User login
Society of Gynecologic Oncology (SGO): Annual Meeting on Women's Cancer
Timely palliative consult affects end-of-life care in gynecologic cancer patients
LOS ANGELES – A palliative care consultation within the last month of life improves a variety of end-of-life outcomes in patients dying from gynecologic cancers, based on a retrospective analysis.
Among the 100 patients studied, about one-fourth had a timely palliative care consultation, defined in one study as 14 days before death and in another study as 30 days before death, lead investigator Dr. Nicole S. Nevadunsky of Montefiore Medical Center, New York, reported at the annual meeting of the Society of Gynecologic Oncology.
Compared with their counterparts who had late or no consultations, patients who had timely consultations had lower scores for aggressive end-of-life events such as emergency department visits, chemotherapy, and death in an acute care setting.
In addition, in their last 14 days of life, this group had median direct inpatient hospital costs that were $5,106 less, and they were half as likely to be admitted.
"Our data suggest that early palliative medicine consultation results in decreased aggressive measures at the end of life [and] was associated with decreased direct inpatient costs for women who died from gynecologic malignancies," Dr. Nevadunsky noted. "Further research is needed to evaluate the quality of life in relation to [the aggressiveness of care] for patients and their families."
While it is unclear how many gynecologic oncologists are also board certified in palliative care, "I think more clinicians actually do palliative medicine as part of their everyday practice," Dr. Nevadunsky said. Also, palliative care is truly a multidisciplinary undertaking involving, for example, nurses, pastoral care personnel, social workers, and others.
"As far as the best metric for palliative medicine, I think it is quality of life. But how to define that is extremely complicated and still evolving," she added.
"I think it’s an experience where the patient is getting what they want most out of things, and sometimes that’s saying to the patient, ‘If we can’t cure you, what is the most important thing to you?’ " she replied. "Each patient is different, and that’s what makes (defining quality of life) so complicated."
The American Society of Clinical Oncology recommends consideration of palliative care early in the course of metastatic or symptomatic disease.
"This is a very vague recommendation: who, what, when, where, how? How will patients respond to this? Who’s going to pay for this? What’s the patient going to get out of this?" Dr. Nevadunsky commented.
She and her colleagues studied 100 consecutive patients who died from gynecologic cancer between 2006 and 2009 and received care at Montefiore in the year before death.
In the first study, they defined a timely palliative care consultation as one occurring more than 30 days before death.
"The ideal timing for palliative medicine consultation is unknown; however, 30 days was chosen as the minimal exposure time because the standard metrics utilized to compare aggressive measures at the end of life included a minimum of 30 days," Dr. Nevadunsky explained.
"Overall, I was surprised to find that 49 of the 100 women actually had a palliative medicine consultation at some time or another during their care," she said.
However, the median number of days between consultation and death was 16, and only 18% of patients had a timely consultation.
Late diagnosis did not explain this finding, as less than 10% of patients received their diagnosis in the month before they died.
"The scope of this study was not inclusive to determine why this [late palliative care consultation] was happening," Dr. Nevadunsky said. Data showed that although the two groups were demographically similar, the patients who received a timely consultation were more likely to be married.
The group with timely consultations were less likely to receive aggressive end-of-life care, based on measures of eight indicators of aggressive care (0 vs. 2, P = .025).
The difference between those patients who had timely consultation and those with untimely or no consultation was greatest for the indicators of a hospital stay lasting more than 14 days in the last month of life (22% vs. 40%) and death in the acute care setting (28% vs. 45%).
In the second study, the investigators found that 29% of patients had a timely palliative care consultation, defined in this case as one occurring 14 days or more before death.
Patients with a timely consultation had lower median direct hospital inpatient costs per day in the last 30 days of life ($613 vs. $702, P = .02). They also had lower median direct hospital inpatient costs in the last 14 days overall ($0 vs. $5,106, P = .007) and on a per-day basis ($0 vs. $676, P = .007).
"The patients who had the timely consultations actually weren’t admitted to the hospital as often," Dr. Nevadunsky noted. In fact, they were half as likely to be admitted in the last 14 days (35% vs. 71%, P = .001).
"Shortcomings [of the study] include small numbers and the retrospective collection of data. Also, our study did not account for outpatient costs, including those assumed by families, or for those costs incurred by loss of time out of work by families to care for the patient," acknowledged Dr. Nevadunsky, who disclosed no relevant conflicts of interest.
LOS ANGELES – A palliative care consultation within the last month of life improves a variety of end-of-life outcomes in patients dying from gynecologic cancers, based on a retrospective analysis.
Among the 100 patients studied, about one-fourth had a timely palliative care consultation, defined in one study as 14 days before death and in another study as 30 days before death, lead investigator Dr. Nicole S. Nevadunsky of Montefiore Medical Center, New York, reported at the annual meeting of the Society of Gynecologic Oncology.
Compared with their counterparts who had late or no consultations, patients who had timely consultations had lower scores for aggressive end-of-life events such as emergency department visits, chemotherapy, and death in an acute care setting.
In addition, in their last 14 days of life, this group had median direct inpatient hospital costs that were $5,106 less, and they were half as likely to be admitted.
"Our data suggest that early palliative medicine consultation results in decreased aggressive measures at the end of life [and] was associated with decreased direct inpatient costs for women who died from gynecologic malignancies," Dr. Nevadunsky noted. "Further research is needed to evaluate the quality of life in relation to [the aggressiveness of care] for patients and their families."
While it is unclear how many gynecologic oncologists are also board certified in palliative care, "I think more clinicians actually do palliative medicine as part of their everyday practice," Dr. Nevadunsky said. Also, palliative care is truly a multidisciplinary undertaking involving, for example, nurses, pastoral care personnel, social workers, and others.
"As far as the best metric for palliative medicine, I think it is quality of life. But how to define that is extremely complicated and still evolving," she added.
"I think it’s an experience where the patient is getting what they want most out of things, and sometimes that’s saying to the patient, ‘If we can’t cure you, what is the most important thing to you?’ " she replied. "Each patient is different, and that’s what makes (defining quality of life) so complicated."
The American Society of Clinical Oncology recommends consideration of palliative care early in the course of metastatic or symptomatic disease.
"This is a very vague recommendation: who, what, when, where, how? How will patients respond to this? Who’s going to pay for this? What’s the patient going to get out of this?" Dr. Nevadunsky commented.
She and her colleagues studied 100 consecutive patients who died from gynecologic cancer between 2006 and 2009 and received care at Montefiore in the year before death.
In the first study, they defined a timely palliative care consultation as one occurring more than 30 days before death.
"The ideal timing for palliative medicine consultation is unknown; however, 30 days was chosen as the minimal exposure time because the standard metrics utilized to compare aggressive measures at the end of life included a minimum of 30 days," Dr. Nevadunsky explained.
"Overall, I was surprised to find that 49 of the 100 women actually had a palliative medicine consultation at some time or another during their care," she said.
However, the median number of days between consultation and death was 16, and only 18% of patients had a timely consultation.
Late diagnosis did not explain this finding, as less than 10% of patients received their diagnosis in the month before they died.
"The scope of this study was not inclusive to determine why this [late palliative care consultation] was happening," Dr. Nevadunsky said. Data showed that although the two groups were demographically similar, the patients who received a timely consultation were more likely to be married.
The group with timely consultations were less likely to receive aggressive end-of-life care, based on measures of eight indicators of aggressive care (0 vs. 2, P = .025).
The difference between those patients who had timely consultation and those with untimely or no consultation was greatest for the indicators of a hospital stay lasting more than 14 days in the last month of life (22% vs. 40%) and death in the acute care setting (28% vs. 45%).
In the second study, the investigators found that 29% of patients had a timely palliative care consultation, defined in this case as one occurring 14 days or more before death.
Patients with a timely consultation had lower median direct hospital inpatient costs per day in the last 30 days of life ($613 vs. $702, P = .02). They also had lower median direct hospital inpatient costs in the last 14 days overall ($0 vs. $5,106, P = .007) and on a per-day basis ($0 vs. $676, P = .007).
"The patients who had the timely consultations actually weren’t admitted to the hospital as often," Dr. Nevadunsky noted. In fact, they were half as likely to be admitted in the last 14 days (35% vs. 71%, P = .001).
"Shortcomings [of the study] include small numbers and the retrospective collection of data. Also, our study did not account for outpatient costs, including those assumed by families, or for those costs incurred by loss of time out of work by families to care for the patient," acknowledged Dr. Nevadunsky, who disclosed no relevant conflicts of interest.
LOS ANGELES – A palliative care consultation within the last month of life improves a variety of end-of-life outcomes in patients dying from gynecologic cancers, based on a retrospective analysis.
Among the 100 patients studied, about one-fourth had a timely palliative care consultation, defined in one study as 14 days before death and in another study as 30 days before death, lead investigator Dr. Nicole S. Nevadunsky of Montefiore Medical Center, New York, reported at the annual meeting of the Society of Gynecologic Oncology.
Compared with their counterparts who had late or no consultations, patients who had timely consultations had lower scores for aggressive end-of-life events such as emergency department visits, chemotherapy, and death in an acute care setting.
In addition, in their last 14 days of life, this group had median direct inpatient hospital costs that were $5,106 less, and they were half as likely to be admitted.
"Our data suggest that early palliative medicine consultation results in decreased aggressive measures at the end of life [and] was associated with decreased direct inpatient costs for women who died from gynecologic malignancies," Dr. Nevadunsky noted. "Further research is needed to evaluate the quality of life in relation to [the aggressiveness of care] for patients and their families."
While it is unclear how many gynecologic oncologists are also board certified in palliative care, "I think more clinicians actually do palliative medicine as part of their everyday practice," Dr. Nevadunsky said. Also, palliative care is truly a multidisciplinary undertaking involving, for example, nurses, pastoral care personnel, social workers, and others.
"As far as the best metric for palliative medicine, I think it is quality of life. But how to define that is extremely complicated and still evolving," she added.
"I think it’s an experience where the patient is getting what they want most out of things, and sometimes that’s saying to the patient, ‘If we can’t cure you, what is the most important thing to you?’ " she replied. "Each patient is different, and that’s what makes (defining quality of life) so complicated."
The American Society of Clinical Oncology recommends consideration of palliative care early in the course of metastatic or symptomatic disease.
"This is a very vague recommendation: who, what, when, where, how? How will patients respond to this? Who’s going to pay for this? What’s the patient going to get out of this?" Dr. Nevadunsky commented.
She and her colleagues studied 100 consecutive patients who died from gynecologic cancer between 2006 and 2009 and received care at Montefiore in the year before death.
In the first study, they defined a timely palliative care consultation as one occurring more than 30 days before death.
"The ideal timing for palliative medicine consultation is unknown; however, 30 days was chosen as the minimal exposure time because the standard metrics utilized to compare aggressive measures at the end of life included a minimum of 30 days," Dr. Nevadunsky explained.
"Overall, I was surprised to find that 49 of the 100 women actually had a palliative medicine consultation at some time or another during their care," she said.
However, the median number of days between consultation and death was 16, and only 18% of patients had a timely consultation.
Late diagnosis did not explain this finding, as less than 10% of patients received their diagnosis in the month before they died.
"The scope of this study was not inclusive to determine why this [late palliative care consultation] was happening," Dr. Nevadunsky said. Data showed that although the two groups were demographically similar, the patients who received a timely consultation were more likely to be married.
The group with timely consultations were less likely to receive aggressive end-of-life care, based on measures of eight indicators of aggressive care (0 vs. 2, P = .025).
The difference between those patients who had timely consultation and those with untimely or no consultation was greatest for the indicators of a hospital stay lasting more than 14 days in the last month of life (22% vs. 40%) and death in the acute care setting (28% vs. 45%).
In the second study, the investigators found that 29% of patients had a timely palliative care consultation, defined in this case as one occurring 14 days or more before death.
Patients with a timely consultation had lower median direct hospital inpatient costs per day in the last 30 days of life ($613 vs. $702, P = .02). They also had lower median direct hospital inpatient costs in the last 14 days overall ($0 vs. $5,106, P = .007) and on a per-day basis ($0 vs. $676, P = .007).
"The patients who had the timely consultations actually weren’t admitted to the hospital as often," Dr. Nevadunsky noted. In fact, they were half as likely to be admitted in the last 14 days (35% vs. 71%, P = .001).
"Shortcomings [of the study] include small numbers and the retrospective collection of data. Also, our study did not account for outpatient costs, including those assumed by families, or for those costs incurred by loss of time out of work by families to care for the patient," acknowledged Dr. Nevadunsky, who disclosed no relevant conflicts of interest.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: Patients receiving timely palliative care had lower scores for aggressive care at the end of life (0 vs. 2) and, in their last 14 days, had lower median direct inpatient hospital costs ($0 vs. $5,106) and were half as likely to be admitted (35% vs. 71%).
Data source: A pair of retrospective cohort studies among 100 patients who died from gynecologic cancers.
Disclosures: Dr. Nevadunsky disclosed no relevant conflicts of interest.
Intraperitoneal chemo superior in low-volume residual ovarian cancer
LOS ANGELES – Patients with resected advanced ovarian cancer and low-volume residual disease fare better in the long term with intraperitoneal chemotherapy instead of intravenous chemotherapy.
A team led by Dr. Devansu Tewari assessed outcomes in 876 women from two key Gynecologic Oncology Group trials: GOG 114 and GOG 172. Combined median follow-up in those trials approached 11 years.
Compared with their peers given intravenous chemotherapy, women given intraperitoneal (IP) chemotherapy had a 16% lower risk of progression or death and a 17% lower risk of death, according to results reported at the annual meeting of the Society of Gynecologic Oncology.
Benefit was evident regardless of the extent of residual disease. Also, each additional cycle of IP chemotherapy reduced the risk of death by 12%.
"A strength of this study is that it is a combined analysis of these two major IP trials that looked at long-term follow-up and showed survival outcomes that are quite significant. The defining difference between the two groups is that one received IP therapy and one did not, as it is very unlikely that IP therapy would have been administered in the recurrent setting," Dr. Tewari commented.
Although more than 7 years have elapsed since the National Cancer Institute recommended consideration of IP chemotherapy for advanced-stage low-volume ovarian cancer, uptake of this therapy has been limited given lingering questions about efficacy, safety, and issues such as the ideal regimen, noted Dr. Tewari, who is director of gynecologic oncology for the Southern California Permanente Medical Group in Orange County, California, and assistant professor of ob.gyn. at the University of California, Irvine.
"We have now updated the results of GOG 172 and GOG 114. But we also acknowledge that in the last 7 years, a lot has changed in the treatment of ovarian cancer in which these advantages may be further enhanced," he noted, for example, through use of bevacizumab (Avastin) and dose-dense therapy.
In particular, oncologists are awaiting results of the recently completed GOG 262 trial (assessing the role of bevacizumab and dose-dense paclitaxel) and the GOG 252 trial (assessing the role of IP carboplatin, bevacizumab, and dose-dense paclitaxel).
"We hope that the results of these studies, combined with the findings before, will bring in the foundation that we need to move forward in terms of laying the groundwork for treating women individually and tailoring their treatment for this cancer specifically for them," Dr. Tewari said.
