User login
Ribociclib/ET improves OS in premenopausal women with HR+/HER2- breast cancer
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis conducted at 42 months showed that the overall survival rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib was 70%, compared with 46% for women randomized to endocrine therapy alone, reported Sara A Hurvitz, MD, of the University of California Los Angeles Jonsson Comprehensive Cancer Center
“This is the first time a statistically significant improvement in overall survival has been observed with a CDK4/6 inhibitor in combination with endocrine therapy in patients with hormone receptor-positive advanced disease,” she said at a briefing prior to her presentation of the data in an oral abstract session at the American Society of Clinical Oncology annual meeting.
“This is an important study, because it shows that the class of drugs, CDK4/6 inhibitors, which we are widely using, has been shown to delay the time to progression, delay the time to need for chemotherapy for advanced breast cancer, and really doubled the effectiveness of endocrine therapy, now also translates into a significant survival benefit for women who ER-positive metastatic breast cancer,” commented Harold J. Burstein, MD, PhD, an ASCO expert from the Dana-Farber Cancer Institute in Boston.
In the trial, 672 pre- or perimenopausal women with HR+/HER2– advanced breast cancer with no prior endocrine therapy for advanced disease and no more than one line of chemotherapy for advanced disease were enrolled. The patients were stratified by the presence of liver/lung metastases, prior chemotherapy, and prior endocrine partner, tamoxifen or nonsteroidal AI, and then randomly assigned to ribociclib 600 mg/day for 3 weeks, followed by 1-week off, plus tamoxifen or AI and goserelin, or the same combination and schedule with placebo.
Of the 672 patients enrolled, a total of 335 patients assigned to ribociclib and 337 assigned to placebo received treatment. The majority of patients – 495 – received an AI, either letrozole (Femara) or anastrozole (Arimidex). Dr. Hurvitz noted that after the initiation of MONALEESA-7, the combination of a CDK4/6 inhibitor and tamoxifen was found to prolong the QT interval and increase risk for cardiac arrhythmias, and is now contraindicated.
As previously reported , results of the primary MONALEESA-7 endpoint of progression-free survival favored the combination, with a median PFS of 23.8 months, compared with 13 months for women treated with endocrine therapy alone. The hazard ratio for progression with the ribociclib-based combination was 0.553 ( P less than .0001), and the treatment benefit of the CDK4/6 inhibitor was seen across all patients subgroups and regardless of the endocrine partner.
At ASCO 2019, Dr. Hurvitz reported on the key secondary endpoint of overall survival. At a median follow-up duration of 34.6 months, with an additional 15 months beyond the initial analysis, the median OS for the ribociclib arm was not reached, compared with 40.9 months in the placebo arm. The hazard ratio for death with ribociclib was 0.712 ( P = .00973). An analysis of OS by endocrine partner subgroup showed no significant differences between AIs or tamoxifen.
At the time of the data cutoff, 35% of patients in the ribociclib arm were still on therapy.
The safety and tolerability of the combination were consistent with those previously reported, Dr. Hurvitz said.
“In an era when we are thinking about value in oncology care, a demonstration of a robust sutvival difference I think substantially adds to a value proposition for products like ribociclib that were discussed here,” Dr. Burstein said.
“Hopefully, these data will enable access to this product to more women around the world, particularly in health care systems that assess value rigorously as part of their decisions for national access to drugs,” he added.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis. Dr. Burstein reported no relevant disclosures.
SOURCE: Hurvitz SA et al. ASCO 2019. Abstract LBA1008 .
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis conducted at 42 months showed that the overall survival rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib was 70%, compared with 46% for women randomized to endocrine therapy alone, reported Sara A Hurvitz, MD, of the University of California Los Angeles Jonsson Comprehensive Cancer Center
“This is the first time a statistically significant improvement in overall survival has been observed with a CDK4/6 inhibitor in combination with endocrine therapy in patients with hormone receptor-positive advanced disease,” she said at a briefing prior to her presentation of the data in an oral abstract session at the American Society of Clinical Oncology annual meeting.
“This is an important study, because it shows that the class of drugs, CDK4/6 inhibitors, which we are widely using, has been shown to delay the time to progression, delay the time to need for chemotherapy for advanced breast cancer, and really doubled the effectiveness of endocrine therapy, now also translates into a significant survival benefit for women who ER-positive metastatic breast cancer,” commented Harold J. Burstein, MD, PhD, an ASCO expert from the Dana-Farber Cancer Institute in Boston.
In the trial, 672 pre- or perimenopausal women with HR+/HER2– advanced breast cancer with no prior endocrine therapy for advanced disease and no more than one line of chemotherapy for advanced disease were enrolled. The patients were stratified by the presence of liver/lung metastases, prior chemotherapy, and prior endocrine partner, tamoxifen or nonsteroidal AI, and then randomly assigned to ribociclib 600 mg/day for 3 weeks, followed by 1-week off, plus tamoxifen or AI and goserelin, or the same combination and schedule with placebo.
