of identifying asymptomatic deep vein thromboses," Dr. Thorson said in an interview.
"Ideally, we hope to find a decrease in the rate of pulmonary embolism as a result of screening, as this consequence can be devastating."
An important implication of the screening protocol, however, is identifying that DVT/VTE should not be included on the Centers for Medicare and Medicaid Services’ list of preventable complications (defined as errors in medical care that are clearly identifiable and preventable, and thus may no longer be eligible for reimbursement).
"A decision to no longer pay for [VTE] treatment could have devastating effects on many urban trauma centers," Dr. Thorson stressed.
The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
Trauma patients are at high risk for VTE, and in the absence of bleeding contraindications, all should be receiving pharmacologic prophylaxis with LDUH/LMWH. Therefore, a risk assessment program for VTE doesn't make much sense: Everyone "rules in" for VTE prophylaxis with medication unless a contraindication exists, according to Dr. Franklin A. Michota.
This observational study used a risk assessment program to identify patients for whom surveillance venous duplex ultrasound might be indicated on top of pharmacologic prophylaxis. Currently, VDU surveillance is not recommended in trauma patients, according to the recently published ninth American College of Chest Physicians' guidelines on antithrombotic therapy and the prevention of thrombosis (Chest 2012;141[suppl.]:e227S-77S). In fact, the ACCP specifically recommends that surveillance not be performed (grade 2C evidence). The rationale is well outlined in the guidelines. It is not clear that using VDU to detect and treat asymptomatic DVT reduces the risk of pulmonary embolism or fatal pulmonary embolism, and some studies have demonstrated that pulmonary embolism can occur even when VDU is negative.
As reported in the ACCP chapter on the prevention of VTE in surgery patients, a large retrospective study from a single center found that over a 6-year period ending in 2000, the frequency of surveillance VDU decreased from 32% to 3.4%, yet there was no increase in the incidence of pulmonary embolism. Also it is well known that surveillance VDU can lead to false-positive findings (asymptomatic distal clot that does not pose a risk for symptoms or embolization), and the risk of treating the false positives with full anticoagulation in the trauma surgery population may increase adverse outcomes.
This new study identified 30 VTEs in 106 high-risk trauma patients with surveillance VDU. However, the investigators reported that 10 of the events were symptomatic, so the VDU was not a screening tool; it was a diagnostic test for signs and symptoms, and therefore, those 10 symptomatic events need to be removed. That leaves you with 20 VTEs in 106 high-risk trauma patients (18.8%). So the real question is, Where were these clots located? If they were distal asymptomatic events, then they may all be false positives. If they were all proximal DVTs, then perhaps this study deserves more credit.
But we should also look at the intensity of VTE prophylaxis provided in this study cohort. The ACCP also recommends mechanical compression on top of pharmacologic prophylaxis in high-risk trauma patients. Was that done here? Perhaps the 20 VTEs were due to inadequate prophylaxis.
Dr. Michota is the director of academic affairs in the department of hospital medicine at the Cleveland Clinic. He reported having no relevant financial disclosures.
Trauma patients are at high risk for VTE, and in the absence of bleeding contraindications, all should be receiving pharmacologic prophylaxis with LDUH/LMWH. Therefore, a risk assessment program for VTE doesn't make much sense: Everyone "rules in" for VTE prophylaxis with medication unless a contraindication exists, according to Dr. Franklin A. Michota.
This observational study used a risk assessment program to identify patients for whom surveillance venous duplex ultrasound might be indicated on top of pharmacologic prophylaxis. Currently, VDU surveillance is not recommended in trauma patients, according to the recently published ninth American College of Chest Physicians' guidelines on antithrombotic therapy and the prevention of thrombosis (Chest 2012;141[suppl.]:e227S-77S). In fact, the ACCP specifically recommends that surveillance not be performed (grade 2C evidence). The rationale is well outlined in the guidelines. It is not clear that using VDU to detect and treat asymptomatic DVT reduces the risk of pulmonary embolism or fatal pulmonary embolism, and some studies have demonstrated that pulmonary embolism can occur even when VDU is negative.
As reported in the ACCP chapter on the prevention of VTE in surgery patients, a large retrospective study from a single center found that over a 6-year period ending in 2000, the frequency of surveillance VDU decreased from 32% to 3.4%, yet there was no increase in the incidence of pulmonary embolism. Also it is well known that surveillance VDU can lead to false-positive findings (asymptomatic distal clot that does not pose a risk for symptoms or embolization), and the risk of treating the false positives with full anticoagulation in the trauma surgery population may increase adverse outcomes.
This new study identified 30 VTEs in 106 high-risk trauma patients with surveillance VDU. However, the investigators reported that 10 of the events were symptomatic, so the VDU was not a screening tool; it was a diagnostic test for signs and symptoms, and therefore, those 10 symptomatic events need to be removed. That leaves you with 20 VTEs in 106 high-risk trauma patients (18.8%). So the real question is, Where were these clots located? If they were distal asymptomatic events, then they may all be false positives. If they were all proximal DVTs, then perhaps this study deserves more credit.
But we should also look at the intensity of VTE prophylaxis provided in this study cohort. The ACCP also recommends mechanical compression on top of pharmacologic prophylaxis in high-risk trauma patients. Was that done here? Perhaps the 20 VTEs were due to inadequate prophylaxis.
Dr. Michota is the director of academic affairs in the department of hospital medicine at the Cleveland Clinic. He reported having no relevant financial disclosures.
Trauma patients are at high risk for VTE, and in the absence of bleeding contraindications, all should be receiving pharmacologic prophylaxis with LDUH/LMWH. Therefore, a risk assessment program for VTE doesn't make much sense: Everyone "rules in" for VTE prophylaxis with medication unless a contraindication exists, according to Dr. Franklin A. Michota.
This observational study used a risk assessment program to identify patients for whom surveillance venous duplex ultrasound might be indicated on top of pharmacologic prophylaxis. Currently, VDU surveillance is not recommended in trauma patients, according to the recently published ninth American College of Chest Physicians' guidelines on antithrombotic therapy and the prevention of thrombosis (Chest 2012;141[suppl.]:e227S-77S). In fact, the ACCP specifically recommends that surveillance not be performed (grade 2C evidence). The rationale is well outlined in the guidelines. It is not clear that using VDU to detect and treat asymptomatic DVT reduces the risk of pulmonary embolism or fatal pulmonary embolism, and some studies have demonstrated that pulmonary embolism can occur even when VDU is negative.