One session attendee, noting the IP regimens used in the trials studied, asked, "Is it the dose-dense treatment or the IP that actually matters?"
"That’s a very good question. The whole issue with GOG 172 was essentially partial deployment of dose dense because patients [in the IP arm] received [an additional] day 8 treatment, so it has to be acknowledged," Dr. Tewari replied. "I think the answer is going to really come about when we see the findings of GOG 252."
Attendee Dr. Joan Walker of the University of Oklahoma, Oklahoma City, said, "I want to thank the presenters for emphasizing IP chemotherapy with cisplatin, and I think that it still needs to be emphasized."
She noted that the long-term survival gains being seen with IP chemotherapy are "just amazing. And we don’t know why that is, but obviously if GOG 104, 114, and 172 all show the same thing, it can’t necessarily be that the Taxol [paclitaxel] IP is the only contributing factor," she said.
"I think the future is bright for women and their survival, and it may be the bone marrow preservation of cisplatin that’s really causing the long-term effect because we know that patients get treated with multiple agents over and over again," Dr. Walker speculated.
The two trials that Dr. Tewari’s group studied – GOG 114 and GOG 172 – enrolled patients with resected stage III epithelial ovarian or peritoneal carcinoma who had residual disease measuring 1.0 cm or less.
The former trial compared IV carboplatin and paclitaxel with IP cisplatin; the latter trial compared IV paclitaxel with IP cisplatin and paclitaxel. About two-thirds of the women had macroscopic residual disease.
With a median follow-up of 10.7 years, relative to their counterparts given IV chemotherapy, women given IP chemotherapy had better progression-free survival (25 vs. 20 months; hazard ratio, 0.84; P = .03) and overall survival (62 vs. 51 months; hazard ratio, 0.83; P = .048).
The survival benefit of IP over IV chemotherapy was evident among both women with microscopic residual disease (5-year survival, 65% vs. 58%) and women with macroscopic residual disease (44% vs. 35%).
"There has been a lot of debate regarding the role of IP therapy in microscopic and macroscopic residual disease, and we saw an advantage in this cohort in both specific groups," commented Dr. Tewari.
Overall, half of patients given IP chemotherapy completed all six cycles of that chemotherapy. The risk of death fell with each additional cycle of IP chemotherapy (hazard ratio, 0.88, P less than .001).
Dr. Tewari disclosed no conflicts of interest related to the research.
LOS ANGELES – Patients with resected advanced ovarian cancer and low-volume residual disease fare better in the long term with intraperitoneal chemotherapy instead of intravenous chemotherapy.
A team led by Dr. Devansu Tewari assessed outcomes in 876 women from two key Gynecologic Oncology Group trials: GOG 114 and GOG 172. Combined median follow-up in those trials approached 11 years.
Compared with their peers given intravenous chemotherapy, women given intraperitoneal (IP) chemotherapy had a 16% lower risk of progression or death and a 17% lower risk of death, according to results reported at the annual meeting of the Society of Gynecologic Oncology.
Benefit was evident regardless of the extent of residual disease. Also, each additional cycle of IP chemotherapy reduced the risk of death by 12%.
"A strength of this study is that it is a combined analysis of these two major IP trials that looked at long-term follow-up and showed survival outcomes that are quite significant. The defining difference between the two groups is that one received IP therapy and one did not, as it is very unlikely that IP therapy would have been administered in the recurrent setting," Dr. Tewari commented.
Although more than 7 years have elapsed since the National Cancer Institute recommended consideration of IP chemotherapy for advanced-stage low-volume ovarian cancer, uptake of this therapy has been limited given lingering questions about efficacy, safety, and issues such as the ideal regimen, noted Dr. Tewari, who is director of gynecologic oncology for the Southern California Permanente Medical Group in Orange County, California, and assistant professor of ob.gyn. at the University of California, Irvine.
"We have now updated the results of GOG 172 and GOG 114. But we also acknowledge that in the last 7 years, a lot has changed in the treatment of ovarian cancer in which these advantages may be further enhanced," he noted, for example, through use of bevacizumab (Avastin) and dose-dense therapy.
In particular, oncologists are awaiting results of the recently completed GOG 262 trial (assessing the role of bevacizumab and dose-dense paclitaxel) and the GOG 252 trial (assessing the role of IP carboplatin, bevacizumab, and dose-dense paclitaxel).
"We hope that the results of these studies, combined with the findings before, will bring in the foundation that we need to move forward in terms of laying the groundwork for treating women individually and tailoring their treatment for this cancer specifically for them," Dr. Tewari said.
One session attendee, noting the IP regimens used in the trials studied, asked, "Is it the dose-dense treatment or the IP that actually matters?"
"That’s a very good question. The whole issue with GOG 172 was essentially partial deployment of dose dense because patients [in the IP arm] received [an additional] day 8 treatment, so it has to be acknowledged," Dr. Tewari replied. "I think the answer is going to really come about when we see the findings of GOG 252."
Attendee Dr. Joan Walker of the University of Oklahoma, Oklahoma City, said, "I want to thank the presenters for emphasizing IP chemotherapy with cisplatin, and I think that it still needs to be emphasized."
She noted that the long-term survival gains being seen with IP chemotherapy are "just amazing. And we don’t know why that is, but obviously if GOG 104, 114, and 172 all show the same thing, it can’t necessarily be that the Taxol [paclitaxel] IP is the only contributing factor," she said.
"I think the future is bright for women and their survival, and it may be the bone marrow preservation of cisplatin that’s really causing the long-term effect because we know that patients get treated with multiple agents over and over again," Dr. Walker speculated.
The two trials that Dr. Tewari’s group studied – GOG 114 and GOG 172 – enrolled patients with resected stage III epithelial ovarian or peritoneal carcinoma who had residual disease measuring 1.0 cm or less.
The former trial compared IV carboplatin and paclitaxel with IP cisplatin; the latter trial compared IV paclitaxel with IP cisplatin and paclitaxel. About two-thirds of the women had macroscopic residual disease.
With a median follow-up of 10.7 years, relative to their counterparts given IV chemotherapy, women given IP chemotherapy had better progression-free survival (25 vs. 20 months; hazard ratio, 0.84; P = .03) and overall survival (62 vs. 51 months; hazard ratio, 0.83; P = .048).
The survival benefit of IP over IV chemotherapy was evident among both women with microscopic residual disease (5-year survival, 65% vs. 58%) and women with macroscopic residual disease (44% vs. 35%).
"There has been a lot of debate regarding the role of IP therapy in microscopic and macroscopic residual disease, and we saw an advantage in this cohort in both specific groups," commented Dr. Tewari.
Overall, half of patients given IP chemotherapy completed all six cycles of that chemotherapy. The risk of death fell with each additional cycle of IP chemotherapy (hazard ratio, 0.88, P less than .001).
Dr. Tewari disclosed no conflicts of interest related to the research.
LOS ANGELES – Patients with resected advanced ovarian cancer and low-volume residual disease fare better in the long term with intraperitoneal chemotherapy instead of intravenous chemotherapy.
A team led by Dr. Devansu Tewari assessed outcomes in 876 women from two key Gynecologic Oncology Group trials: GOG 114 and GOG 172. Combined median follow-up in those trials approached 11 years.
Compared with their peers given intravenous chemotherapy, women given intraperitoneal (IP) chemotherapy had a 16% lower risk of progression or death and a 17% lower risk of death, according to results reported at the annual meeting of the Society of Gynecologic Oncology.
Benefit was evident regardless of the extent of residual disease. Also, each additional cycle of IP chemotherapy reduced the risk of death by 12%.
"A strength of this study is that it is a combined analysis of these two major IP trials that looked at long-term follow-up and showed survival outcomes that are quite significant. The defining difference between the two groups is that one received IP therapy and one did not, as it is very unlikely that IP therapy would have been administered in the recurrent setting," Dr. Tewari commented.
Although more than 7 years have elapsed since the National Cancer Institute recommended consideration of IP chemotherapy for advanced-stage low-volume ovarian cancer, uptake of this therapy has been limited given lingering questions about efficacy, safety, and issues such as the ideal regimen, noted Dr. Tewari, who is director of gynecologic oncology for the Southern California Permanente Medical Group in Orange County, California, and assistant professor of ob.gyn. at the University of California, Irvine.
"We have now updated the results of GOG 172 and GOG 114. But we also acknowledge that in the last 7 years, a lot has changed in the treatment of ovarian cancer in which these advantages may be further enhanced," he noted, for example, through use of bevacizumab (Avastin) and dose-dense therapy.
In particular, oncologists are awaiting results of the recently completed GOG 262 trial (assessing the role of bevacizumab and dose-dense paclitaxel) and the GOG 252 trial (assessing the role of IP carboplatin, bevacizumab, and dose-dense paclitaxel).
"We hope that the results of these studies, combined with the findings before, will bring in the foundation that we need to move forward in terms of laying the groundwork for treating women individually and tailoring their treatment for this cancer specifically for them," Dr. Tewari said.
One session attendee, noting the IP regimens used in the trials studied, asked, "Is it the dose-dense treatment or the IP that actually matters?"
"That’s a very good question. The whole issue with GOG 172 was essentially partial deployment of dose dense because patients [in the IP arm] received [an additional] day 8 treatment, so it has to be acknowledged," Dr. Tewari replied. "I think the answer is going to really come about when we see the findings of GOG 252."
Attendee Dr. Joan Walker of the University of Oklahoma, Oklahoma City, said, "I want to thank the presenters for emphasizing IP chemotherapy with cisplatin, and I think that it still needs to be emphasized."
She noted that the long-term survival gains being seen with IP chemotherapy are "just amazing. And we don’t know why that is, but obviously if GOG 104, 114, and 172 all show the same thing, it can’t necessarily be that the Taxol [paclitaxel] IP is the only contributing factor," she said.
"I think the future is bright for women and their survival, and it may be the bone marrow preservation of cisplatin that’s really causing the long-term effect because we know that patients get treated with multiple agents over and over again," Dr. Walker speculated.
The two trials that Dr. Tewari’s group studied – GOG 114 and GOG 172 – enrolled patients with resected stage III epithelial ovarian or peritoneal carcinoma who had residual disease measuring 1.0 cm or less.
The former trial compared IV carboplatin and paclitaxel with IP cisplatin; the latter trial compared IV paclitaxel with IP cisplatin and paclitaxel. About two-thirds of the women had macroscopic residual disease.
With a median follow-up of 10.7 years, relative to their counterparts given IV chemotherapy, women given IP chemotherapy had better progression-free survival (25 vs. 20 months; hazard ratio, 0.84; P = .03) and overall survival (62 vs. 51 months; hazard ratio, 0.83; P = .048).
The survival benefit of IP over IV chemotherapy was evident among both women with microscopic residual disease (5-year survival, 65% vs. 58%) and women with macroscopic residual disease (44% vs. 35%).
"There has been a lot of debate regarding the role of IP therapy in microscopic and macroscopic residual disease, and we saw an advantage in this cohort in both specific groups," commented Dr. Tewari.
Overall, half of patients given IP chemotherapy completed all six cycles of that chemotherapy. The risk of death fell with each additional cycle of IP chemotherapy (hazard ratio, 0.88, P less than .001).
Dr. Tewari disclosed no conflicts of interest related to the research.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major Finding: With a median follow-up of nearly 11 years, relative to their counterparts given IV chemotherapy, women given IP chemotherapy had better progression-free survival (25 vs. 20 months; hazard ratio, 0.84; P = .03) and overall survival (62 vs. 51 months; hazard ratio, 0.83; P = .048).
Data Source: A combined analysis of the GOG 114 and GOG 172 trials comparing IP vs. IV chemotherapy in 876 patients with resected advanced ovarian cancer and low-volume residual disease.
Disclosures: Dr. Tewari disclosed no relevant conflicts of interest.
Photodynamic therapy looks promising in early CIN
LOS ANGELES – An investigational type of photodynamic therapy appears promising for treating early cervical intraepithelial neoplasia, finds a phase 2b trial reported at the annual meeting of the Society of Gynecologic Oncology.
A team led by Dr. Mark H. Einstein undertook a dose-finding study of hexaminolevulinate (HAL) gel coupled with photodynamic therapy in 262 patients with grade 1 or 2 cervical intraepithelial neoplasia (CIN1, CIN2).
Among patients with CIN2, nearly all of those treated with the highest dose of HAL and photodynamic therapy had a response at 3 months, compared with roughly half of their counterparts treated with placebo.
The therapy was associated with a higher rate of local reactions, but none had to discontinue treatment.
"The 5% HAL photodynamic therapy was effective in treating patients with CIN2. There seems to be a signal of efficacy in patients who have HPV 16 and 18 as well," which may help inform the design of future phase III trials, commented Dr. Einstein, who is director of clinical research for women’s health and gynecologic oncology at the Montefiore Medical Center, New York.
"This device was very easy to use and was very well tolerated by this patient population, with essentially self-limiting reactions," he added.
Dr. Einstein noted that new approaches are needed for dealing with CIN, given that it commonly occurs in young women of childbearing age, and that some current treatments aimed at obliterating these lesions make subsequent colposcopies difficult and increase the risk of preterm birth.
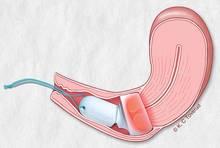
For photodynamic therapy, a photosensitizing agent is applied to the cervix and accumulates in the premalignant cells, he explained. When the area is illuminated at a specific energy, reactive oxygen species are generated, killing the cells.
"The hypothesized mechanism of photodynamic therapy in cervical lesions is that once the HAL is applied and light is emitted for about 5 hours, this induces some local apoptosis, and that will release a lot of HPV antigens from these dying cells. These are then presented to naive T cells in the locoregional lymph nodes, which then stimulates even more of a cell-mediated immune response and inflammatory response that then further increases apoptosis of local cells," Dr. Einstein elaborated. "And then, hypothetically, in other areas of the cervical and vaginal tract, you are going to get a big cell-mediated immune response."
Women in the trial, which was sponsored by Photocure, had pathologically confirmed, previously untreated CIN1 or CIN2.
They were randomized evenly to four groups treated with HAL 5%, 1%, or 0.2%, or placebo, and photodynamic therapy.
A gynecologist placed the integrated drug and device (Cevira, manufactured by Photocure) in the outpatient setting. Five hours after placement, the device self-activated and delivered photodynamic therapy for roughly 5 hours. The patients removed the device themselves thereafter.
The patients had a median age of 27 years, and 46% had CIN2. About half of those tested were found to have a high-risk type of HPV.
Among patients with CIN2, 5% HAL photodynamic therapy yielded a higher 3-month rate of response (based on histology, cytology, and HPV status) than did placebo, both overall (95% vs. 56%; P = .01) and in the subset who were positive for any type of HPV (92% vs. 50%; P = .02).
"Clearly, the placebo effect was very large in this group, and this is expected in young women who have CIN1 and CIN2. That being said, this was significant efficacy when compared to placebo," said Dr. Einstein, who disclosed that his institution has received funding from Photocure for educational speaking activities and research.
Additionally, among the patients with CIN2 who had HPV 16 or 18 infection, those treated with 5% HAL photodynamic therapy were more likely than were those treated with placebo to have clearance of the virus (83% vs. 0%; P = .02).
There was no significant benefit among women with CIN1 or among women treated with the lower doses of HAL.
Relative to their counterparts treated with placebo, patients treated with 5% HAL photodynamic therapy had a higher rate of self-limiting local reactions (54% vs. 32%); the most common were vaginal discharge and local discomfort. None of the patients discontinued treatment because of these reactions.
A total of five pregnancies were reported among study patients in the 3 months after treatment. All of these women delivered normal full-term infants.
LOS ANGELES – An investigational type of photodynamic therapy appears promising for treating early cervical intraepithelial neoplasia, finds a phase 2b trial reported at the annual meeting of the Society of Gynecologic Oncology.
A team led by Dr. Mark H. Einstein undertook a dose-finding study of hexaminolevulinate (HAL) gel coupled with photodynamic therapy in 262 patients with grade 1 or 2 cervical intraepithelial neoplasia (CIN1, CIN2).
Among patients with CIN2, nearly all of those treated with the highest dose of HAL and photodynamic therapy had a response at 3 months, compared with roughly half of their counterparts treated with placebo.
The therapy was associated with a higher rate of local reactions, but none had to discontinue treatment.
"The 5% HAL photodynamic therapy was effective in treating patients with CIN2. There seems to be a signal of efficacy in patients who have HPV 16 and 18 as well," which may help inform the design of future phase III trials, commented Dr. Einstein, who is director of clinical research for women’s health and gynecologic oncology at the Montefiore Medical Center, New York.
"This device was very easy to use and was very well tolerated by this patient population, with essentially self-limiting reactions," he added.
Dr. Einstein noted that new approaches are needed for dealing with CIN, given that it commonly occurs in young women of childbearing age, and that some current treatments aimed at obliterating these lesions make subsequent colposcopies difficult and increase the risk of preterm birth.
For photodynamic therapy, a photosensitizing agent is applied to the cervix and accumulates in the premalignant cells, he explained. When the area is illuminated at a specific energy, reactive oxygen species are generated, killing the cells.
"The hypothesized mechanism of photodynamic therapy in cervical lesions is that once the HAL is applied and light is emitted for about 5 hours, this induces some local apoptosis, and that will release a lot of HPV antigens from these dying cells. These are then presented to naive T cells in the locoregional lymph nodes, which then stimulates even more of a cell-mediated immune response and inflammatory response that then further increases apoptosis of local cells," Dr. Einstein elaborated. "And then, hypothetically, in other areas of the cervical and vaginal tract, you are going to get a big cell-mediated immune response."
Women in the trial, which was sponsored by Photocure, had pathologically confirmed, previously untreated CIN1 or CIN2.
They were randomized evenly to four groups treated with HAL 5%, 1%, or 0.2%, or placebo, and photodynamic therapy.
A gynecologist placed the integrated drug and device (Cevira, manufactured by Photocure) in the outpatient setting. Five hours after placement, the device self-activated and delivered photodynamic therapy for roughly 5 hours. The patients removed the device themselves thereafter.
The patients had a median age of 27 years, and 46% had CIN2. About half of those tested were found to have a high-risk type of HPV.
Among patients with CIN2, 5% HAL photodynamic therapy yielded a higher 3-month rate of response (based on histology, cytology, and HPV status) than did placebo, both overall (95% vs. 56%; P = .01) and in the subset who were positive for any type of HPV (92% vs. 50%; P = .02).
"Clearly, the placebo effect was very large in this group, and this is expected in young women who have CIN1 and CIN2. That being said, this was significant efficacy when compared to placebo," said Dr. Einstein, who disclosed that his institution has received funding from Photocure for educational speaking activities and research.
Additionally, among the patients with CIN2 who had HPV 16 or 18 infection, those treated with 5% HAL photodynamic therapy were more likely than were those treated with placebo to have clearance of the virus (83% vs. 0%; P = .02).
There was no significant benefit among women with CIN1 or among women treated with the lower doses of HAL.
Relative to their counterparts treated with placebo, patients treated with 5% HAL photodynamic therapy had a higher rate of self-limiting local reactions (54% vs. 32%); the most common were vaginal discharge and local discomfort. None of the patients discontinued treatment because of these reactions.
A total of five pregnancies were reported among study patients in the 3 months after treatment. All of these women delivered normal full-term infants.
LOS ANGELES – An investigational type of photodynamic therapy appears promising for treating early cervical intraepithelial neoplasia, finds a phase 2b trial reported at the annual meeting of the Society of Gynecologic Oncology.
A team led by Dr. Mark H. Einstein undertook a dose-finding study of hexaminolevulinate (HAL) gel coupled with photodynamic therapy in 262 patients with grade 1 or 2 cervical intraepithelial neoplasia (CIN1, CIN2).
Among patients with CIN2, nearly all of those treated with the highest dose of HAL and photodynamic therapy had a response at 3 months, compared with roughly half of their counterparts treated with placebo.
The therapy was associated with a higher rate of local reactions, but none had to discontinue treatment.
"The 5% HAL photodynamic therapy was effective in treating patients with CIN2. There seems to be a signal of efficacy in patients who have HPV 16 and 18 as well," which may help inform the design of future phase III trials, commented Dr. Einstein, who is director of clinical research for women’s health and gynecologic oncology at the Montefiore Medical Center, New York.
"This device was very easy to use and was very well tolerated by this patient population, with essentially self-limiting reactions," he added.
Dr. Einstein noted that new approaches are needed for dealing with CIN, given that it commonly occurs in young women of childbearing age, and that some current treatments aimed at obliterating these lesions make subsequent colposcopies difficult and increase the risk of preterm birth.
For photodynamic therapy, a photosensitizing agent is applied to the cervix and accumulates in the premalignant cells, he explained. When the area is illuminated at a specific energy, reactive oxygen species are generated, killing the cells.
"The hypothesized mechanism of photodynamic therapy in cervical lesions is that once the HAL is applied and light is emitted for about 5 hours, this induces some local apoptosis, and that will release a lot of HPV antigens from these dying cells. These are then presented to naive T cells in the locoregional lymph nodes, which then stimulates even more of a cell-mediated immune response and inflammatory response that then further increases apoptosis of local cells," Dr. Einstein elaborated. "And then, hypothetically, in other areas of the cervical and vaginal tract, you are going to get a big cell-mediated immune response."
Women in the trial, which was sponsored by Photocure, had pathologically confirmed, previously untreated CIN1 or CIN2.
They were randomized evenly to four groups treated with HAL 5%, 1%, or 0.2%, or placebo, and photodynamic therapy.
A gynecologist placed the integrated drug and device (Cevira, manufactured by Photocure) in the outpatient setting. Five hours after placement, the device self-activated and delivered photodynamic therapy for roughly 5 hours. The patients removed the device themselves thereafter.
The patients had a median age of 27 years, and 46% had CIN2. About half of those tested were found to have a high-risk type of HPV.
Among patients with CIN2, 5% HAL photodynamic therapy yielded a higher 3-month rate of response (based on histology, cytology, and HPV status) than did placebo, both overall (95% vs. 56%; P = .01) and in the subset who were positive for any type of HPV (92% vs. 50%; P = .02).
"Clearly, the placebo effect was very large in this group, and this is expected in young women who have CIN1 and CIN2. That being said, this was significant efficacy when compared to placebo," said Dr. Einstein, who disclosed that his institution has received funding from Photocure for educational speaking activities and research.
Additionally, among the patients with CIN2 who had HPV 16 or 18 infection, those treated with 5% HAL photodynamic therapy were more likely than were those treated with placebo to have clearance of the virus (83% vs. 0%; P = .02).
There was no significant benefit among women with CIN1 or among women treated with the lower doses of HAL.
Relative to their counterparts treated with placebo, patients treated with 5% HAL photodynamic therapy had a higher rate of self-limiting local reactions (54% vs. 32%); the most common were vaginal discharge and local discomfort. None of the patients discontinued treatment because of these reactions.
A total of five pregnancies were reported among study patients in the 3 months after treatment. All of these women delivered normal full-term infants.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: Patients with CIN2 were significantly more likely to have a response when treated with the highest dose of HAL photodynamic therapy than when treated with placebo (95% vs. 56%).
Data source: A randomized double-blind phase 2b trial of HAL photodynamic therapy in 262 patients with CIN1 or CIN2
Disclosures: Dr. Einstein disclosed that his institution has received funding from Photocure for educational speaking activities and research. The trial was sponsored by Photocure.
Retroperitoneal exploration extends survival in stage IIIc ovarian cancer
LOS ANGELES – Surgically exploring the retroperitoneum for disease may benefit some patients undergoing primary debulking of advanced ovarian cancer, a study reported at the annual meeting of the Society of Gynecologic Oncology has shown.
Investigators analyzed data from Gynecologic Oncology Group (GOG) trial 182, focusing on the 1,876 women who had stage IIIc epithelial ovarian cancer on the basis of intraperitoneal tumor size and who underwent optimal debulking.
Overall, one-third had a retroperitoneal exploration, defined in the study as removal of at least one pelvic or para-aortic lymph node.
Patients who had this procedure were 15% less likely to experience progression or death and 15% less likely to die after other factors were considered, reported lead investigator Dr. Bunja Rungruang, a gynecologic oncologist with Georgia Regents University in Augusta.
In stratified analyses, benefit was seen in the subgroup with minimal gross residual disease but not in the subgroup with microscopic residual disease.
"In this large multi-institutional trial, there is evidence that retroperitoneal exploration at the time of primary debulking surgery of patients with intraperitoneal stage IIIc epithelial ovarian cancer may provide survival benefit," she commented.
"Surgical effort and tumor biology interact to affect patient outcomes," Dr. Rungruang noted. "Retroperitoneal exploration may be a proxy for more thorough surgical effort in these patients, rather than tumor biology alone driving outcomes. Surgeon discretion is a potential factor here as well; it is conceivable that the surgeon’s impression or information about prognosis influences the retroperitoneal exploration decision, based on unmeasured indicators of patient disease burden or vitality.
"Given the small but significant survival differences and the large sample size of this study, it is possible that these survival advantages are to some degree indicative of unmeasured factors or the accuracy of the surgeon’s impression, and not completely about the act of pathologic exploration," she said.
One attendee noted that analyses have suggested that patients who do not have a retroperitoneal exploration fare even more poorly than those who have the procedure and are found to have positive lymph nodes.
"I am concerned that that is because the surgeon thought the prognosis was so bad that they didn’t bother. I don’t know whether you have a sense of whether that conclusion looked appropriate for your analysis of all the tumor burden in that patient," Dr. Rungruang said.
"For some of the patients, it seemed to be a surgeon preference that they didn’t sample the nodes because they felt that the patient was already stage IIIc and called them microscopic optimally debulked, or microscopic optimally debulked without assessing the lymph nodes. Other patients had a much larger surgery, a higher complexity of procedures, and still had a lymph node assessment on top of it. What I can tell from reading the actual operative notes is a lot of [the approach] is based on surgeon preference."
In discussing the lack of additional benefit for exploration in women with microscopic residual disease, Dr. Rungruang explained that "if you have microscopic residual disease, that seems like the best you can do for those patients. I think in the macroscopic residual patients, you see the difference because it is perhaps a proxy for just a more thorough surgical assessment in these patients. Plus, macroscopic residual disease is such a wide spectrum, you can be anywhere from one site of residual disease to miliary disease spread throughout, and that heterogeneity within that residual disease group also accounts for that difference."
Patients enrolled in GOG 182 had advanced epithelial ovarian cancer, primary peritoneal cancer, or fallopian tube cancer, and underwent primary debulking to optimal residual disease (less than 1 cm), followed by randomization to a variety of platinum- and paclitaxel-based adjuvant chemotherapy regimens.
The investigators restricted analyses to the subset whose disease was stage IIIc on the basis of an intraperitoneal tumor measuring at least 2 cm. Overall, 37% of this subset had a retroperitoneal exploration.
The patients undergoing this additional procedure had better median progression-free survival (18.5 vs. 16.0 months, P less than .0001) and overall survival (53.3 vs. 42.8 months, P less than .0001), reported Dr. Rungruang.
When patients were stratified, retroperitoneal exploration was beneficial in those with minimal gross residual disease in terms of both progression-free survival (16.8 vs. 15.1 months, P = .01) and overall survival (44.9 vs. 40.5 months, P = .008). But there was no such benefit in patients who had microscopic residual disease.
In a multivariate analysis, retroperitoneal exploration independently predicted better progression-free survival (hazard ratio, 0.85; P = .004) and overall survival (HR, 0.85; P = .009).
Dr. Rungruang disclosed no relevant financial conflicts.
LOS ANGELES – Surgically exploring the retroperitoneum for disease may benefit some patients undergoing primary debulking of advanced ovarian cancer, a study reported at the annual meeting of the Society of Gynecologic Oncology has shown.
Investigators analyzed data from Gynecologic Oncology Group (GOG) trial 182, focusing on the 1,876 women who had stage IIIc epithelial ovarian cancer on the basis of intraperitoneal tumor size and who underwent optimal debulking.
Overall, one-third had a retroperitoneal exploration, defined in the study as removal of at least one pelvic or para-aortic lymph node.
Patients who had this procedure were 15% less likely to experience progression or death and 15% less likely to die after other factors were considered, reported lead investigator Dr. Bunja Rungruang, a gynecologic oncologist with Georgia Regents University in Augusta.
In stratified analyses, benefit was seen in the subgroup with minimal gross residual disease but not in the subgroup with microscopic residual disease.
"In this large multi-institutional trial, there is evidence that retroperitoneal exploration at the time of primary debulking surgery of patients with intraperitoneal stage IIIc epithelial ovarian cancer may provide survival benefit," she commented.
"Surgical effort and tumor biology interact to affect patient outcomes," Dr. Rungruang noted. "Retroperitoneal exploration may be a proxy for more thorough surgical effort in these patients, rather than tumor biology alone driving outcomes. Surgeon discretion is a potential factor here as well; it is conceivable that the surgeon’s impression or information about prognosis influences the retroperitoneal exploration decision, based on unmeasured indicators of patient disease burden or vitality.
"Given the small but significant survival differences and the large sample size of this study, it is possible that these survival advantages are to some degree indicative of unmeasured factors or the accuracy of the surgeon’s impression, and not completely about the act of pathologic exploration," she said.
One attendee noted that analyses have suggested that patients who do not have a retroperitoneal exploration fare even more poorly than those who have the procedure and are found to have positive lymph nodes.
"I am concerned that that is because the surgeon thought the prognosis was so bad that they didn’t bother. I don’t know whether you have a sense of whether that conclusion looked appropriate for your analysis of all the tumor burden in that patient," Dr. Rungruang said.
"For some of the patients, it seemed to be a surgeon preference that they didn’t sample the nodes because they felt that the patient was already stage IIIc and called them microscopic optimally debulked, or microscopic optimally debulked without assessing the lymph nodes. Other patients had a much larger surgery, a higher complexity of procedures, and still had a lymph node assessment on top of it. What I can tell from reading the actual operative notes is a lot of [the approach] is based on surgeon preference."