As reported in the ACCP chapter on the prevention of VTE in surgery patients, a large retrospective study from a single center found that over a 6-year period ending in 2000, the frequency of surveillance VDU decreased from 32% to 3.4%, yet there was no increase in the incidence of pulmonary embolism. Also it is well known that surveillance VDU can lead to false-positive findings (asymptomatic distal clot that does not pose a risk for symptoms or embolization), and the risk of treating the false positives with full anticoagulation in the trauma surgery population may increase adverse outcomes.
This new study identified 30 VTEs in 106 high-risk trauma patients with surveillance VDU. However, the investigators reported that 10 of the events were symptomatic, so the VDU was not a screening tool; it was a diagnostic test for signs and symptoms, and therefore, those 10 symptomatic events need to be removed. That leaves you with 20 VTEs in 106 high-risk trauma patients (18.8%). So the real question is, Where were these clots located? If they were distal asymptomatic events, then they may all be false positives. If they were all proximal DVTs, then perhaps this study deserves more credit.
But we should also look at the intensity of VTE prophylaxis provided in this study cohort. The ACCP also recommends mechanical compression on top of pharmacologic prophylaxis in high-risk trauma patients. Was that done here? Perhaps the 20 VTEs were due to inadequate prophylaxis.
Dr. Michota is the director of academic affairs in the department of hospital medicine at the Cleveland Clinic. He reported having no relevant financial disclosures.
HOUSTON – Nearly 30% of trauma patients who were identified upon admission as being high risk for venous thromboembolism using a validated risk assessment tool went on to develop the thrombotic condition during their ICU stay, a study has shown.
Importantly, the deep vein thromboses in most of these patients were asymptomatic and might have gone undetected with potentially life-threatening consequences but for periodic ultrasound screening, Dr. Chad Thorson reported at the annual congress of the Society of Critical Care Medicine.
"Routine venous thromboembolism screening in the trauma population has been widely debated, and there currently is no protocol for it," according to Dr. Thorson of the Ryder Trauma Center at the University of Miami. Although the principal diagnostic screening tool – venous duplex ultrasound (VDU) – is not considered cost effective for screening all trauma patients, the investigators sought to determine whether prescreening trauma patients using the risk assessment profile (RAP) would yield a cohort of high- risk patients in whom increased vigilance and VDU screening are warranted (J. Trauma 1997;42:100-3).
Toward this end, all patients admitted to the Ryder Center’s level 1 trauma intensive care unit from November 2009 through January 2012 were prospectively screened with RAP, which stratifies an individual’s venous thromboembolism (VTE) risk based on underlying conditions, iatrogenic factors, injury-related factors, and age, within 24 hours of admission.
"Patients with [RAP] scores of 10 or higher received bilateral lower-extremity venous duplex ultrasounds at the time of admission and then weekly throughout their ICU stay," Dr. Thorson said, noting that logistic regression was performed on risk factors to identify independent predictors of VTE development. Among the risk factors considered were RAP score, RAP score higher than 20, femoral central venous catheterization for more than 24 hours, operative intervention duration longer than 2 hours, lower-extremity fracture, pelvic fracture, and spinal cord injury with paraplegia.
Of 534 trauma ICU admissions during the study period, 106 patients (mean age, 47 years) were identified as high risk based on their RAP score. Blunt trauma was the primary mechanism of injury in 79% of the population, and the mean injury severity score of the predominantly male (74%) high-risk population was 30, said Dr. Thorson.
Routine VDU screening identified 30 VTEs, including 20 that were asymptomatic and 10 that were symptomatic, despite the patients having received thromboprophylaxis (heparin 5,000 U every 8 hours or dalteparin 5,000 U daily), Dr. Thorson reported. Four of the symptomatic events were pulmonary emboli, and of the asymptomatic VTEs, six were identified on admission, seven were identified within the first week of admission, and four were identified within 2 weeks of admission, he said.
A comparison of those who did and did not develop VTEs showed significant differences in the number of risk factors, overall RAP score, and RAP score greater than 20, Dr. Thorson reported. Specifically, those in the non-VTE group averaged five risk factors compared with seven in the VTE group, and the respective median RAP scores were 14 and 19, he said. In addition, 6 patients in the non-VTE and 11 in the VTE group had RAP scores higher than 20. In the stepwise logistic regression analysis, RAP score and a combination of pelvic fracture and prolonged operative intervention were independent predictors of VTE development, he said.
Prescreening trauma patients with RAP is useful for identifying patients at increased risk of VTE who may be candidates for increased surveillance, according to Dr. Thorson. "There is plenty of debate with regard to the utility and cost effectiveness of routine screening, as well as the benefit of identifying asymptomatic deep vein thromboses," Dr. Thorson said in an interview.
"Ideally, we hope to find a decrease in the rate of pulmonary embolism as a result of screening, as this consequence can be devastating."
An important implication of the screening protocol, however, is identifying that DVT/VTE should not be included on the Centers for Medicare and Medicaid Services’ list of preventable complications (defined as errors in medical care that are clearly identifiable and preventable, and thus may no longer be eligible for reimbursement).
"A decision to no longer pay for [VTE] treatment could have devastating effects on many urban trauma centers," Dr. Thorson stressed.
The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
HOUSTON – Nearly 30% of trauma patients who were identified upon admission as being high risk for venous thromboembolism using a validated risk assessment tool went on to develop the thrombotic condition during their ICU stay, a study has shown.
Importantly, the deep vein thromboses in most of these patients were asymptomatic and might have gone undetected with potentially life-threatening consequences but for periodic ultrasound screening, Dr. Chad Thorson reported at the annual congress of the Society of Critical Care Medicine.
"Routine venous thromboembolism screening in the trauma population has been widely debated, and there currently is no protocol for it," according to Dr. Thorson of the Ryder Trauma Center at the University of Miami. Although the principal diagnostic screening tool – venous duplex ultrasound (VDU) – is not considered cost effective for screening all trauma patients, the investigators sought to determine whether prescreening trauma patients using the risk assessment profile (RAP) would yield a cohort of high- risk patients in whom increased vigilance and VDU screening are warranted (J. Trauma 1997;42:100-3).
Toward this end, all patients admitted to the Ryder Center’s level 1 trauma intensive care unit from November 2009 through January 2012 were prospectively screened with RAP, which stratifies an individual’s venous thromboembolism (VTE) risk based on underlying conditions, iatrogenic factors, injury-related factors, and age, within 24 hours of admission.
"Patients with [RAP] scores of 10 or higher received bilateral lower-extremity venous duplex ultrasounds at the time of admission and then weekly throughout their ICU stay," Dr. Thorson said, noting that logistic regression was performed on risk factors to identify independent predictors of VTE development. Among the risk factors considered were RAP score, RAP score higher than 20, femoral central venous catheterization for more than 24 hours, operative intervention duration longer than 2 hours, lower-extremity fracture, pelvic fracture, and spinal cord injury with paraplegia.