In discussing the lack of additional benefit for exploration in women with microscopic residual disease, Dr. Rungruang explained that "if you have microscopic residual disease, that seems like the best you can do for those patients. I think in the macroscopic residual patients, you see the difference because it is perhaps a proxy for just a more thorough surgical assessment in these patients. Plus, macroscopic residual disease is such a wide spectrum, you can be anywhere from one site of residual disease to miliary disease spread throughout, and that heterogeneity within that residual disease group also accounts for that difference."
Patients enrolled in GOG 182 had advanced epithelial ovarian cancer, primary peritoneal cancer, or fallopian tube cancer, and underwent primary debulking to optimal residual disease (less than 1 cm), followed by randomization to a variety of platinum- and paclitaxel-based adjuvant chemotherapy regimens.
The investigators restricted analyses to the subset whose disease was stage IIIc on the basis of an intraperitoneal tumor measuring at least 2 cm. Overall, 37% of this subset had a retroperitoneal exploration.
The patients undergoing this additional procedure had better median progression-free survival (18.5 vs. 16.0 months, P less than .0001) and overall survival (53.3 vs. 42.8 months, P less than .0001), reported Dr. Rungruang.
When patients were stratified, retroperitoneal exploration was beneficial in those with minimal gross residual disease in terms of both progression-free survival (16.8 vs. 15.1 months, P = .01) and overall survival (44.9 vs. 40.5 months, P = .008). But there was no such benefit in patients who had microscopic residual disease.
In a multivariate analysis, retroperitoneal exploration independently predicted better progression-free survival (hazard ratio, 0.85; P = .004) and overall survival (HR, 0.85; P = .009).
Dr. Rungruang disclosed no relevant financial conflicts.
LOS ANGELES – Surgically exploring the retroperitoneum for disease may benefit some patients undergoing primary debulking of advanced ovarian cancer, a study reported at the annual meeting of the Society of Gynecologic Oncology has shown.
Investigators analyzed data from Gynecologic Oncology Group (GOG) trial 182, focusing on the 1,876 women who had stage IIIc epithelial ovarian cancer on the basis of intraperitoneal tumor size and who underwent optimal debulking.
Overall, one-third had a retroperitoneal exploration, defined in the study as removal of at least one pelvic or para-aortic lymph node.
Patients who had this procedure were 15% less likely to experience progression or death and 15% less likely to die after other factors were considered, reported lead investigator Dr. Bunja Rungruang, a gynecologic oncologist with Georgia Regents University in Augusta.
In stratified analyses, benefit was seen in the subgroup with minimal gross residual disease but not in the subgroup with microscopic residual disease.
"In this large multi-institutional trial, there is evidence that retroperitoneal exploration at the time of primary debulking surgery of patients with intraperitoneal stage IIIc epithelial ovarian cancer may provide survival benefit," she commented.
"Surgical effort and tumor biology interact to affect patient outcomes," Dr. Rungruang noted. "Retroperitoneal exploration may be a proxy for more thorough surgical effort in these patients, rather than tumor biology alone driving outcomes. Surgeon discretion is a potential factor here as well; it is conceivable that the surgeon’s impression or information about prognosis influences the retroperitoneal exploration decision, based on unmeasured indicators of patient disease burden or vitality.
"Given the small but significant survival differences and the large sample size of this study, it is possible that these survival advantages are to some degree indicative of unmeasured factors or the accuracy of the surgeon’s impression, and not completely about the act of pathologic exploration," she said.
One attendee noted that analyses have suggested that patients who do not have a retroperitoneal exploration fare even more poorly than those who have the procedure and are found to have positive lymph nodes.
"I am concerned that that is because the surgeon thought the prognosis was so bad that they didn’t bother. I don’t know whether you have a sense of whether that conclusion looked appropriate for your analysis of all the tumor burden in that patient," Dr. Rungruang said.
"For some of the patients, it seemed to be a surgeon preference that they didn’t sample the nodes because they felt that the patient was already stage IIIc and called them microscopic optimally debulked, or microscopic optimally debulked without assessing the lymph nodes. Other patients had a much larger surgery, a higher complexity of procedures, and still had a lymph node assessment on top of it. What I can tell from reading the actual operative notes is a lot of [the approach] is based on surgeon preference."
In discussing the lack of additional benefit for exploration in women with microscopic residual disease, Dr. Rungruang explained that "if you have microscopic residual disease, that seems like the best you can do for those patients. I think in the macroscopic residual patients, you see the difference because it is perhaps a proxy for just a more thorough surgical assessment in these patients. Plus, macroscopic residual disease is such a wide spectrum, you can be anywhere from one site of residual disease to miliary disease spread throughout, and that heterogeneity within that residual disease group also accounts for that difference."
Patients enrolled in GOG 182 had advanced epithelial ovarian cancer, primary peritoneal cancer, or fallopian tube cancer, and underwent primary debulking to optimal residual disease (less than 1 cm), followed by randomization to a variety of platinum- and paclitaxel-based adjuvant chemotherapy regimens.
The investigators restricted analyses to the subset whose disease was stage IIIc on the basis of an intraperitoneal tumor measuring at least 2 cm. Overall, 37% of this subset had a retroperitoneal exploration.
The patients undergoing this additional procedure had better median progression-free survival (18.5 vs. 16.0 months, P less than .0001) and overall survival (53.3 vs. 42.8 months, P less than .0001), reported Dr. Rungruang.
When patients were stratified, retroperitoneal exploration was beneficial in those with minimal gross residual disease in terms of both progression-free survival (16.8 vs. 15.1 months, P = .01) and overall survival (44.9 vs. 40.5 months, P = .008). But there was no such benefit in patients who had microscopic residual disease.
In a multivariate analysis, retroperitoneal exploration independently predicted better progression-free survival (hazard ratio, 0.85; P = .004) and overall survival (HR, 0.85; P = .009).
Dr. Rungruang disclosed no relevant financial conflicts.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: Median progression-free survival was better (18.5 vs. 16.0 months, P less than .0001) and overall survival was longer (53.3 vs. 42.8 months, P less than .0001) in patients who had a retroperitoneal exploration.
Data source: A subset analysis of GOG 182 focusing on 1,876 women who had stage IIIc epithelial ovarian cancer and underwent optimal debulking.
Disclosures: Dr. Rungruang disclosed no relevant financial conflicts.
CA125 level predicts microscopic residual disease in ovarian cancer
LOS ANGELES – Preoperative levels of cancer antigen 125 (CA125) predict surgical and disease outcomes in women with advanced epithelial ovarian cancer who are able to undergo optimal debulking surgery, new data show, and may therefore help guide treatment decisions.
A team led by Dr. Neil S. Horowitz of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston assessed levels of the biomarker among nearly 1,000 women who had stage III or IV disease that was optimally debulked to less than 1 cm of residual disease and who received adjuvant paclitaxel- and platinum-containing chemotherapy.
Results showed that no cutoff value of preoperative CA125 levels clearly separated women in whom microscopic residual disease was achieved surgically from women in whom a greater volume of disease remained, he reported at the annual meeting of the Society of Gynecologic Oncology.
But the probability of achieving microscopic status decreased with increasing CA125 levels. For example, it fell from 33% in women with a level of 500 U/mL to 27% in women with a level of 1,000 U/mL.
"Although a strict CA125 value to predict microscopic residual cannot be made, these data are helpful for counseling patients regarding surgical results and outcome, and should influence decisions regarding primary debulking surgery and possibly use of other ... treatment options like neoadjuvant chemotherapy," Dr. Horowitz said. "Each surgeon and [his or her] patient have to decide for themselves what is an acceptable probability of successful surgical outcome to microscopic residual disease.
Additional study findings showed that women with higher preoperative CA125 levels and women with smaller reductions in CA125 levels between the preoperative period and the pretreatment period, before starting chemotherapy, had significantly worse progression-free and overall survival.
One session attendee asked, "What impact do you think surgical expertise has on the ability to predict the extent of cytoreduction?"
"Most trained gyn oncologists have the ability and training to take somebody to microscopic residual disease. What it takes to get to that place obviously varies from patient to patient and the disease that they have at the time that they present. Ultimately, what has to be decided between the patient and the physician is what’s going to be the best possibility for them and using CA125 as a potential guide, say, taking everything into consideration – age, where their disease is, what their CA125 is, what my comfort level is doing certain procedures being able to get them down to microscopic disease," Dr. Horowitz replied. "So I don’t think it’s a one-size-fits-all [objective] based just on the surgical expertise. Most gyn oncologists are trained adequately to be able to do this. It’s just, because you can do it, the question is, should you be doing it on everybody."
Another attendee said, "In follow-up to that, do you think that the difference in the behavior of the presurgical and the pretreatment CA125 could be confounded, the latter by surgical decisions or surgical intervention?"
"It’s potentially confounded; whether it’s surgical skill or some people would say, I don’t want to use the term honesty, but it may be a reflection of what truly is left behind versus not left behind, if it didn’t really follow the way it should. It may be a window into how accurate our predictions or our estimates of what we left behind really are," Dr. Horowitz explained. "Pretreatment CA125, it is difficult to really get a good understanding of this number because obviously the patients who start with the highest CA125 have the greatest chance to fall ... So it’s a little tricky trying to figure out what to make of that number, whereas patients who start with a lower one, although they didn’t fall with the same percentile, you still may have done just as good a job surgically."
The 998 women studied were from Gynecologic Oncology Group (GOG) trial 182. "This is the largest reported series to evaluate the ability of preoperative CA125 to predict surgical cytoreductive outcomes and survival in a population of women with optimally cytoreduced primary ovarian or peritoneal cancer," Dr. Horowitz noted.
Overall, 33% had microscopic residual disease, while the other 67% had more extensive residual disease but still measuring less than 1 cm.
The median preoperative CA125 level was 346 U/mL in the former group and 870 U/mL in the latter, reported Dr. Horowitz, who disclosed no conflicts of interest related to the research.
"Despite the difference in median preoperative CA125 values, the distributions of the preoperative CA125s in those with microscopic and less than 1 cm residual overlapped almost completely," Dr. Horowitz reported. "This suggests that there is not a preoperative CA125 beyond which one cannot achieve a complete cytoreductive surgery."
However, the higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease (P less than .01). For example, the probability was 33%, 27%, and 19% for women having a level of 500, 1,000, and 2,500 U/mL, respectively.
"It is important to remember that these curves only reflect data from women who achieved optimal cytoreduction and do not include those with suboptimal primary debulking. Therefore, the estimated predictions and probabilities are likely to decrease when applied to a preoperative population of unknown surgical outcome," he said. "But if one assumes a priori that you can achieve and will achieve optimal cytoreduction, then preoperative CA125 can estimate the likelihood of obtaining either microscopic or less than 1-cm residual."
In adjusted analyses, preoperative CA125 levels and extent of residual disease jointly predicted both progression-free survival (P less than .001) and overall survival (P = .04). For example, median overall survival ranged from 82 months in women having microscopic residual disease and a CA125 level of 35 U/mL to just 39 months in their counterparts with more residual disease and a CA125 level of 1,000 U/mL.
The change from preoperative to pretreatment CA125 levels predicted both progression-free survival (P less than .0001) and overall survival (P less than .0001). For example, median overall survival ranged from 60 months in women having a reduction in levels exceeding 80% to 45 months in their counterparts having stable or increasing levels.
In addition, among the group having a greater than 80% decline in CA125 level, survival was almost twice as long among those achieving microscopic residual disease, at 82 months, as among those with greater residual disease, at 48 months, "suggesting that residual disease rather than change in CA125 is more important to survival," Dr. Horowitz said.
LOS ANGELES – Preoperative levels of cancer antigen 125 (CA125) predict surgical and disease outcomes in women with advanced epithelial ovarian cancer who are able to undergo optimal debulking surgery, new data show, and may therefore help guide treatment decisions.
A team led by Dr. Neil S. Horowitz of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston assessed levels of the biomarker among nearly 1,000 women who had stage III or IV disease that was optimally debulked to less than 1 cm of residual disease and who received adjuvant paclitaxel- and platinum-containing chemotherapy.
Results showed that no cutoff value of preoperative CA125 levels clearly separated women in whom microscopic residual disease was achieved surgically from women in whom a greater volume of disease remained, he reported at the annual meeting of the Society of Gynecologic Oncology.
But the probability of achieving microscopic status decreased with increasing CA125 levels. For example, it fell from 33% in women with a level of 500 U/mL to 27% in women with a level of 1,000 U/mL.
"Although a strict CA125 value to predict microscopic residual cannot be made, these data are helpful for counseling patients regarding surgical results and outcome, and should influence decisions regarding primary debulking surgery and possibly use of other ... treatment options like neoadjuvant chemotherapy," Dr. Horowitz said. "Each surgeon and [his or her] patient have to decide for themselves what is an acceptable probability of successful surgical outcome to microscopic residual disease.
Additional study findings showed that women with higher preoperative CA125 levels and women with smaller reductions in CA125 levels between the preoperative period and the pretreatment period, before starting chemotherapy, had significantly worse progression-free and overall survival.
One session attendee asked, "What impact do you think surgical expertise has on the ability to predict the extent of cytoreduction?"
"Most trained gyn oncologists have the ability and training to take somebody to microscopic residual disease. What it takes to get to that place obviously varies from patient to patient and the disease that they have at the time that they present. Ultimately, what has to be decided between the patient and the physician is what’s going to be the best possibility for them and using CA125 as a potential guide, say, taking everything into consideration – age, where their disease is, what their CA125 is, what my comfort level is doing certain procedures being able to get them down to microscopic disease," Dr. Horowitz replied. "So I don’t think it’s a one-size-fits-all [objective] based just on the surgical expertise. Most gyn oncologists are trained adequately to be able to do this. It’s just, because you can do it, the question is, should you be doing it on everybody."
Another attendee said, "In follow-up to that, do you think that the difference in the behavior of the presurgical and the pretreatment CA125 could be confounded, the latter by surgical decisions or surgical intervention?"
"It’s potentially confounded; whether it’s surgical skill or some people would say, I don’t want to use the term honesty, but it may be a reflection of what truly is left behind versus not left behind, if it didn’t really follow the way it should. It may be a window into how accurate our predictions or our estimates of what we left behind really are," Dr. Horowitz explained. "Pretreatment CA125, it is difficult to really get a good understanding of this number because obviously the patients who start with the highest CA125 have the greatest chance to fall ... So it’s a little tricky trying to figure out what to make of that number, whereas patients who start with a lower one, although they didn’t fall with the same percentile, you still may have done just as good a job surgically."
The 998 women studied were from Gynecologic Oncology Group (GOG) trial 182. "This is the largest reported series to evaluate the ability of preoperative CA125 to predict surgical cytoreductive outcomes and survival in a population of women with optimally cytoreduced primary ovarian or peritoneal cancer," Dr. Horowitz noted.
Overall, 33% had microscopic residual disease, while the other 67% had more extensive residual disease but still measuring less than 1 cm.
The median preoperative CA125 level was 346 U/mL in the former group and 870 U/mL in the latter, reported Dr. Horowitz, who disclosed no conflicts of interest related to the research.