Of 534 trauma ICU admissions during the study period, 106 patients (mean age, 47 years) were identified as high risk based on their RAP score. Blunt trauma was the primary mechanism of injury in 79% of the population, and the mean injury severity score of the predominantly male (74%) high-risk population was 30, said Dr. Thorson.
Routine VDU screening identified 30 VTEs, including 20 that were asymptomatic and 10 that were symptomatic, despite the patients having received thromboprophylaxis (heparin 5,000 U every 8 hours or dalteparin 5,000 U daily), Dr. Thorson reported. Four of the symptomatic events were pulmonary emboli, and of the asymptomatic VTEs, six were identified on admission, seven were identified within the first week of admission, and four were identified within 2 weeks of admission, he said.
A comparison of those who did and did not develop VTEs showed significant differences in the number of risk factors, overall RAP score, and RAP score greater than 20, Dr. Thorson reported. Specifically, those in the non-VTE group averaged five risk factors compared with seven in the VTE group, and the respective median RAP scores were 14 and 19, he said. In addition, 6 patients in the non-VTE and 11 in the VTE group had RAP scores higher than 20. In the stepwise logistic regression analysis, RAP score and a combination of pelvic fracture and prolonged operative intervention were independent predictors of VTE development, he said.
Prescreening trauma patients with RAP is useful for identifying patients at increased risk of VTE who may be candidates for increased surveillance, according to Dr. Thorson. "There is plenty of debate with regard to the utility and cost effectiveness of routine screening, as well as the benefit of identifying asymptomatic deep vein thromboses," Dr. Thorson said in an interview.
"Ideally, we hope to find a decrease in the rate of pulmonary embolism as a result of screening, as this consequence can be devastating."
An important implication of the screening protocol, however, is identifying that DVT/VTE should not be included on the Centers for Medicare and Medicaid Services’ list of preventable complications (defined as errors in medical care that are clearly identifiable and preventable, and thus may no longer be eligible for reimbursement).
"A decision to no longer pay for [VTE] treatment could have devastating effects on many urban trauma centers," Dr. Thorson stressed.
The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
FROM THE ANNUAL CONGRESS OF THE SOCIETY OF CRITICAL CARE MEDICINE
Major Finding: Of 106 trauma patients identified through a prescreening protocol as being high risk for venous thromboembolism, 30 developed the condition during their ICU stay despite their receiving standard thromboprophylaxis.
Data Source: A prospective study in which 106 patients deemed to be at high risk of venous thromboembolism underwent venous duplex ultrasound at the time of admission and then weekly throughout their ICU stay.
Disclosures: The prescreening study was supported by grants from the Office of Naval Research and the U.S. Army Medical Research and Materiel Command. Dr. Thorson reported that he had no relevant financial disclosures.
ARDS Outcome Linked to Oxygenation at 48 Hours
HOUSTON – Failure to achieve threshold respiratory parameters within the first 48 hours after implementation of high-frequency oscillatory ventilation was linked to higher mortality in patients with severe acute respiratory distress syndrome.
This finding from a retrospective study suggests that the absence of sufficient early improvements in oxygenation in patients with the fulminant lung condition may justify a switch to an alternate ventilation strategy, according to Dr. Samantha Tarras of the University of Michigan Health System in Ann Arbor.
Although high-frequency oscillatory ventilation (HFOV) is indicated as a rescue therapy for patients with severe acute respiratory distress syndrome (ARDS), specific threshold parameters predictive of outcome have not been described, contributing to uncertainty about its optimal application, she said at the annual congress of the Society of Critical Care Medicine.
In a retrospective investigation, Dr. Tarras and her colleagues evaluated the link between threshold oxygenation values and mortality in patients placed on HFOV in the University of Michigan extracorporeal membrane oxygenation (ECMO) referral surgical ICU during 2005-2011. Patients were excluded from analysis if their baseline PaO2/FiO2 (P/F) ratio was 100 or more; if they had ECMO support; or if transition to conventional ventilation, withdrawal of care, or death occurred within the first 48 hours.
Of 112 patients placed on HFOV as part of a standardized ARDS treatment algorithm during the period of study, 58 met entry criteria, according to Dr. Tarras. "Most of the patients were male, young, and critically ill. The median number of days on mechanical ventilation prior to HFOV was 3, and the largest risk factors for ARDS were pneumonia followed by sepsis," she said. The mean P/F ratio at baseline of the patients included in the analysis was 58.4, the mean oxygenation index at baseline was 51.5, and in-hospital mortality was 41.3%, she said.
In univariate analyses, the mortality of patients who failed to reach a threshold P/F ratio of at least 100 within 48 hours was 75%, three times higher than the 24.3% observed in patients who achieved the threshold ratio, Dr. Tarras reported. The sensitivity and specificity of this threshold for predicting survival were 82.4% and 62.5%, respectively, and the positive and negative predictive values were 75.7% and 71.4%, respectively. "Similarly, a significant mortality rate was identified at a threshold oxygenation index of 25 at 48 hours," she said.
Failure to reach the threshold P/F ratio of 100 remained significantly associated with mortality in a multivariate logistic regression model that incorporated patient age, APACHE (Acute Physiology and Chronic Health Evaluation) score, and number of days of mechanical ventilation prior to initiation of HFOV, said Dr. Tarras. "The area under the receiver operator characteristic curve for model performance was 0.774," she noted.
The findings are limited by the lack of information on patients’ cause of death, which could have an effect, Dr. Tarras acknowledged. Even so, "the results tell us that for patients whose oxygenation is not improving after 48 hours of HFOV, clinicians should start thinking about other rescue strategies as well as referral to an ECMO center." Additionally, she said, "this group of patients that is at greater risk of death despite 48 hours [of HFOV] should be targeted in future intervention trials."
Dr. Tarras disclosed having no relevant conflicts of interest.
HOUSTON – Failure to achieve threshold respiratory parameters within the first 48 hours after implementation of high-frequency oscillatory ventilation was linked to higher mortality in patients with severe acute respiratory distress syndrome.
This finding from a retrospective study suggests that the absence of sufficient early improvements in oxygenation in patients with the fulminant lung condition may justify a switch to an alternate ventilation strategy, according to Dr. Samantha Tarras of the University of Michigan Health System in Ann Arbor.
Although high-frequency oscillatory ventilation (HFOV) is indicated as a rescue therapy for patients with severe acute respiratory distress syndrome (ARDS), specific threshold parameters predictive of outcome have not been described, contributing to uncertainty about its optimal application, she said at the annual congress of the Society of Critical Care Medicine.