"Despite the difference in median preoperative CA125 values, the distributions of the preoperative CA125s in those with microscopic and less than 1 cm residual overlapped almost completely," Dr. Horowitz reported. "This suggests that there is not a preoperative CA125 beyond which one cannot achieve a complete cytoreductive surgery."
However, the higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease (P less than .01). For example, the probability was 33%, 27%, and 19% for women having a level of 500, 1,000, and 2,500 U/mL, respectively.
"It is important to remember that these curves only reflect data from women who achieved optimal cytoreduction and do not include those with suboptimal primary debulking. Therefore, the estimated predictions and probabilities are likely to decrease when applied to a preoperative population of unknown surgical outcome," he said. "But if one assumes a priori that you can achieve and will achieve optimal cytoreduction, then preoperative CA125 can estimate the likelihood of obtaining either microscopic or less than 1-cm residual."
In adjusted analyses, preoperative CA125 levels and extent of residual disease jointly predicted both progression-free survival (P less than .001) and overall survival (P = .04). For example, median overall survival ranged from 82 months in women having microscopic residual disease and a CA125 level of 35 U/mL to just 39 months in their counterparts with more residual disease and a CA125 level of 1,000 U/mL.
The change from preoperative to pretreatment CA125 levels predicted both progression-free survival (P less than .0001) and overall survival (P less than .0001). For example, median overall survival ranged from 60 months in women having a reduction in levels exceeding 80% to 45 months in their counterparts having stable or increasing levels.
In addition, among the group having a greater than 80% decline in CA125 level, survival was almost twice as long among those achieving microscopic residual disease, at 82 months, as among those with greater residual disease, at 48 months, "suggesting that residual disease rather than change in CA125 is more important to survival," Dr. Horowitz said.
LOS ANGELES – Preoperative levels of cancer antigen 125 (CA125) predict surgical and disease outcomes in women with advanced epithelial ovarian cancer who are able to undergo optimal debulking surgery, new data show, and may therefore help guide treatment decisions.
A team led by Dr. Neil S. Horowitz of Brigham and Women’s Hospital and the Dana Farber Cancer Institute in Boston assessed levels of the biomarker among nearly 1,000 women who had stage III or IV disease that was optimally debulked to less than 1 cm of residual disease and who received adjuvant paclitaxel- and platinum-containing chemotherapy.
Results showed that no cutoff value of preoperative CA125 levels clearly separated women in whom microscopic residual disease was achieved surgically from women in whom a greater volume of disease remained, he reported at the annual meeting of the Society of Gynecologic Oncology.
But the probability of achieving microscopic status decreased with increasing CA125 levels. For example, it fell from 33% in women with a level of 500 U/mL to 27% in women with a level of 1,000 U/mL.
"Although a strict CA125 value to predict microscopic residual cannot be made, these data are helpful for counseling patients regarding surgical results and outcome, and should influence decisions regarding primary debulking surgery and possibly use of other ... treatment options like neoadjuvant chemotherapy," Dr. Horowitz said. "Each surgeon and [his or her] patient have to decide for themselves what is an acceptable probability of successful surgical outcome to microscopic residual disease.
Additional study findings showed that women with higher preoperative CA125 levels and women with smaller reductions in CA125 levels between the preoperative period and the pretreatment period, before starting chemotherapy, had significantly worse progression-free and overall survival.
One session attendee asked, "What impact do you think surgical expertise has on the ability to predict the extent of cytoreduction?"
"Most trained gyn oncologists have the ability and training to take somebody to microscopic residual disease. What it takes to get to that place obviously varies from patient to patient and the disease that they have at the time that they present. Ultimately, what has to be decided between the patient and the physician is what’s going to be the best possibility for them and using CA125 as a potential guide, say, taking everything into consideration – age, where their disease is, what their CA125 is, what my comfort level is doing certain procedures being able to get them down to microscopic disease," Dr. Horowitz replied. "So I don’t think it’s a one-size-fits-all [objective] based just on the surgical expertise. Most gyn oncologists are trained adequately to be able to do this. It’s just, because you can do it, the question is, should you be doing it on everybody."
Another attendee said, "In follow-up to that, do you think that the difference in the behavior of the presurgical and the pretreatment CA125 could be confounded, the latter by surgical decisions or surgical intervention?"
"It’s potentially confounded; whether it’s surgical skill or some people would say, I don’t want to use the term honesty, but it may be a reflection of what truly is left behind versus not left behind, if it didn’t really follow the way it should. It may be a window into how accurate our predictions or our estimates of what we left behind really are," Dr. Horowitz explained. "Pretreatment CA125, it is difficult to really get a good understanding of this number because obviously the patients who start with the highest CA125 have the greatest chance to fall ... So it’s a little tricky trying to figure out what to make of that number, whereas patients who start with a lower one, although they didn’t fall with the same percentile, you still may have done just as good a job surgically."
The 998 women studied were from Gynecologic Oncology Group (GOG) trial 182. "This is the largest reported series to evaluate the ability of preoperative CA125 to predict surgical cytoreductive outcomes and survival in a population of women with optimally cytoreduced primary ovarian or peritoneal cancer," Dr. Horowitz noted.
Overall, 33% had microscopic residual disease, while the other 67% had more extensive residual disease but still measuring less than 1 cm.
The median preoperative CA125 level was 346 U/mL in the former group and 870 U/mL in the latter, reported Dr. Horowitz, who disclosed no conflicts of interest related to the research.
"Despite the difference in median preoperative CA125 values, the distributions of the preoperative CA125s in those with microscopic and less than 1 cm residual overlapped almost completely," Dr. Horowitz reported. "This suggests that there is not a preoperative CA125 beyond which one cannot achieve a complete cytoreductive surgery."
However, the higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease (P less than .01). For example, the probability was 33%, 27%, and 19% for women having a level of 500, 1,000, and 2,500 U/mL, respectively.
"It is important to remember that these curves only reflect data from women who achieved optimal cytoreduction and do not include those with suboptimal primary debulking. Therefore, the estimated predictions and probabilities are likely to decrease when applied to a preoperative population of unknown surgical outcome," he said. "But if one assumes a priori that you can achieve and will achieve optimal cytoreduction, then preoperative CA125 can estimate the likelihood of obtaining either microscopic or less than 1-cm residual."
In adjusted analyses, preoperative CA125 levels and extent of residual disease jointly predicted both progression-free survival (P less than .001) and overall survival (P = .04). For example, median overall survival ranged from 82 months in women having microscopic residual disease and a CA125 level of 35 U/mL to just 39 months in their counterparts with more residual disease and a CA125 level of 1,000 U/mL.
The change from preoperative to pretreatment CA125 levels predicted both progression-free survival (P less than .0001) and overall survival (P less than .0001). For example, median overall survival ranged from 60 months in women having a reduction in levels exceeding 80% to 45 months in their counterparts having stable or increasing levels.
In addition, among the group having a greater than 80% decline in CA125 level, survival was almost twice as long among those achieving microscopic residual disease, at 82 months, as among those with greater residual disease, at 48 months, "suggesting that residual disease rather than change in CA125 is more important to survival," Dr. Horowitz said.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: The higher the preoperative CA125 level, the lower the predicted probability of achieving microscopic residual disease. Probability was 33%, 27%, and 19% for levels of 500, 1,000, and 2,500 U/mL, respectively.
Data source: An ancillary study among 998 women with optimally debulked advanced epithelial ovarian cancer or primary peritoneal cancer from the GOG 182 trial.
Disclosures: Dr. Horowitz disclosed no relevant conflicts of interest.
Cyberknife therapy offers benefits for recurring gyn cancers
LOS ANGELES – Robotic Cyberknife radiation therapy will likely expand the treatment options for patients whose gynecologic malignancies recur, researchers reported at the annual meeting of the Society of Gynecologic Oncologists.
A total of 50 patients with recurrent gynecologic (mainly ovarian and endometrial) cancers underwent Cyberknife treatment, which allows targeting of high doses of radiation to the tumor while largely sparing adjacent healthy tissue. In this case, patients received an 8-Gy treatment on each of 3 consecutive days.
Results showed that two-thirds of the patients had a complete response, a partial response, or stable disease 6 months after treatment. Higher-severity acute adverse events were uncommon and consisted of single cases of diarrhea and hyperbilirubinemia.
"This is the first phase II clinical trial of robotic radiosurgery in the gynecologic oncology space. Robotic Cyberknife radiation therapy does definitely provide clinical benefit to your patients," commented lead author Dr. Charles Kunos, a radiation oncologist with the Case Comprehensive Cancer Center in Cleveland and the Summa Cancer Institute in Akron, Ohio.
However, the majority of women ultimately had progression in nontargeted areas of disease, and this progression was the cause of death in 40%. Therefore, the investigators have initiated a phase I trial combining Cyberknife therapy with systemic chemotherapy.
One attendee noted, "As I think we all know, many of these patients who have recurrent side-wall disease from gynecologic cancers have a loop of bowel that’s sitting immediately adjacent to the potential target. And we have always felt that you needed to adjust the dose per fraction depending on that in patients with recurrent disease who have been previously irradiated. How do you select your patients for these 8-Gy-fraction treatments?"
"Patient selection is mostly based on target volume and the number of sites that are going to be treated during the course of therapy. ... We find that the 8-Gy dose is extremely well tolerated," he noted. The team is currently performing analyses to determine maximum tissue tolerances and optimally guide patient selection.
Another attendee had a similar question, asking whether any of the lesions treated were located in a previously irradiated field.
"More than 60% of those patients had received prior radiation therapy. Almost all the cervical cancer patients in the trial, as well as the majority of those patients with endometrial cancer, had received prior radiation therapy," Dr. Kunos replied. "The prior radiation therapy is not a barrier for delivering this form of treatment at these doses. Our toxicity rates are extraordinarily low, even in the cases with the prior radiation, so with selection of the patient who has a relatively good performing health status, as well as considering the time of when the previous radiation therapy dose was delivered, I think you can adequately select patients for this type of therapy."
A third attendee posed bigger-picture questions: "Can you tell us a little bit about the cost-effectiveness of the Cyberknife therapy and, given that you have an ongoing phase I trial looking at this in dual-modality [treatment] with chemotherapy, what is the future of this therapeutic approach for gyn malignancies?"
"The NCI [National Cancer Institute] is interested in exploring the radiosurgery platform as a way of testing novel therapeutics as radiation sensitizers, but because the radiation therapy is so exquisitely tuned to the actual cancer target, there is an opportunity to study whether or not there are systemic effects of the novel drugs as well. So I think at some level, the future is relatively bright," Dr. Kunos explained.
"Regarding the cost or the expense of therapy, we are condensing 5, 6, 7 weeks of radiation therapy into 3 days on the trial, so there are considerable savings in that regard to patient travel and other, social aspects of treatment in trying to get patients back and forth for several weeks of therapy in a palliative situation," he continued. "The radiosurgery itself is expensive; that part of the cost structure will probably continue to come down in the future with the way that patients will be managed."
The cohort enrolled in the trial included 25 patients with ovarian cancer, 14 with endometrial cancer, 9 with cervical cancer, and 2 with vulvar cancer. All had received at least one chemotherapy or radiation therapy regimen previously.
The patients had up to four targets of disease to be treated. They underwent implantation of gold seeds for target tracking during treatment, and co-registered computed tomography and positron emission tomography scans were used to generate the radiation therapy plan.
The patients received a total of 24 Gy of radiation delivered in three daily doses of 8 Gy each. The median duration of follow-up was 15 months.
Study results, reported at the meeting and recently published (Front. Oncol. 2012;2:181), showed that 3 months after treatment, 50% of patients had a complete response, 46% had a partial response, and 4% had stable disease, according to Dr. Kunos.
At 6 months, the rate of clinical benefit – capturing patients with a complete response, partial response, or stable disease – was 68%.
Ultimately, 62% of patients had progression in a nontargeted disease site, and 40% died from disease progression.
"Reversible fatigue lasting up to 1 week after treatment was the most noticeable toxicity," Dr. Kunos said. In the first 30 days after treatment, the most common adverse effects were grade 2 fatigue, seen in 16% of patients, and grade 2 nausea, seen in 8%. Only 2% of patients had grade 3 diarrhea, and only 2% had grade 4 hyperbilirubinemia.
Dr. Kunos disclosed that he had no relevant conflicts of interest.
LOS ANGELES – Robotic Cyberknife radiation therapy will likely expand the treatment options for patients whose gynecologic malignancies recur, researchers reported at the annual meeting of the Society of Gynecologic Oncologists.
A total of 50 patients with recurrent gynecologic (mainly ovarian and endometrial) cancers underwent Cyberknife treatment, which allows targeting of high doses of radiation to the tumor while largely sparing adjacent healthy tissue. In this case, patients received an 8-Gy treatment on each of 3 consecutive days.
Results showed that two-thirds of the patients had a complete response, a partial response, or stable disease 6 months after treatment. Higher-severity acute adverse events were uncommon and consisted of single cases of diarrhea and hyperbilirubinemia.
"This is the first phase II clinical trial of robotic radiosurgery in the gynecologic oncology space. Robotic Cyberknife radiation therapy does definitely provide clinical benefit to your patients," commented lead author Dr. Charles Kunos, a radiation oncologist with the Case Comprehensive Cancer Center in Cleveland and the Summa Cancer Institute in Akron, Ohio.
However, the majority of women ultimately had progression in nontargeted areas of disease, and this progression was the cause of death in 40%. Therefore, the investigators have initiated a phase I trial combining Cyberknife therapy with systemic chemotherapy.
One attendee noted, "As I think we all know, many of these patients who have recurrent side-wall disease from gynecologic cancers have a loop of bowel that’s sitting immediately adjacent to the potential target. And we have always felt that you needed to adjust the dose per fraction depending on that in patients with recurrent disease who have been previously irradiated. How do you select your patients for these 8-Gy-fraction treatments?"
"Patient selection is mostly based on target volume and the number of sites that are going to be treated during the course of therapy. ... We find that the 8-Gy dose is extremely well tolerated," he noted. The team is currently performing analyses to determine maximum tissue tolerances and optimally guide patient selection.
Another attendee had a similar question, asking whether any of the lesions treated were located in a previously irradiated field.
"More than 60% of those patients had received prior radiation therapy. Almost all the cervical cancer patients in the trial, as well as the majority of those patients with endometrial cancer, had received prior radiation therapy," Dr. Kunos replied. "The prior radiation therapy is not a barrier for delivering this form of treatment at these doses. Our toxicity rates are extraordinarily low, even in the cases with the prior radiation, so with selection of the patient who has a relatively good performing health status, as well as considering the time of when the previous radiation therapy dose was delivered, I think you can adequately select patients for this type of therapy."
A third attendee posed bigger-picture questions: "Can you tell us a little bit about the cost-effectiveness of the Cyberknife therapy and, given that you have an ongoing phase I trial looking at this in dual-modality [treatment] with chemotherapy, what is the future of this therapeutic approach for gyn malignancies?"
"The NCI [National Cancer Institute] is interested in exploring the radiosurgery platform as a way of testing novel therapeutics as radiation sensitizers, but because the radiation therapy is so exquisitely tuned to the actual cancer target, there is an opportunity to study whether or not there are systemic effects of the novel drugs as well. So I think at some level, the future is relatively bright," Dr. Kunos explained.