In a retrospective investigation, Dr. Tarras and her colleagues evaluated the link between threshold oxygenation values and mortality in patients placed on HFOV in the University of Michigan extracorporeal membrane oxygenation (ECMO) referral surgical ICU during 2005-2011. Patients were excluded from analysis if their baseline PaO2/FiO2 (P/F) ratio was 100 or more; if they had ECMO support; or if transition to conventional ventilation, withdrawal of care, or death occurred within the first 48 hours.
Of 112 patients placed on HFOV as part of a standardized ARDS treatment algorithm during the period of study, 58 met entry criteria, according to Dr. Tarras. "Most of the patients were male, young, and critically ill. The median number of days on mechanical ventilation prior to HFOV was 3, and the largest risk factors for ARDS were pneumonia followed by sepsis," she said. The mean P/F ratio at baseline of the patients included in the analysis was 58.4, the mean oxygenation index at baseline was 51.5, and in-hospital mortality was 41.3%, she said.
In univariate analyses, the mortality of patients who failed to reach a threshold P/F ratio of at least 100 within 48 hours was 75%, three times higher than the 24.3% observed in patients who achieved the threshold ratio, Dr. Tarras reported. The sensitivity and specificity of this threshold for predicting survival were 82.4% and 62.5%, respectively, and the positive and negative predictive values were 75.7% and 71.4%, respectively. "Similarly, a significant mortality rate was identified at a threshold oxygenation index of 25 at 48 hours," she said.
Failure to reach the threshold P/F ratio of 100 remained significantly associated with mortality in a multivariate logistic regression model that incorporated patient age, APACHE (Acute Physiology and Chronic Health Evaluation) score, and number of days of mechanical ventilation prior to initiation of HFOV, said Dr. Tarras. "The area under the receiver operator characteristic curve for model performance was 0.774," she noted.
The findings are limited by the lack of information on patients’ cause of death, which could have an effect, Dr. Tarras acknowledged. Even so, "the results tell us that for patients whose oxygenation is not improving after 48 hours of HFOV, clinicians should start thinking about other rescue strategies as well as referral to an ECMO center." Additionally, she said, "this group of patients that is at greater risk of death despite 48 hours [of HFOV] should be targeted in future intervention trials."
Dr. Tarras disclosed having no relevant conflicts of interest.
HOUSTON – Failure to achieve threshold respiratory parameters within the first 48 hours after implementation of high-frequency oscillatory ventilation was linked to higher mortality in patients with severe acute respiratory distress syndrome.
This finding from a retrospective study suggests that the absence of sufficient early improvements in oxygenation in patients with the fulminant lung condition may justify a switch to an alternate ventilation strategy, according to Dr. Samantha Tarras of the University of Michigan Health System in Ann Arbor.
Although high-frequency oscillatory ventilation (HFOV) is indicated as a rescue therapy for patients with severe acute respiratory distress syndrome (ARDS), specific threshold parameters predictive of outcome have not been described, contributing to uncertainty about its optimal application, she said at the annual congress of the Society of Critical Care Medicine.
In a retrospective investigation, Dr. Tarras and her colleagues evaluated the link between threshold oxygenation values and mortality in patients placed on HFOV in the University of Michigan extracorporeal membrane oxygenation (ECMO) referral surgical ICU during 2005-2011. Patients were excluded from analysis if their baseline PaO2/FiO2 (P/F) ratio was 100 or more; if they had ECMO support; or if transition to conventional ventilation, withdrawal of care, or death occurred within the first 48 hours.
Of 112 patients placed on HFOV as part of a standardized ARDS treatment algorithm during the period of study, 58 met entry criteria, according to Dr. Tarras. "Most of the patients were male, young, and critically ill. The median number of days on mechanical ventilation prior to HFOV was 3, and the largest risk factors for ARDS were pneumonia followed by sepsis," she said. The mean P/F ratio at baseline of the patients included in the analysis was 58.4, the mean oxygenation index at baseline was 51.5, and in-hospital mortality was 41.3%, she said.
In univariate analyses, the mortality of patients who failed to reach a threshold P/F ratio of at least 100 within 48 hours was 75%, three times higher than the 24.3% observed in patients who achieved the threshold ratio, Dr. Tarras reported. The sensitivity and specificity of this threshold for predicting survival were 82.4% and 62.5%, respectively, and the positive and negative predictive values were 75.7% and 71.4%, respectively. "Similarly, a significant mortality rate was identified at a threshold oxygenation index of 25 at 48 hours," she said.
Failure to reach the threshold P/F ratio of 100 remained significantly associated with mortality in a multivariate logistic regression model that incorporated patient age, APACHE (Acute Physiology and Chronic Health Evaluation) score, and number of days of mechanical ventilation prior to initiation of HFOV, said Dr. Tarras. "The area under the receiver operator characteristic curve for model performance was 0.774," she noted.
The findings are limited by the lack of information on patients’ cause of death, which could have an effect, Dr. Tarras acknowledged. Even so, "the results tell us that for patients whose oxygenation is not improving after 48 hours of HFOV, clinicians should start thinking about other rescue strategies as well as referral to an ECMO center." Additionally, she said, "this group of patients that is at greater risk of death despite 48 hours [of HFOV] should be targeted in future intervention trials."
Dr. Tarras disclosed having no relevant conflicts of interest.
FROM THE ANNUAL CONGRESS OF THE SOCIETY OF CRITICAL CARE MEDICINE
Major Finding: The mortality of patients with ARDS who failed to reach a threshold P/F ratio of at least 100 within 48 hours of initiation of high-frequency oscillatory ventilation was 75%, compared with a mortality of 24.3% among similar patients who achieved the ratio.
Data Source: A retrospective study comparing mortality in 58 surgical ICU patients with ARDS who received at least 48 hours of high-frequency oscillatory ventilation.
Disclosures: Dr. Tarras disclosed having no relevant conflicts of interest.
Prehospitalization Steroids Don't Reduce Risk of Acute Lung Injury
HOUSTON – Prehospital use of systemic corticosteroids does not prevent the development of acute lung injury in at-risk patients, according to data reported at the annual congress of the Society of Critical Care Medicine.
In the first study to specifically evaluate the prophylactic value of prehospital systemic corticosteroids in patients with at least one risk factor for acute lung injury (ALI), Dr. Lioudmila Karnatovskaia of the Mayo Clinic in Jacksonville, Fla., and colleagues found a statistically similar incidence of ALI among at-risk patients who were and were not taking systemic corticosteroids at the time of hospitalization.
The investigators also determined that prehospital use of systemic corticosteroids did not affect the need for mechanical ventilation or overall mortality – a finding that appears to contradict previous studies that have linked preventive steroids in at-risk patients with increased rates of ALI and acute respiratory distress syndrome, Dr. Karnatovskaia said.