"Regarding the cost or the expense of therapy, we are condensing 5, 6, 7 weeks of radiation therapy into 3 days on the trial, so there are considerable savings in that regard to patient travel and other, social aspects of treatment in trying to get patients back and forth for several weeks of therapy in a palliative situation," he continued. "The radiosurgery itself is expensive; that part of the cost structure will probably continue to come down in the future with the way that patients will be managed."
The cohort enrolled in the trial included 25 patients with ovarian cancer, 14 with endometrial cancer, 9 with cervical cancer, and 2 with vulvar cancer. All had received at least one chemotherapy or radiation therapy regimen previously.
The patients had up to four targets of disease to be treated. They underwent implantation of gold seeds for target tracking during treatment, and co-registered computed tomography and positron emission tomography scans were used to generate the radiation therapy plan.
The patients received a total of 24 Gy of radiation delivered in three daily doses of 8 Gy each. The median duration of follow-up was 15 months.
Study results, reported at the meeting and recently published (Front. Oncol. 2012;2:181), showed that 3 months after treatment, 50% of patients had a complete response, 46% had a partial response, and 4% had stable disease, according to Dr. Kunos.
At 6 months, the rate of clinical benefit – capturing patients with a complete response, partial response, or stable disease – was 68%.
Ultimately, 62% of patients had progression in a nontargeted disease site, and 40% died from disease progression.
"Reversible fatigue lasting up to 1 week after treatment was the most noticeable toxicity," Dr. Kunos said. In the first 30 days after treatment, the most common adverse effects were grade 2 fatigue, seen in 16% of patients, and grade 2 nausea, seen in 8%. Only 2% of patients had grade 3 diarrhea, and only 2% had grade 4 hyperbilirubinemia.
Dr. Kunos disclosed that he had no relevant conflicts of interest.
LOS ANGELES – Robotic Cyberknife radiation therapy will likely expand the treatment options for patients whose gynecologic malignancies recur, researchers reported at the annual meeting of the Society of Gynecologic Oncologists.
A total of 50 patients with recurrent gynecologic (mainly ovarian and endometrial) cancers underwent Cyberknife treatment, which allows targeting of high doses of radiation to the tumor while largely sparing adjacent healthy tissue. In this case, patients received an 8-Gy treatment on each of 3 consecutive days.
Results showed that two-thirds of the patients had a complete response, a partial response, or stable disease 6 months after treatment. Higher-severity acute adverse events were uncommon and consisted of single cases of diarrhea and hyperbilirubinemia.
"This is the first phase II clinical trial of robotic radiosurgery in the gynecologic oncology space. Robotic Cyberknife radiation therapy does definitely provide clinical benefit to your patients," commented lead author Dr. Charles Kunos, a radiation oncologist with the Case Comprehensive Cancer Center in Cleveland and the Summa Cancer Institute in Akron, Ohio.
However, the majority of women ultimately had progression in nontargeted areas of disease, and this progression was the cause of death in 40%. Therefore, the investigators have initiated a phase I trial combining Cyberknife therapy with systemic chemotherapy.
One attendee noted, "As I think we all know, many of these patients who have recurrent side-wall disease from gynecologic cancers have a loop of bowel that’s sitting immediately adjacent to the potential target. And we have always felt that you needed to adjust the dose per fraction depending on that in patients with recurrent disease who have been previously irradiated. How do you select your patients for these 8-Gy-fraction treatments?"
"Patient selection is mostly based on target volume and the number of sites that are going to be treated during the course of therapy. ... We find that the 8-Gy dose is extremely well tolerated," he noted. The team is currently performing analyses to determine maximum tissue tolerances and optimally guide patient selection.
Another attendee had a similar question, asking whether any of the lesions treated were located in a previously irradiated field.
"More than 60% of those patients had received prior radiation therapy. Almost all the cervical cancer patients in the trial, as well as the majority of those patients with endometrial cancer, had received prior radiation therapy," Dr. Kunos replied. "The prior radiation therapy is not a barrier for delivering this form of treatment at these doses. Our toxicity rates are extraordinarily low, even in the cases with the prior radiation, so with selection of the patient who has a relatively good performing health status, as well as considering the time of when the previous radiation therapy dose was delivered, I think you can adequately select patients for this type of therapy."
A third attendee posed bigger-picture questions: "Can you tell us a little bit about the cost-effectiveness of the Cyberknife therapy and, given that you have an ongoing phase I trial looking at this in dual-modality [treatment] with chemotherapy, what is the future of this therapeutic approach for gyn malignancies?"
"The NCI [National Cancer Institute] is interested in exploring the radiosurgery platform as a way of testing novel therapeutics as radiation sensitizers, but because the radiation therapy is so exquisitely tuned to the actual cancer target, there is an opportunity to study whether or not there are systemic effects of the novel drugs as well. So I think at some level, the future is relatively bright," Dr. Kunos explained.
"Regarding the cost or the expense of therapy, we are condensing 5, 6, 7 weeks of radiation therapy into 3 days on the trial, so there are considerable savings in that regard to patient travel and other, social aspects of treatment in trying to get patients back and forth for several weeks of therapy in a palliative situation," he continued. "The radiosurgery itself is expensive; that part of the cost structure will probably continue to come down in the future with the way that patients will be managed."
The cohort enrolled in the trial included 25 patients with ovarian cancer, 14 with endometrial cancer, 9 with cervical cancer, and 2 with vulvar cancer. All had received at least one chemotherapy or radiation therapy regimen previously.
The patients had up to four targets of disease to be treated. They underwent implantation of gold seeds for target tracking during treatment, and co-registered computed tomography and positron emission tomography scans were used to generate the radiation therapy plan.
The patients received a total of 24 Gy of radiation delivered in three daily doses of 8 Gy each. The median duration of follow-up was 15 months.
Study results, reported at the meeting and recently published (Front. Oncol. 2012;2:181), showed that 3 months after treatment, 50% of patients had a complete response, 46% had a partial response, and 4% had stable disease, according to Dr. Kunos.
At 6 months, the rate of clinical benefit – capturing patients with a complete response, partial response, or stable disease – was 68%.
Ultimately, 62% of patients had progression in a nontargeted disease site, and 40% died from disease progression.
"Reversible fatigue lasting up to 1 week after treatment was the most noticeable toxicity," Dr. Kunos said. In the first 30 days after treatment, the most common adverse effects were grade 2 fatigue, seen in 16% of patients, and grade 2 nausea, seen in 8%. Only 2% of patients had grade 3 diarrhea, and only 2% had grade 4 hyperbilirubinemia.
Dr. Kunos disclosed that he had no relevant conflicts of interest.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: The 6-month clinical benefit rate was 68%. Higher-severity acute adverse events were uncommon.
Data source: A phase II trial among 50 patients with recurrent gynecologic cancers.
Disclosures: Dr. Kunos disclosed that he had no relevant conflicts of interest.
Racial genetic admixture linked to endometrial cancer outcomes
LOS ANGELES – Racial makeup based on genetic testing trumps self-reported race as a predictor of endometrial cancer outcomes, suggests the results of a study reported at the annual meeting of the Society of Gynecologic Oncology.
Researchers compared patient self reports of racial identity and the results of genotyping for markers of race in 217 women with endometrial cancer who had any-stage endometroid tumors.
The risk of cancer progression or death rose by 2% with each 1% increase in African racial genetic admixture and fell by 3% with each 1% increase in European racial genetic admixture.
"Racial genetic admixture significantly predicts the risk of recurrence and progression-free survival in endometrial cancer patients. Importantly, this risk is irrespective of self-designated race and could be used to stratify and identify patients’ recurrence risk," reported lead author Dr. Rodney P. Rocconi, a gynecologic oncologist at the Mitchell Cancer Institute and University of South Alabama in Mobile.
The results are worth examining as a key "to unraveling the etiology of this disparity, with the hopes of improving treatment outcomes and eventually eliminating this racial disparity in the future."
Dr. Rocconi acknowledged that the study included only endometroid tumors, and noted that black women typically have higher proportions of carcinosarcoma and type 2 endometrial cancers, a distinction that’s not always known preoperatively.
"In an ideal world, we would like to evaluate that (larger) population," Dr. Rocconi said. But "it came down to having enough funding to evaluate a population that is meaningful. In the future, by all means, it would be an extremely important population to look at."
African American women make up just 7% of all patients with endometrial cancer but account for 15% of deaths from the disease, he noted.
"To date, breaking down the definition of race in cancer racial disparity has largely been overlooked. Considering the majority of racial disparity research utilizes self-designated race, this in my opinion is the greatest limitation in this type of research. Self-designated race can be used as a proxy, but it is not precise in measurement of population differences. It cannot infer genetic similarity," he said.
Genetic testing "can mathematically calculate the place of origin genetically. Thus, it’s a more precise definition of race, and this methodology is important in teasing out those true factors of racial disparity. Simply put, this definition allows a continuous variable, a true percentage of African descent, as opposed to a categorical value of self-designated African American [race]," he said.
For the study, Dr. Rocconi and his coinvestigators identified women from Gynecologic Oncology Group (GOG) trial 210 who had endometroid tumors.
The team extracted DNA from tumor-free tissue samples and performed genotyping for 140 ancestry informative markers (AIMs), or single-nucleotide polymorphisms that occur in different frequencies in populations from different world geographic regions.
The 5-year rate of progression-free survival was 82% among self-reported white women and 74% among self-reported African American women, Dr. Rocconi reported.
Mean racial genetic admixture scores showed considerable racial genetic heterogeneity among both self-reported African American women (65% African, 20% European, and 15% Native American Indian) and self-reported white women (77% European, 17% Native American Indian, and 6% African).
After adjustment for self-reported race, women’s risk of progression or death rose significantly with each 1% increase in African racial genetic admixture (hazard ratio, 1.02) and fell significantly with each 1% increase in European racial genetic admixture (HR, 0.97).
When women were stratified into quintiles of African racial genetic admixture, the risk of events rose steadily with quintile. Relative to their peers having 0%-2% of this racial genetic composition, women having 72%-86% were 7.7 times more likely to experience progression or death.
"For a reference, this is higher than any of the factors we take into account on a daily basis when stratifying high- or intermediate-risk endometrial cancer for recurrence," noted Dr. Rocconi, who disclosed that the study was sponsored by Amgen through a Young Investigator Award.
LOS ANGELES – Racial makeup based on genetic testing trumps self-reported race as a predictor of endometrial cancer outcomes, suggests the results of a study reported at the annual meeting of the Society of Gynecologic Oncology.
Researchers compared patient self reports of racial identity and the results of genotyping for markers of race in 217 women with endometrial cancer who had any-stage endometroid tumors.
The risk of cancer progression or death rose by 2% with each 1% increase in African racial genetic admixture and fell by 3% with each 1% increase in European racial genetic admixture.
"Racial genetic admixture significantly predicts the risk of recurrence and progression-free survival in endometrial cancer patients. Importantly, this risk is irrespective of self-designated race and could be used to stratify and identify patients’ recurrence risk," reported lead author Dr. Rodney P. Rocconi, a gynecologic oncologist at the Mitchell Cancer Institute and University of South Alabama in Mobile.
The results are worth examining as a key "to unraveling the etiology of this disparity, with the hopes of improving treatment outcomes and eventually eliminating this racial disparity in the future."
Dr. Rocconi acknowledged that the study included only endometroid tumors, and noted that black women typically have higher proportions of carcinosarcoma and type 2 endometrial cancers, a distinction that’s not always known preoperatively.
"In an ideal world, we would like to evaluate that (larger) population," Dr. Rocconi said. But "it came down to having enough funding to evaluate a population that is meaningful. In the future, by all means, it would be an extremely important population to look at."
African American women make up just 7% of all patients with endometrial cancer but account for 15% of deaths from the disease, he noted.
"To date, breaking down the definition of race in cancer racial disparity has largely been overlooked. Considering the majority of racial disparity research utilizes self-designated race, this in my opinion is the greatest limitation in this type of research. Self-designated race can be used as a proxy, but it is not precise in measurement of population differences. It cannot infer genetic similarity," he said.
Genetic testing "can mathematically calculate the place of origin genetically. Thus, it’s a more precise definition of race, and this methodology is important in teasing out those true factors of racial disparity. Simply put, this definition allows a continuous variable, a true percentage of African descent, as opposed to a categorical value of self-designated African American [race]," he said.
For the study, Dr. Rocconi and his coinvestigators identified women from Gynecologic Oncology Group (GOG) trial 210 who had endometroid tumors.
The team extracted DNA from tumor-free tissue samples and performed genotyping for 140 ancestry informative markers (AIMs), or single-nucleotide polymorphisms that occur in different frequencies in populations from different world geographic regions.
The 5-year rate of progression-free survival was 82% among self-reported white women and 74% among self-reported African American women, Dr. Rocconi reported.
Mean racial genetic admixture scores showed considerable racial genetic heterogeneity among both self-reported African American women (65% African, 20% European, and 15% Native American Indian) and self-reported white women (77% European, 17% Native American Indian, and 6% African).
After adjustment for self-reported race, women’s risk of progression or death rose significantly with each 1% increase in African racial genetic admixture (hazard ratio, 1.02) and fell significantly with each 1% increase in European racial genetic admixture (HR, 0.97).
When women were stratified into quintiles of African racial genetic admixture, the risk of events rose steadily with quintile. Relative to their peers having 0%-2% of this racial genetic composition, women having 72%-86% were 7.7 times more likely to experience progression or death.
"For a reference, this is higher than any of the factors we take into account on a daily basis when stratifying high- or intermediate-risk endometrial cancer for recurrence," noted Dr. Rocconi, who disclosed that the study was sponsored by Amgen through a Young Investigator Award.
LOS ANGELES – Racial makeup based on genetic testing trumps self-reported race as a predictor of endometrial cancer outcomes, suggests the results of a study reported at the annual meeting of the Society of Gynecologic Oncology.
Researchers compared patient self reports of racial identity and the results of genotyping for markers of race in 217 women with endometrial cancer who had any-stage endometroid tumors.
The risk of cancer progression or death rose by 2% with each 1% increase in African racial genetic admixture and fell by 3% with each 1% increase in European racial genetic admixture.
"Racial genetic admixture significantly predicts the risk of recurrence and progression-free survival in endometrial cancer patients. Importantly, this risk is irrespective of self-designated race and could be used to stratify and identify patients’ recurrence risk," reported lead author Dr. Rodney P. Rocconi, a gynecologic oncologist at the Mitchell Cancer Institute and University of South Alabama in Mobile.
The results are worth examining as a key "to unraveling the etiology of this disparity, with the hopes of improving treatment outcomes and eventually eliminating this racial disparity in the future."
Dr. Rocconi acknowledged that the study included only endometroid tumors, and noted that black women typically have higher proportions of carcinosarcoma and type 2 endometrial cancers, a distinction that’s not always known preoperatively.
"In an ideal world, we would like to evaluate that (larger) population," Dr. Rocconi said. But "it came down to having enough funding to evaluate a population that is meaningful. In the future, by all means, it would be an extremely important population to look at."
African American women make up just 7% of all patients with endometrial cancer but account for 15% of deaths from the disease, he noted.
"To date, breaking down the definition of race in cancer racial disparity has largely been overlooked. Considering the majority of racial disparity research utilizes self-designated race, this in my opinion is the greatest limitation in this type of research. Self-designated race can be used as a proxy, but it is not precise in measurement of population differences. It cannot infer genetic similarity," he said.
Genetic testing "can mathematically calculate the place of origin genetically. Thus, it’s a more precise definition of race, and this methodology is important in teasing out those true factors of racial disparity. Simply put, this definition allows a continuous variable, a true percentage of African descent, as opposed to a categorical value of self-designated African American [race]," he said.
For the study, Dr. Rocconi and his coinvestigators identified women from Gynecologic Oncology Group (GOG) trial 210 who had endometroid tumors.
The team extracted DNA from tumor-free tissue samples and performed genotyping for 140 ancestry informative markers (AIMs), or single-nucleotide polymorphisms that occur in different frequencies in populations from different world geographic regions.
The 5-year rate of progression-free survival was 82% among self-reported white women and 74% among self-reported African American women, Dr. Rocconi reported.
Mean racial genetic admixture scores showed considerable racial genetic heterogeneity among both self-reported African American women (65% African, 20% European, and 15% Native American Indian) and self-reported white women (77% European, 17% Native American Indian, and 6% African).
After adjustment for self-reported race, women’s risk of progression or death rose significantly with each 1% increase in African racial genetic admixture (hazard ratio, 1.02) and fell significantly with each 1% increase in European racial genetic admixture (HR, 0.97).
When women were stratified into quintiles of African racial genetic admixture, the risk of events rose steadily with quintile. Relative to their peers having 0%-2% of this racial genetic composition, women having 72%-86% were 7.7 times more likely to experience progression or death.
"For a reference, this is higher than any of the factors we take into account on a daily basis when stratifying high- or intermediate-risk endometrial cancer for recurrence," noted Dr. Rocconi, who disclosed that the study was sponsored by Amgen through a Young Investigator Award.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: The risk of progression or death rose by 2% with each 1% increase in African racial genetic admixture and fell by 3% with each 1% increase in European racial genetic admixture, irrespective of self-reported race.
Data source: An observational cohort study of 217 women with endometroid endometrial cancer from the GOG 210 trial.
Disclosures: Dr. Rocconi disclosed that the study was sponsored by Amgen through a Young Investigator Award.
HPV testing best predicts cervical neoplasia risk
LOS ANGELES – Testing for high-risk human papillomavirus appears to be more reliable than performing liquid-based cytology for assessing a woman’s risk of developing advanced cervical neoplasia, based on the final results of the ATHENA trial.
In the prospective cohort study, both types of testing were performed in 42,209 women aged 25 years or older presenting for routine cervical cancer screening. A subset of these women had annual follow-up including repeat testing and colposcopy over 3 years.
The cumulative incidence rate of grade 3 cervical intraepithelial neoplasia (CIN3) or more advanced neoplasia was 0.33% in women having negative results for high-risk HPV, but much higher at 0.77% in women having negative liquid-based cytology results, regardless of HPV results. In addition, combining the two types of testing yielded very little gain over HPV testing alone; the rate was 0.29% in women with negative results on both tests.
"The adjusted 3-year cumulative incidence rate of CIN3 or greater in high-risk HPV-negative women is less than half that of women who have liquid based cytology that is negative," said lead author Thomas C. Wright Jr. at the annual meeting of the Society of Gynecologic Oncology. "Co-testing with both liquid-based cytology and high-risk HPV provides very little benefit over using high-risk HPV testing alone for screening."
"These results, we believe, suggest that high-risk HPV testing and genotyping is superior to liquid-based cytology for cervical cancer screening. And one of the goals of this trial is to go to the FDA and to get approval for HPV with genotyping for primary screening," added Dr. Wright, director of the division of gynecologic and obstetrical pathology at Columbia (N.Y.) University Medical Center.
"Certainly, the new American Cancer Society, ASCCP [American Society for Colposcopy and Cervical Pathology], and ASCP [American Society for Clinical Pathology] guidelines recommend co-testing, which is cytology and HPV, as a preferred screening approach for women 30 years and older," Dr. Wright noted. "I think the data that I showed today suggest that cytology adds so little that we would really do well to look at primary HPV screening. It’s going to be up to regulatory agencies though, as well as societies such as the American Cancer Society to make risk-benefit analyses. But, certainly, the data look very promising."
The 3-year cumulative incidence rate of CIN3 or worse was about 10% overall among patients having positive test results for any of the 14 high-risk types of HPV assessed. The main driver, however, was positivity for HPV 16 – women positive for this HPV type had a CIN3 or worse rate of 25%. HPV 18 was a lesser but still major contributor, associated with a rate of nearly 11%. The rate was 5% for women positive for any of the other 12 high-risk HPV types.
The data show "the disproportionate impact of HPV 16 positivity on the 3-year cumulative incidence rate among individuals who are high-risk HPV positive," Dr. Wright commented. "It is actually well over double that of women who have the 14 other types of high-risk HPV pooled, and compared to the other high-risk types, you have a fivefold increase."
The trial was the U.S. regulatory trial to obtain FDA clearance for the cobas HPV Test (manufactured by Roche Molecular Systems), which detects 14 types of HPV associated with a high risk of cervical neoplasia and cancer.
The analyses reported were based on 42,209 women aged 25 years or older on enrollment. They had a median age of 41 years, and 83% were white. At baseline, 10% had a high-risk HPV infection as assessed by the cobas test and 6% had atypical squamous cells of undetermined significance (ASCUS) or more advanced cervical neoplasia as detected by cytology.
The widely differing rates of CIN3 or worse for women who were high-risk HPV negative versus liquid-based cytology negative "are very similar to what has been seen in a number of large European studies," Dr. Wright noted.
And the temporal trends for the various high-risk HPV groups generally mirror those observed in a previous series of women seen at a Kaiser facility who had 10 years of follow-up (J. Natl. Cancer Inst. 2005;97:1072-9). "High-risk HPV-negative women remain very low [risk] in the ATHENA as well as in the Kaiser series," he pointed out.
In his post-presentation discussion, Dr. Wright was asked whether the study findings lend "a further push for school-based HPV vaccines in the United States."
"I’m not sure how my data address that," he responded. "However, I firmly believe that we should have school-based HPV vaccination in the United States. I think that most people in this room would believe that the percentage of our vaccinated cohort in the United States is much smaller than it should be; some people would use the word ‘appalling’ to refer to the rate at which we have vaccinated. And I think that societies such as the Society of Gynecologic Oncology should take the lead in trying to" improve vaccine uptake.
Dr. Wright disclosed that he is a consultant for Roche Molecular Systems, BD Diagnostics, Cepheid, and Hologic. The trial was sponsored by Roche Molecular Systems.
LOS ANGELES – Testing for high-risk human papillomavirus appears to be more reliable than performing liquid-based cytology for assessing a woman’s risk of developing advanced cervical neoplasia, based on the final results of the ATHENA trial.
In the prospective cohort study, both types of testing were performed in 42,209 women aged 25 years or older presenting for routine cervical cancer screening. A subset of these women had annual follow-up including repeat testing and colposcopy over 3 years.
The cumulative incidence rate of grade 3 cervical intraepithelial neoplasia (CIN3) or more advanced neoplasia was 0.33% in women having negative results for high-risk HPV, but much higher at 0.77% in women having negative liquid-based cytology results, regardless of HPV results. In addition, combining the two types of testing yielded very little gain over HPV testing alone; the rate was 0.29% in women with negative results on both tests.
"The adjusted 3-year cumulative incidence rate of CIN3 or greater in high-risk HPV-negative women is less than half that of women who have liquid based cytology that is negative," said lead author Thomas C. Wright Jr. at the annual meeting of the Society of Gynecologic Oncology. "Co-testing with both liquid-based cytology and high-risk HPV provides very little benefit over using high-risk HPV testing alone for screening."
"These results, we believe, suggest that high-risk HPV testing and genotyping is superior to liquid-based cytology for cervical cancer screening. And one of the goals of this trial is to go to the FDA and to get approval for HPV with genotyping for primary screening," added Dr. Wright, director of the division of gynecologic and obstetrical pathology at Columbia (N.Y.) University Medical Center.
"Certainly, the new American Cancer Society, ASCCP [American Society for Colposcopy and Cervical Pathology], and ASCP [American Society for Clinical Pathology] guidelines recommend co-testing, which is cytology and HPV, as a preferred screening approach for women 30 years and older," Dr. Wright noted. "I think the data that I showed today suggest that cytology adds so little that we would really do well to look at primary HPV screening. It’s going to be up to regulatory agencies though, as well as societies such as the American Cancer Society to make risk-benefit analyses. But, certainly, the data look very promising."
The 3-year cumulative incidence rate of CIN3 or worse was about 10% overall among patients having positive test results for any of the 14 high-risk types of HPV assessed. The main driver, however, was positivity for HPV 16 – women positive for this HPV type had a CIN3 or worse rate of 25%. HPV 18 was a lesser but still major contributor, associated with a rate of nearly 11%. The rate was 5% for women positive for any of the other 12 high-risk HPV types.
The data show "the disproportionate impact of HPV 16 positivity on the 3-year cumulative incidence rate among individuals who are high-risk HPV positive," Dr. Wright commented. "It is actually well over double that of women who have the 14 other types of high-risk HPV pooled, and compared to the other high-risk types, you have a fivefold increase."
The trial was the U.S. regulatory trial to obtain FDA clearance for the cobas HPV Test (manufactured by Roche Molecular Systems), which detects 14 types of HPV associated with a high risk of cervical neoplasia and cancer.
The analyses reported were based on 42,209 women aged 25 years or older on enrollment. They had a median age of 41 years, and 83% were white. At baseline, 10% had a high-risk HPV infection as assessed by the cobas test and 6% had atypical squamous cells of undetermined significance (ASCUS) or more advanced cervical neoplasia as detected by cytology.
The widely differing rates of CIN3 or worse for women who were high-risk HPV negative versus liquid-based cytology negative "are very similar to what has been seen in a number of large European studies," Dr. Wright noted.
And the temporal trends for the various high-risk HPV groups generally mirror those observed in a previous series of women seen at a Kaiser facility who had 10 years of follow-up (J. Natl. Cancer Inst. 2005;97:1072-9). "High-risk HPV-negative women remain very low [risk] in the ATHENA as well as in the Kaiser series," he pointed out.
In his post-presentation discussion, Dr. Wright was asked whether the study findings lend "a further push for school-based HPV vaccines in the United States."
"I’m not sure how my data address that," he responded. "However, I firmly believe that we should have school-based HPV vaccination in the United States. I think that most people in this room would believe that the percentage of our vaccinated cohort in the United States is much smaller than it should be; some people would use the word ‘appalling’ to refer to the rate at which we have vaccinated. And I think that societies such as the Society of Gynecologic Oncology should take the lead in trying to" improve vaccine uptake.
Dr. Wright disclosed that he is a consultant for Roche Molecular Systems, BD Diagnostics, Cepheid, and Hologic. The trial was sponsored by Roche Molecular Systems.
LOS ANGELES – Testing for high-risk human papillomavirus appears to be more reliable than performing liquid-based cytology for assessing a woman’s risk of developing advanced cervical neoplasia, based on the final results of the ATHENA trial.
In the prospective cohort study, both types of testing were performed in 42,209 women aged 25 years or older presenting for routine cervical cancer screening. A subset of these women had annual follow-up including repeat testing and colposcopy over 3 years.
The cumulative incidence rate of grade 3 cervical intraepithelial neoplasia (CIN3) or more advanced neoplasia was 0.33% in women having negative results for high-risk HPV, but much higher at 0.77% in women having negative liquid-based cytology results, regardless of HPV results. In addition, combining the two types of testing yielded very little gain over HPV testing alone; the rate was 0.29% in women with negative results on both tests.
"The adjusted 3-year cumulative incidence rate of CIN3 or greater in high-risk HPV-negative women is less than half that of women who have liquid based cytology that is negative," said lead author Thomas C. Wright Jr. at the annual meeting of the Society of Gynecologic Oncology. "Co-testing with both liquid-based cytology and high-risk HPV provides very little benefit over using high-risk HPV testing alone for screening."
"These results, we believe, suggest that high-risk HPV testing and genotyping is superior to liquid-based cytology for cervical cancer screening. And one of the goals of this trial is to go to the FDA and to get approval for HPV with genotyping for primary screening," added Dr. Wright, director of the division of gynecologic and obstetrical pathology at Columbia (N.Y.) University Medical Center.
"Certainly, the new American Cancer Society, ASCCP [American Society for Colposcopy and Cervical Pathology], and ASCP [American Society for Clinical Pathology] guidelines recommend co-testing, which is cytology and HPV, as a preferred screening approach for women 30 years and older," Dr. Wright noted. "I think the data that I showed today suggest that cytology adds so little that we would really do well to look at primary HPV screening. It’s going to be up to regulatory agencies though, as well as societies such as the American Cancer Society to make risk-benefit analyses. But, certainly, the data look very promising."
The 3-year cumulative incidence rate of CIN3 or worse was about 10% overall among patients having positive test results for any of the 14 high-risk types of HPV assessed. The main driver, however, was positivity for HPV 16 – women positive for this HPV type had a CIN3 or worse rate of 25%. HPV 18 was a lesser but still major contributor, associated with a rate of nearly 11%. The rate was 5% for women positive for any of the other 12 high-risk HPV types.
The data show "the disproportionate impact of HPV 16 positivity on the 3-year cumulative incidence rate among individuals who are high-risk HPV positive," Dr. Wright commented. "It is actually well over double that of women who have the 14 other types of high-risk HPV pooled, and compared to the other high-risk types, you have a fivefold increase."
The trial was the U.S. regulatory trial to obtain FDA clearance for the cobas HPV Test (manufactured by Roche Molecular Systems), which detects 14 types of HPV associated with a high risk of cervical neoplasia and cancer.
The analyses reported were based on 42,209 women aged 25 years or older on enrollment. They had a median age of 41 years, and 83% were white. At baseline, 10% had a high-risk HPV infection as assessed by the cobas test and 6% had atypical squamous cells of undetermined significance (ASCUS) or more advanced cervical neoplasia as detected by cytology.
The widely differing rates of CIN3 or worse for women who were high-risk HPV negative versus liquid-based cytology negative "are very similar to what has been seen in a number of large European studies," Dr. Wright noted.
And the temporal trends for the various high-risk HPV groups generally mirror those observed in a previous series of women seen at a Kaiser facility who had 10 years of follow-up (J. Natl. Cancer Inst. 2005;97:1072-9). "High-risk HPV-negative women remain very low [risk] in the ATHENA as well as in the Kaiser series," he pointed out.
In his post-presentation discussion, Dr. Wright was asked whether the study findings lend "a further push for school-based HPV vaccines in the United States."