The study was a planned exploratory subgroup analysis of the Lung Injury Prediction Score cohort of the U.S. Critical Illness and Injury Trials Group, which prospectively enrolled 5,584 patients who were admitted to 22 acute care hospitals and who had predisposing conditions for ALI, including sepsis, shock, pancreatitis, pneumonia, aspiration, high-risk trauma, and high-risk surgery. The primary outcome was the development of ALI, and secondary outcomes were need for invasive ventilation and ICU and hospital mortality, Dr. Karnatovskaia said, noting that the data were analyzed using univariate, logistic regression, and propensity score–based analyses.
For the propensity analysis, "the propensity score balanced all of the covariates. Of the 458 patients on systemic corticosteroids, 443 were matched up to 1:4 to those not on systemic corticosteroids, for a total of 1,332 matched patients," she said. "We calculated adjusted risk for acute lung injury, invasive ventilation, and in-hospital mortality from the propensity score–matched sample using a conditional logistic regression model."
Of the 5,584 patients, 458 were on systemic corticosteroids at the time of hospitalization and 5,126 were not. Among the systemic corticosteroid group, 34 (7.4%) developed ALI, compared with 343 (6.7%) of those not taking them, Dr. Karnatovskaia reported. In the systemic corticosteroid group, 104 patients (23%) required mechanical ventilation and 35 patients (8%) died, compared with 1,752 (34%) and 172 (3%) of those not taking systemic corticosteroids, she said.
On univariate analysis, systemic corticosteroid patients were more likely to be older, to be white, and to have diabetes, chronic obstructive pulmonary disease, malignancy, or previous chest radiation, Dr. Karnatovskaia said, noting that they were also more likely to have a lower body mass index and to be on a statin drug, inhaled steroid, inhaled beta-agonist, proton pump inhibitor, ACE inhibitor, angiotensin receptor blocker, or insulin and were less like likely to abuse alcohol or smoke tobacco.
After adjustment for significant covariates, systemic corticosteroid use was not independently associated with the development of ALI or the need for invasive ventilation, but did appear to be an independent predictor of ICU and hospital mortality, Dr. Karnatovskaia said. The latter association fell away, however, in the propensity score–based analysis. "Following propensity score–based analysis with matching, the association of prehospital systemic corticosteroids with mortality no longer remained significant," she said.
The findings are limited by the lack of data on the indication for systemic corticosteroid therapy, its duration, "and even whether it was continued throughout the hospital stay," as well as the fact that patients on prehospital systemic corticosteroids appeared to have worse functional status, which might have influenced their outcomes, according to Dr. Karnatovskaia. Although using the propensity score with matching addressed this as well as other hidden biases, "the potential for unmeasured effects remains," she said.
The study’s strengths include the large number of patients at risk for ALI enrolled from different centers and regions in the United States, as well as two hospitals in Turkey, and the use of comprehensive propensity score–based analysis with matching in addition to traditional logistic regression, Dr. Karnatovskaia said.
Ideally, the finding that prehospital use of systemic corticosteroids does not mitigate the development of ALI would be validated in a randomized controlled trial to best address any causal relationship, "but such a study would not be practical," Dr. Karnatovskaia said.
Dr. Karnatovskaia reported having no relevant financial disclosures.
HOUSTON – Prehospital use of systemic corticosteroids does not prevent the development of acute lung injury in at-risk patients, according to data reported at the annual congress of the Society of Critical Care Medicine.
In the first study to specifically evaluate the prophylactic value of prehospital systemic corticosteroids in patients with at least one risk factor for acute lung injury (ALI), Dr. Lioudmila Karnatovskaia of the Mayo Clinic in Jacksonville, Fla., and colleagues found a statistically similar incidence of ALI among at-risk patients who were and were not taking systemic corticosteroids at the time of hospitalization.
The investigators also determined that prehospital use of systemic corticosteroids did not affect the need for mechanical ventilation or overall mortality – a finding that appears to contradict previous studies that have linked preventive steroids in at-risk patients with increased rates of ALI and acute respiratory distress syndrome, Dr. Karnatovskaia said.
The study was a planned exploratory subgroup analysis of the Lung Injury Prediction Score cohort of the U.S. Critical Illness and Injury Trials Group, which prospectively enrolled 5,584 patients who were admitted to 22 acute care hospitals and who had predisposing conditions for ALI, including sepsis, shock, pancreatitis, pneumonia, aspiration, high-risk trauma, and high-risk surgery. The primary outcome was the development of ALI, and secondary outcomes were need for invasive ventilation and ICU and hospital mortality, Dr. Karnatovskaia said, noting that the data were analyzed using univariate, logistic regression, and propensity score–based analyses.
For the propensity analysis, "the propensity score balanced all of the covariates. Of the 458 patients on systemic corticosteroids, 443 were matched up to 1:4 to those not on systemic corticosteroids, for a total of 1,332 matched patients," she said. "We calculated adjusted risk for acute lung injury, invasive ventilation, and in-hospital mortality from the propensity score–matched sample using a conditional logistic regression model."
Of the 5,584 patients, 458 were on systemic corticosteroids at the time of hospitalization and 5,126 were not. Among the systemic corticosteroid group, 34 (7.4%) developed ALI, compared with 343 (6.7%) of those not taking them, Dr. Karnatovskaia reported. In the systemic corticosteroid group, 104 patients (23%) required mechanical ventilation and 35 patients (8%) died, compared with 1,752 (34%) and 172 (3%) of those not taking systemic corticosteroids, she said.
On univariate analysis, systemic corticosteroid patients were more likely to be older, to be white, and to have diabetes, chronic obstructive pulmonary disease, malignancy, or previous chest radiation, Dr. Karnatovskaia said, noting that they were also more likely to have a lower body mass index and to be on a statin drug, inhaled steroid, inhaled beta-agonist, proton pump inhibitor, ACE inhibitor, angiotensin receptor blocker, or insulin and were less like likely to abuse alcohol or smoke tobacco.
After adjustment for significant covariates, systemic corticosteroid use was not independently associated with the development of ALI or the need for invasive ventilation, but did appear to be an independent predictor of ICU and hospital mortality, Dr. Karnatovskaia said. The latter association fell away, however, in the propensity score–based analysis. "Following propensity score–based analysis with matching, the association of prehospital systemic corticosteroids with mortality no longer remained significant," she said.
The findings are limited by the lack of data on the indication for systemic corticosteroid therapy, its duration, "and even whether it was continued throughout the hospital stay," as well as the fact that patients on prehospital systemic corticosteroids appeared to have worse functional status, which might have influenced their outcomes, according to Dr. Karnatovskaia. Although using the propensity score with matching addressed this as well as other hidden biases, "the potential for unmeasured effects remains," she said.
The study’s strengths include the large number of patients at risk for ALI enrolled from different centers and regions in the United States, as well as two hospitals in Turkey, and the use of comprehensive propensity score–based analysis with matching in addition to traditional logistic regression, Dr. Karnatovskaia said.
Ideally, the finding that prehospital use of systemic corticosteroids does not mitigate the development of ALI would be validated in a randomized controlled trial to best address any causal relationship, "but such a study would not be practical," Dr. Karnatovskaia said.
Dr. Karnatovskaia reported having no relevant financial disclosures.
HOUSTON – Prehospital use of systemic corticosteroids does not prevent the development of acute lung injury in at-risk patients, according to data reported at the annual congress of the Society of Critical Care Medicine.
In the first study to specifically evaluate the prophylactic value of prehospital systemic corticosteroids in patients with at least one risk factor for acute lung injury (ALI), Dr. Lioudmila Karnatovskaia of the Mayo Clinic in Jacksonville, Fla., and colleagues found a statistically similar incidence of ALI among at-risk patients who were and were not taking systemic corticosteroids at the time of hospitalization.
The investigators also determined that prehospital use of systemic corticosteroids did not affect the need for mechanical ventilation or overall mortality – a finding that appears to contradict previous studies that have linked preventive steroids in at-risk patients with increased rates of ALI and acute respiratory distress syndrome, Dr. Karnatovskaia said.
The study was a planned exploratory subgroup analysis of the Lung Injury Prediction Score cohort of the U.S. Critical Illness and Injury Trials Group, which prospectively enrolled 5,584 patients who were admitted to 22 acute care hospitals and who had predisposing conditions for ALI, including sepsis, shock, pancreatitis, pneumonia, aspiration, high-risk trauma, and high-risk surgery. The primary outcome was the development of ALI, and secondary outcomes were need for invasive ventilation and ICU and hospital mortality, Dr. Karnatovskaia said, noting that the data were analyzed using univariate, logistic regression, and propensity score–based analyses.
For the propensity analysis, "the propensity score balanced all of the covariates. Of the 458 patients on systemic corticosteroids, 443 were matched up to 1:4 to those not on systemic corticosteroids, for a total of 1,332 matched patients," she said. "We calculated adjusted risk for acute lung injury, invasive ventilation, and in-hospital mortality from the propensity score–matched sample using a conditional logistic regression model."
Of the 5,584 patients, 458 were on systemic corticosteroids at the time of hospitalization and 5,126 were not. Among the systemic corticosteroid group, 34 (7.4%) developed ALI, compared with 343 (6.7%) of those not taking them, Dr. Karnatovskaia reported. In the systemic corticosteroid group, 104 patients (23%) required mechanical ventilation and 35 patients (8%) died, compared with 1,752 (34%) and 172 (3%) of those not taking systemic corticosteroids, she said.
On univariate analysis, systemic corticosteroid patients were more likely to be older, to be white, and to have diabetes, chronic obstructive pulmonary disease, malignancy, or previous chest radiation, Dr. Karnatovskaia said, noting that they were also more likely to have a lower body mass index and to be on a statin drug, inhaled steroid, inhaled beta-agonist, proton pump inhibitor, ACE inhibitor, angiotensin receptor blocker, or insulin and were less like likely to abuse alcohol or smoke tobacco.
After adjustment for significant covariates, systemic corticosteroid use was not independently associated with the development of ALI or the need for invasive ventilation, but did appear to be an independent predictor of ICU and hospital mortality, Dr. Karnatovskaia said. The latter association fell away, however, in the propensity score–based analysis. "Following propensity score–based analysis with matching, the association of prehospital systemic corticosteroids with mortality no longer remained significant," she said.
The findings are limited by the lack of data on the indication for systemic corticosteroid therapy, its duration, "and even whether it was continued throughout the hospital stay," as well as the fact that patients on prehospital systemic corticosteroids appeared to have worse functional status, which might have influenced their outcomes, according to Dr. Karnatovskaia. Although using the propensity score with matching addressed this as well as other hidden biases, "the potential for unmeasured effects remains," she said.
The study’s strengths include the large number of patients at risk for ALI enrolled from different centers and regions in the United States, as well as two hospitals in Turkey, and the use of comprehensive propensity score–based analysis with matching in addition to traditional logistic regression, Dr. Karnatovskaia said.
Ideally, the finding that prehospital use of systemic corticosteroids does not mitigate the development of ALI would be validated in a randomized controlled trial to best address any causal relationship, "but such a study would not be practical," Dr. Karnatovskaia said.
Dr. Karnatovskaia reported having no relevant financial disclosures.
FROM THE ANNUAL CONGRESS OF THE SOCIETY OF CRITICAL CARE MEDICINE
EDEN Trial Questions Restricting Nutrition to ALI Patients
HOUSTON – Restricting the amount of initial enteral intake in mechanically ventilated patients who have acute lung injury neither reduces the duration of mechanical ventilation nor improves mortality relative to full enteral feeding, but the nutritional strategy may be slightly easier on the stomach, according to a study reported Feb. 5 at the annual meeting of the Society of Critical Care Medicine Critical Care Congress.
The importance of nutrition support in critically ill patients with acute lung injury (ALI) is well accepted as a means of maintaining gut integrity, modulating both stress and the systemic immune response, and attenuating disease severity, but conflicting data regarding the timing, formulation, and amount of enteral nutrition have contributed to uncertainty about the optimal feeding protocol, according to Dr. Todd W. Rice of Vanderbilt University Medical Center in Nashville, Tenn.
"How much nutrition we need to promote the protective benefits, we don’t know. Providing a little bit of nutrition (called trophic feeding) has been shown to decrease intestinal intolerances, compared with full-calorie feeds, but it may do so at the risk of malnutrition, worse immune function, and loss of muscle strength," he said. Full-calorie feeding, on the other hand, may lead to more intolerances, may cause hyperglycemia and other imbalances, may increase septic complications, and may fuel the inflammatory fire, he added.
In the current study, which was published simultaneously in JAMA, Dr. Rice and colleagues in the EDEN (Early Vs. Delayed Enteral Nutrition in ALI) trial, sought to examine the relative advantages of restricting the amount of initial enteral intake in mechanically ventilated ALI patients. Specifically, the prospective, randomized, open-label trial compared the effect on clinical outcomes and survival of initial trophic enteral feeding – approximately 25% of the full target feeding – with initial full-calorie feeding for the first 6 days of mechanical ventilation in ALI patients. "We hypothesized that reduced trophic feeding during the first [6 days] would increase ventilator-free days and reduce instances of gastrointestinal intolerances compared with the conventional full enteral nutrition strategy," he said.