"I’m not sure how my data address that," he responded. "However, I firmly believe that we should have school-based HPV vaccination in the United States. I think that most people in this room would believe that the percentage of our vaccinated cohort in the United States is much smaller than it should be; some people would use the word ‘appalling’ to refer to the rate at which we have vaccinated. And I think that societies such as the Society of Gynecologic Oncology should take the lead in trying to" improve vaccine uptake.
Dr. Wright disclosed that he is a consultant for Roche Molecular Systems, BD Diagnostics, Cepheid, and Hologic. The trial was sponsored by Roche Molecular Systems.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major Finding: The 3-year cumulative incidence rate of CIN3 or more advanced neoplasia was 0.33% in women negative for high-risk HPV and 0.77% in women with negative liquid-based cytology results.
Data Source: A prospective cohort study of 42,209 women presenting for routine cervical cancer screening in the ATHENA trial
Disclosures: Dr. Wright disclosed that he is a consultant for Roche Molecular Systems, BD Diagnostics, Cepheid, and Hologic. The trial was sponsored by Roche Molecular Systems.
Guideline nonadherence linked to increased ovarian cancer deaths
LOS ANGELES – Guideline-adherent treatment can make the difference between life and death in patients with ovarian cancer, and it often hinges on where and from whom patients receive care, new data suggest.
In a retrospective, population-based study of more than 13,000 patients with epithelial ovarian cancer, only about 40% of patients received treatment adhering to that recommended by the National Comprehensive Cancer Network (NCCN).
Patients were more likely to receive guideline-adherent treatment if they went to high-volume hospitals (those treating at least 20 such patients each year) and high-volume physicians (those treating at least 10 such patients each year), according to results reported at the annual meeting of the Society of Gynecologic Oncology*. Still, in absolute terms, only about half of patients treated in high-volume hospitals or by high-volume surgeons received adherent treatment.
Compared with their counterparts who received guideline-adherent treatment, patients who received nonadherent treatment had a 33% higher risk of dying from their disease in the subsequent 5 years.
"NCCN guideline adherence predicts improved survival," lead investigator Dr. Robert E. Bristow commented in an interview. "A minority of patients is getting access to guideline care, and increased efforts to direct ovarian cancer patients to high-volume providers are warranted."
From a population-based perspective, much greater gains in survival can be achieved by centralizing ovarian cancer care to gynecologic oncologists and high-volume hospitals than through new chemotherapy drugs or experimental treatments, according to Dr. Bristow, who is director of the division of gynecologic oncology at the University of California, Irvine, medical center. The success of this model "has been demonstrated in Norway, where nonaccredited providers are not paid for any ovarian cancer care they deliver."
That said, the data cannot be used to discern the reasons for the overall poor rate of guideline adherence.
"In population-based data sets, you don’t have the granularity of data to tease out the nuances that might contribute to risk, like an infirm 85-year-old woman who can’t tolerate major surgery and aggressive surgery. We were not able to control for that," Dr. Bristow noted. Yet "only about 20% of patients had access to high-volume providers, and since high-volume providers are more likely to deliver appropriate care, the lack of access to these physicians and hospitals is probably the biggest reason (for nonadherence). By ensuring that we do everything possible to get ovarian cancer patients to the physicians and centers that are best equipped to take care of them, we will maximize each patient’s chance for the best possible outcome."
Analyses were based on 13,321 patients with epithelial ovarian cancer having data in the California Cancer Registry for the years 1999 through 2006. They had a median age of 61 years; 70% had stage III or IV disease, and 42% had serous tumor histology.
Among patients having data on these measures, 81% were treated at low-volume hospitals and 79% by low-volume surgeons. In multivariate analyses, patients were significantly more likely to receive nonadherent treatment if they were treated in low-volume hospitals (odds ratio, 1.83) or by low-volume physicians (OR, 1.19).
Overall, 37% of the patients received treatment recommended by NCCN guidelines. The 5-year disease-specific survival rate was 45% for the cohort overall. In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
"We are in the infancy of defining quality care for ovarian cancer," concluded Dr. Bristow. "We need to develop risk-adjusted models for comparison, to make sure we are comparing apples to apples, so to speak. We need to become more sophisticated in our measurement and reporting. Ideally, one day, everyone’s quality performance measures will be publicly available and patients and payers can choose for themselves where to go for care."
The investigators plan future research on such models and on universal reporting requirements. "There are also critical issues of racial and socioeconomic disparities in ovarian cancer care and outcomes that we are investigating," he said.
Dr. Bristow disclosed no relevant conflicts of interest.
Correction, 3/28/2013: An earlier version of this story misstated the name of the Society of Gynecologic Oncology.
 |
|
Dr. Maurie Markman comments:
The report from Bristow, et al., is provocative and raises reasonable
questions regarding the quality of care provided to patients with
ovarian cancer. However, it is critical to acknowledge that while this
report suggests an association between "guideline adherence" and
clinical outcome, it does not in any way demonstrate the inferior
outcome actually resulted from the lack of guideline adherence. For
example, it is highly likely that patients with more advanced disease or
with clinically relevant co-morbidity were less likely to
undergo primary cytoreductive surgery, and these factors are known to be
independently associated with inferior survival. Large databases, as
employed in this analysis, will almost certainly be unable to capture
these clinical factors (for example, performance status, presence of
massive ascites, or large-volume pleural effusion) that will influence
both the decision to perform surgery and the survival outcome.
Therefore, while this study requires follow-up evaluation, it would be
premature to believe outcomes would improve simply because of physician
adherence to a declared "guideline." In fact, inappropriate adherence
that goes against a physician’s clinical judgment may result in a worse
outcome for an individual patient.
Dr. Markman is the senior
vice president of clinical affairs and national director of medical
oncology for the Cancer Treatment Centers of America.
 |
|
Dr. Maurie Markman comments:
The report from Bristow, et al., is provocative and raises reasonable
questions regarding the quality of care provided to patients with
ovarian cancer. However, it is critical to acknowledge that while this
report suggests an association between "guideline adherence" and
clinical outcome, it does not in any way demonstrate the inferior
outcome actually resulted from the lack of guideline adherence. For
example, it is highly likely that patients with more advanced disease or
with clinically relevant co-morbidity were less likely to
undergo primary cytoreductive surgery, and these factors are known to be
independently associated with inferior survival. Large databases, as
employed in this analysis, will almost certainly be unable to capture
these clinical factors (for example, performance status, presence of
massive ascites, or large-volume pleural effusion) that will influence
both the decision to perform surgery and the survival outcome.
Therefore, while this study requires follow-up evaluation, it would be
premature to believe outcomes would improve simply because of physician
adherence to a declared "guideline." In fact, inappropriate adherence
that goes against a physician’s clinical judgment may result in a worse
outcome for an individual patient.
Dr. Markman is the senior
vice president of clinical affairs and national director of medical
oncology for the Cancer Treatment Centers of America.
 |
|
Dr. Maurie Markman comments:
The report from Bristow, et al., is provocative and raises reasonable
questions regarding the quality of care provided to patients with
ovarian cancer. However, it is critical to acknowledge that while this
report suggests an association between "guideline adherence" and
clinical outcome, it does not in any way demonstrate the inferior
outcome actually resulted from the lack of guideline adherence. For
example, it is highly likely that patients with more advanced disease or
with clinically relevant co-morbidity were less likely to
undergo primary cytoreductive surgery, and these factors are known to be
independently associated with inferior survival. Large databases, as
employed in this analysis, will almost certainly be unable to capture
these clinical factors (for example, performance status, presence of
massive ascites, or large-volume pleural effusion) that will influence
both the decision to perform surgery and the survival outcome.
Therefore, while this study requires follow-up evaluation, it would be
premature to believe outcomes would improve simply because of physician
adherence to a declared "guideline." In fact, inappropriate adherence
that goes against a physician’s clinical judgment may result in a worse
outcome for an individual patient.
Dr. Markman is the senior
vice president of clinical affairs and national director of medical
oncology for the Cancer Treatment Centers of America.
LOS ANGELES – Guideline-adherent treatment can make the difference between life and death in patients with ovarian cancer, and it often hinges on where and from whom patients receive care, new data suggest.
In a retrospective, population-based study of more than 13,000 patients with epithelial ovarian cancer, only about 40% of patients received treatment adhering to that recommended by the National Comprehensive Cancer Network (NCCN).
Patients were more likely to receive guideline-adherent treatment if they went to high-volume hospitals (those treating at least 20 such patients each year) and high-volume physicians (those treating at least 10 such patients each year), according to results reported at the annual meeting of the Society of Gynecologic Oncology*. Still, in absolute terms, only about half of patients treated in high-volume hospitals or by high-volume surgeons received adherent treatment.
Compared with their counterparts who received guideline-adherent treatment, patients who received nonadherent treatment had a 33% higher risk of dying from their disease in the subsequent 5 years.
"NCCN guideline adherence predicts improved survival," lead investigator Dr. Robert E. Bristow commented in an interview. "A minority of patients is getting access to guideline care, and increased efforts to direct ovarian cancer patients to high-volume providers are warranted."
From a population-based perspective, much greater gains in survival can be achieved by centralizing ovarian cancer care to gynecologic oncologists and high-volume hospitals than through new chemotherapy drugs or experimental treatments, according to Dr. Bristow, who is director of the division of gynecologic oncology at the University of California, Irvine, medical center. The success of this model "has been demonstrated in Norway, where nonaccredited providers are not paid for any ovarian cancer care they deliver."
That said, the data cannot be used to discern the reasons for the overall poor rate of guideline adherence.
"In population-based data sets, you don’t have the granularity of data to tease out the nuances that might contribute to risk, like an infirm 85-year-old woman who can’t tolerate major surgery and aggressive surgery. We were not able to control for that," Dr. Bristow noted. Yet "only about 20% of patients had access to high-volume providers, and since high-volume providers are more likely to deliver appropriate care, the lack of access to these physicians and hospitals is probably the biggest reason (for nonadherence). By ensuring that we do everything possible to get ovarian cancer patients to the physicians and centers that are best equipped to take care of them, we will maximize each patient’s chance for the best possible outcome."
Analyses were based on 13,321 patients with epithelial ovarian cancer having data in the California Cancer Registry for the years 1999 through 2006. They had a median age of 61 years; 70% had stage III or IV disease, and 42% had serous tumor histology.
Among patients having data on these measures, 81% were treated at low-volume hospitals and 79% by low-volume surgeons. In multivariate analyses, patients were significantly more likely to receive nonadherent treatment if they were treated in low-volume hospitals (odds ratio, 1.83) or by low-volume physicians (OR, 1.19).
Overall, 37% of the patients received treatment recommended by NCCN guidelines. The 5-year disease-specific survival rate was 45% for the cohort overall. In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
"We are in the infancy of defining quality care for ovarian cancer," concluded Dr. Bristow. "We need to develop risk-adjusted models for comparison, to make sure we are comparing apples to apples, so to speak. We need to become more sophisticated in our measurement and reporting. Ideally, one day, everyone’s quality performance measures will be publicly available and patients and payers can choose for themselves where to go for care."
The investigators plan future research on such models and on universal reporting requirements. "There are also critical issues of racial and socioeconomic disparities in ovarian cancer care and outcomes that we are investigating," he said.
Dr. Bristow disclosed no relevant conflicts of interest.
Correction, 3/28/2013: An earlier version of this story misstated the name of the Society of Gynecologic Oncology.
LOS ANGELES – Guideline-adherent treatment can make the difference between life and death in patients with ovarian cancer, and it often hinges on where and from whom patients receive care, new data suggest.
In a retrospective, population-based study of more than 13,000 patients with epithelial ovarian cancer, only about 40% of patients received treatment adhering to that recommended by the National Comprehensive Cancer Network (NCCN).
Patients were more likely to receive guideline-adherent treatment if they went to high-volume hospitals (those treating at least 20 such patients each year) and high-volume physicians (those treating at least 10 such patients each year), according to results reported at the annual meeting of the Society of Gynecologic Oncology*. Still, in absolute terms, only about half of patients treated in high-volume hospitals or by high-volume surgeons received adherent treatment.
Compared with their counterparts who received guideline-adherent treatment, patients who received nonadherent treatment had a 33% higher risk of dying from their disease in the subsequent 5 years.
"NCCN guideline adherence predicts improved survival," lead investigator Dr. Robert E. Bristow commented in an interview. "A minority of patients is getting access to guideline care, and increased efforts to direct ovarian cancer patients to high-volume providers are warranted."
From a population-based perspective, much greater gains in survival can be achieved by centralizing ovarian cancer care to gynecologic oncologists and high-volume hospitals than through new chemotherapy drugs or experimental treatments, according to Dr. Bristow, who is director of the division of gynecologic oncology at the University of California, Irvine, medical center. The success of this model "has been demonstrated in Norway, where nonaccredited providers are not paid for any ovarian cancer care they deliver."
That said, the data cannot be used to discern the reasons for the overall poor rate of guideline adherence.
"In population-based data sets, you don’t have the granularity of data to tease out the nuances that might contribute to risk, like an infirm 85-year-old woman who can’t tolerate major surgery and aggressive surgery. We were not able to control for that," Dr. Bristow noted. Yet "only about 20% of patients had access to high-volume providers, and since high-volume providers are more likely to deliver appropriate care, the lack of access to these physicians and hospitals is probably the biggest reason (for nonadherence). By ensuring that we do everything possible to get ovarian cancer patients to the physicians and centers that are best equipped to take care of them, we will maximize each patient’s chance for the best possible outcome."
Analyses were based on 13,321 patients with epithelial ovarian cancer having data in the California Cancer Registry for the years 1999 through 2006. They had a median age of 61 years; 70% had stage III or IV disease, and 42% had serous tumor histology.
Among patients having data on these measures, 81% were treated at low-volume hospitals and 79% by low-volume surgeons. In multivariate analyses, patients were significantly more likely to receive nonadherent treatment if they were treated in low-volume hospitals (odds ratio, 1.83) or by low-volume physicians (OR, 1.19).
Overall, 37% of the patients received treatment recommended by NCCN guidelines. The 5-year disease-specific survival rate was 45% for the cohort overall. In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
"We are in the infancy of defining quality care for ovarian cancer," concluded Dr. Bristow. "We need to develop risk-adjusted models for comparison, to make sure we are comparing apples to apples, so to speak. We need to become more sophisticated in our measurement and reporting. Ideally, one day, everyone’s quality performance measures will be publicly available and patients and payers can choose for themselves where to go for care."
The investigators plan future research on such models and on universal reporting requirements. "There are also critical issues of racial and socioeconomic disparities in ovarian cancer care and outcomes that we are investigating," he said.
Dr. Bristow disclosed no relevant conflicts of interest.
Correction, 3/28/2013: An earlier version of this story misstated the name of the Society of Gynecologic Oncology.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Major finding: In multivariate analyses, patients had significantly higher odds of ovarian cancer death if they received nonadherent treatment (hazard ratio, 1.33), and if they were treated at a low-volume hospital (HR, 1.08) or by a low-volume physician (HR, 1.18).
Data source: A retrospective population-based cohort study of 13,321 patients with epithelial ovarian cancer from the California Cancer Registry
Disclosures: Dr. Bristow disclosed no relevant conflicts of interest.