"How much nutrition we need to promote the protective benefits, we don’t know."
The study’s primary end point was ventilator-free days through day 28; secondary end points were daily percentage of goal enteral feeding, frequency of gastrointestinal intolerances, 60-day mortality before hospital discharge with unassisted breathing, ICU- and organ failure–free days, and new infections (JAMA 2012 Feb. 5 [doi:10.1001/jama2012.137]).
The multicenter study population comprised 1,000 patients, from January 2008 through mid-April 2011, who were initiated on mechanical ventilation within 48 hours of developing ALI. Within 6 hours of randomization, enteric nutrition was initiated in 508 patients assigned to trophic nutrition and 492 assigned to full feeding, and was continued until death, extubation, or day 6, Dr. Rice explained. Per standard protocol, enteral nutrition in the full-feeding group began at 25 mL/hr and advanced to goal weights (25-30 kcal/day of nonprotein calories and 1.2-1.6 g/kg per day of protein) as quickly as possible; gastric residual volumes were checked every 6 hours while enteral feeding was increased. In the trophic group, enteral feeding was initiated at 10-20 kcal/hr and gastric residual volumes were checked every 12 hours. After 6 days, patients in the trophic group who still required mechanical ventilation were advanced to the full-energy feeding rates, he said.
Baseline characteristics of the two groups were similar, Dr. Rice noted. "The primary etiologies of lung injury in both groups of patients were pneumonia and sepsis, and the average APACHE III [Acute Physiology and Chronic Health Evaluation III] score was approximately 92. These were sick patients," he said. For the first 6 days, the full- and trophic feeding groups received 1,300 kcal/day and 400 kcal/day, respectively.
With respect to the primary end point (28 days), the average number of ventilator-free days in both groups was similar, at 14.9 in the trophic group and 15.0 in the full-feeding group. "There were also no differences in 60-day mortality, organ failure–free days, ICU-free days, or the incidence of infection between groups," he said. Similarly, with respect to body mass index category or lung injury severity, "there were no between-group differences in ventilator free days or survival."
The full-feeding group did have a higher number of gastrointestinal intolerances on any one day, and statistically significant increase on days 2 and 3, but the overall percentages of intolerances were low, Dr. Rice said. There were no differences in albumin and protein levels between the groups over the first 7 days, he said.
Regarding the immediate clinical relevance of the findings, Dr. Rice stressed that the study wasn’t designed as an equivalence trial, "so I can’t tell you both feeding strategies are similar, but you can look at the results." In fact, he said, although the study did not show a benefit other than improved gastrointestinal tolerance, his group has moved toward trophic feeds because of the ease of administration. "Our nurses love the trophic feeds. Starting at 10-20 cc/hr and running it for 6 days is a lot less hassle than worrying about trying to ramp it up and get to goals," he said.
"Looking ahead, there are a number of places to go" with this research, Dr. Rice said. "Some of the questions we’ve thought about are what role does this play in the [total parenteral nutrition] question, and whether we need to be feeding patients at all. Initially, we thought the idea of not feeding patients would be a hard study to sell, but with these data, it may not be an unreasonable thing to look at."
Dr. Rice disclosed no financial conflicts of interest.
HOUSTON – Restricting the amount of initial enteral intake in mechanically ventilated patients who have acute lung injury neither reduces the duration of mechanical ventilation nor improves mortality relative to full enteral feeding, but the nutritional strategy may be slightly easier on the stomach, according to a study reported Feb. 5 at the annual meeting of the Society of Critical Care Medicine Critical Care Congress.
The importance of nutrition support in critically ill patients with acute lung injury (ALI) is well accepted as a means of maintaining gut integrity, modulating both stress and the systemic immune response, and attenuating disease severity, but conflicting data regarding the timing, formulation, and amount of enteral nutrition have contributed to uncertainty about the optimal feeding protocol, according to Dr. Todd W. Rice of Vanderbilt University Medical Center in Nashville, Tenn.
"How much nutrition we need to promote the protective benefits, we don’t know. Providing a little bit of nutrition (called trophic feeding) has been shown to decrease intestinal intolerances, compared with full-calorie feeds, but it may do so at the risk of malnutrition, worse immune function, and loss of muscle strength," he said. Full-calorie feeding, on the other hand, may lead to more intolerances, may cause hyperglycemia and other imbalances, may increase septic complications, and may fuel the inflammatory fire, he added.
In the current study, which was published simultaneously in JAMA, Dr. Rice and colleagues in the EDEN (Early Vs. Delayed Enteral Nutrition in ALI) trial, sought to examine the relative advantages of restricting the amount of initial enteral intake in mechanically ventilated ALI patients. Specifically, the prospective, randomized, open-label trial compared the effect on clinical outcomes and survival of initial trophic enteral feeding – approximately 25% of the full target feeding – with initial full-calorie feeding for the first 6 days of mechanical ventilation in ALI patients. "We hypothesized that reduced trophic feeding during the first [6 days] would increase ventilator-free days and reduce instances of gastrointestinal intolerances compared with the conventional full enteral nutrition strategy," he said.
"How much nutrition we need to promote the protective benefits, we don’t know."
The study’s primary end point was ventilator-free days through day 28; secondary end points were daily percentage of goal enteral feeding, frequency of gastrointestinal intolerances, 60-day mortality before hospital discharge with unassisted breathing, ICU- and organ failure–free days, and new infections (JAMA 2012 Feb. 5 [doi:10.1001/jama2012.137]).
The multicenter study population comprised 1,000 patients, from January 2008 through mid-April 2011, who were initiated on mechanical ventilation within 48 hours of developing ALI. Within 6 hours of randomization, enteric nutrition was initiated in 508 patients assigned to trophic nutrition and 492 assigned to full feeding, and was continued until death, extubation, or day 6, Dr. Rice explained. Per standard protocol, enteral nutrition in the full-feeding group began at 25 mL/hr and advanced to goal weights (25-30 kcal/day of nonprotein calories and 1.2-1.6 g/kg per day of protein) as quickly as possible; gastric residual volumes were checked every 6 hours while enteral feeding was increased. In the trophic group, enteral feeding was initiated at 10-20 kcal/hr and gastric residual volumes were checked every 12 hours. After 6 days, patients in the trophic group who still required mechanical ventilation were advanced to the full-energy feeding rates, he said.
Baseline characteristics of the two groups were similar, Dr. Rice noted. "The primary etiologies of lung injury in both groups of patients were pneumonia and sepsis, and the average APACHE III [Acute Physiology and Chronic Health Evaluation III] score was approximately 92. These were sick patients," he said. For the first 6 days, the full- and trophic feeding groups received 1,300 kcal/day and 400 kcal/day, respectively.
With respect to the primary end point (28 days), the average number of ventilator-free days in both groups was similar, at 14.9 in the trophic group and 15.0 in the full-feeding group. "There were also no differences in 60-day mortality, organ failure–free days, ICU-free days, or the incidence of infection between groups," he said. Similarly, with respect to body mass index category or lung injury severity, "there were no between-group differences in ventilator free days or survival."
The full-feeding group did have a higher number of gastrointestinal intolerances on any one day, and statistically significant increase on days 2 and 3, but the overall percentages of intolerances were low, Dr. Rice said. There were no differences in albumin and protein levels between the groups over the first 7 days, he said.
Regarding the immediate clinical relevance of the findings, Dr. Rice stressed that the study wasn’t designed as an equivalence trial, "so I can’t tell you both feeding strategies are similar, but you can look at the results." In fact, he said, although the study did not show a benefit other than improved gastrointestinal tolerance, his group has moved toward trophic feeds because of the ease of administration. "Our nurses love the trophic feeds. Starting at 10-20 cc/hr and running it for 6 days is a lot less hassle than worrying about trying to ramp it up and get to goals," he said.
"Looking ahead, there are a number of places to go" with this research, Dr. Rice said. "Some of the questions we’ve thought about are what role does this play in the [total parenteral nutrition] question, and whether we need to be feeding patients at all. Initially, we thought the idea of not feeding patients would be a hard study to sell, but with these data, it may not be an unreasonable thing to look at."
Dr. Rice disclosed no financial conflicts of interest.
HOUSTON – Restricting the amount of initial enteral intake in mechanically ventilated patients who have acute lung injury neither reduces the duration of mechanical ventilation nor improves mortality relative to full enteral feeding, but the nutritional strategy may be slightly easier on the stomach, according to a study reported Feb. 5 at the annual meeting of the Society of Critical Care Medicine Critical Care Congress.
The importance of nutrition support in critically ill patients with acute lung injury (ALI) is well accepted as a means of maintaining gut integrity, modulating both stress and the systemic immune response, and attenuating disease severity, but conflicting data regarding the timing, formulation, and amount of enteral nutrition have contributed to uncertainty about the optimal feeding protocol, according to Dr. Todd W. Rice of Vanderbilt University Medical Center in Nashville, Tenn.
"How much nutrition we need to promote the protective benefits, we don’t know. Providing a little bit of nutrition (called trophic feeding) has been shown to decrease intestinal intolerances, compared with full-calorie feeds, but it may do so at the risk of malnutrition, worse immune function, and loss of muscle strength," he said. Full-calorie feeding, on the other hand, may lead to more intolerances, may cause hyperglycemia and other imbalances, may increase septic complications, and may fuel the inflammatory fire, he added.
In the current study, which was published simultaneously in JAMA, Dr. Rice and colleagues in the EDEN (Early Vs. Delayed Enteral Nutrition in ALI) trial, sought to examine the relative advantages of restricting the amount of initial enteral intake in mechanically ventilated ALI patients. Specifically, the prospective, randomized, open-label trial compared the effect on clinical outcomes and survival of initial trophic enteral feeding – approximately 25% of the full target feeding – with initial full-calorie feeding for the first 6 days of mechanical ventilation in ALI patients. "We hypothesized that reduced trophic feeding during the first [6 days] would increase ventilator-free days and reduce instances of gastrointestinal intolerances compared with the conventional full enteral nutrition strategy," he said.
"How much nutrition we need to promote the protective benefits, we don’t know."
The study’s primary end point was ventilator-free days through day 28; secondary end points were daily percentage of goal enteral feeding, frequency of gastrointestinal intolerances, 60-day mortality before hospital discharge with unassisted breathing, ICU- and organ failure–free days, and new infections (JAMA 2012 Feb. 5 [doi:10.1001/jama2012.137]).
The multicenter study population comprised 1,000 patients, from January 2008 through mid-April 2011, who were initiated on mechanical ventilation within 48 hours of developing ALI. Within 6 hours of randomization, enteric nutrition was initiated in 508 patients assigned to trophic nutrition and 492 assigned to full feeding, and was continued until death, extubation, or day 6, Dr. Rice explained. Per standard protocol, enteral nutrition in the full-feeding group began at 25 mL/hr and advanced to goal weights (25-30 kcal/day of nonprotein calories and 1.2-1.6 g/kg per day of protein) as quickly as possible; gastric residual volumes were checked every 6 hours while enteral feeding was increased. In the trophic group, enteral feeding was initiated at 10-20 kcal/hr and gastric residual volumes were checked every 12 hours. After 6 days, patients in the trophic group who still required mechanical ventilation were advanced to the full-energy feeding rates, he said.
Baseline characteristics of the two groups were similar, Dr. Rice noted. "The primary etiologies of lung injury in both groups of patients were pneumonia and sepsis, and the average APACHE III [Acute Physiology and Chronic Health Evaluation III] score was approximately 92. These were sick patients," he said. For the first 6 days, the full- and trophic feeding groups received 1,300 kcal/day and 400 kcal/day, respectively.
With respect to the primary end point (28 days), the average number of ventilator-free days in both groups was similar, at 14.9 in the trophic group and 15.0 in the full-feeding group. "There were also no differences in 60-day mortality, organ failure–free days, ICU-free days, or the incidence of infection between groups," he said. Similarly, with respect to body mass index category or lung injury severity, "there were no between-group differences in ventilator free days or survival."
The full-feeding group did have a higher number of gastrointestinal intolerances on any one day, and statistically significant increase on days 2 and 3, but the overall percentages of intolerances were low, Dr. Rice said. There were no differences in albumin and protein levels between the groups over the first 7 days, he said.
Regarding the immediate clinical relevance of the findings, Dr. Rice stressed that the study wasn’t designed as an equivalence trial, "so I can’t tell you both feeding strategies are similar, but you can look at the results." In fact, he said, although the study did not show a benefit other than improved gastrointestinal tolerance, his group has moved toward trophic feeds because of the ease of administration. "Our nurses love the trophic feeds. Starting at 10-20 cc/hr and running it for 6 days is a lot less hassle than worrying about trying to ramp it up and get to goals," he said.
"Looking ahead, there are a number of places to go" with this research, Dr. Rice said. "Some of the questions we’ve thought about are what role does this play in the [total parenteral nutrition] question, and whether we need to be feeding patients at all. Initially, we thought the idea of not feeding patients would be a hard study to sell, but with these data, it may not be an unreasonable thing to look at."
Dr. Rice disclosed no financial conflicts of interest.
FROM THE ANNUAL CONGRESS OF THE SOCIETY OF CRITICAL CARE MEDICINE