Of the 672 patients enrolled, a total of 335 patients assigned to ribociclib and 337 assigned to placebo received treatment. The majority of patients – 495 – received an AI, either letrozole (Femara) or anastrozole (Arimidex). Dr. Hurvitz noted that after the initiation of MONALEESA-7, the combination of a CDK4/6 inhibitor and tamoxifen was found to prolong the QT interval and increase risk for cardiac arrhythmias, and is now contraindicated.
As previously reported , results of the primary MONALEESA-7 endpoint of progression-free survival favored the combination, with a median PFS of 23.8 months, compared with 13 months for women treated with endocrine therapy alone. The hazard ratio for progression with the ribociclib-based combination was 0.553 ( P less than .0001), and the treatment benefit of the CDK4/6 inhibitor was seen across all patients subgroups and regardless of the endocrine partner.
At ASCO 2019, Dr. Hurvitz reported on the key secondary endpoint of overall survival. At a median follow-up duration of 34.6 months, with an additional 15 months beyond the initial analysis, the median OS for the ribociclib arm was not reached, compared with 40.9 months in the placebo arm. The hazard ratio for death with ribociclib was 0.712 ( P = .00973). An analysis of OS by endocrine partner subgroup showed no significant differences between AIs or tamoxifen.
At the time of the data cutoff, 35% of patients in the ribociclib arm were still on therapy.
The safety and tolerability of the combination were consistent with those previously reported, Dr. Hurvitz said.
“In an era when we are thinking about value in oncology care, a demonstration of a robust sutvival difference I think substantially adds to a value proposition for products like ribociclib that were discussed here,” Dr. Burstein said.
“Hopefully, these data will enable access to this product to more women around the world, particularly in health care systems that assess value rigorously as part of their decisions for national access to drugs,” he added.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis. Dr. Burstein reported no relevant disclosures.
SOURCE: Hurvitz SA et al. ASCO 2019. Abstract LBA1008 .
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis conducted at 42 months showed that the overall survival rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib was 70%, compared with 46% for women randomized to endocrine therapy alone, reported Sara A Hurvitz, MD, of the University of California Los Angeles Jonsson Comprehensive Cancer Center
“This is the first time a statistically significant improvement in overall survival has been observed with a CDK4/6 inhibitor in combination with endocrine therapy in patients with hormone receptor-positive advanced disease,” she said at a briefing prior to her presentation of the data in an oral abstract session at the American Society of Clinical Oncology annual meeting.
“This is an important study, because it shows that the class of drugs, CDK4/6 inhibitors, which we are widely using, has been shown to delay the time to progression, delay the time to need for chemotherapy for advanced breast cancer, and really doubled the effectiveness of endocrine therapy, now also translates into a significant survival benefit for women who ER-positive metastatic breast cancer,” commented Harold J. Burstein, MD, PhD, an ASCO expert from the Dana-Farber Cancer Institute in Boston.
In the trial, 672 pre- or perimenopausal women with HR+/HER2– advanced breast cancer with no prior endocrine therapy for advanced disease and no more than one line of chemotherapy for advanced disease were enrolled. The patients were stratified by the presence of liver/lung metastases, prior chemotherapy, and prior endocrine partner, tamoxifen or nonsteroidal AI, and then randomly assigned to ribociclib 600 mg/day for 3 weeks, followed by 1-week off, plus tamoxifen or AI and goserelin, or the same combination and schedule with placebo.
Of the 672 patients enrolled, a total of 335 patients assigned to ribociclib and 337 assigned to placebo received treatment. The majority of patients – 495 – received an AI, either letrozole (Femara) or anastrozole (Arimidex). Dr. Hurvitz noted that after the initiation of MONALEESA-7, the combination of a CDK4/6 inhibitor and tamoxifen was found to prolong the QT interval and increase risk for cardiac arrhythmias, and is now contraindicated.
As previously reported , results of the primary MONALEESA-7 endpoint of progression-free survival favored the combination, with a median PFS of 23.8 months, compared with 13 months for women treated with endocrine therapy alone. The hazard ratio for progression with the ribociclib-based combination was 0.553 ( P less than .0001), and the treatment benefit of the CDK4/6 inhibitor was seen across all patients subgroups and regardless of the endocrine partner.
At ASCO 2019, Dr. Hurvitz reported on the key secondary endpoint of overall survival. At a median follow-up duration of 34.6 months, with an additional 15 months beyond the initial analysis, the median OS for the ribociclib arm was not reached, compared with 40.9 months in the placebo arm. The hazard ratio for death with ribociclib was 0.712 ( P = .00973). An analysis of OS by endocrine partner subgroup showed no significant differences between AIs or tamoxifen.
At the time of the data cutoff, 35% of patients in the ribociclib arm were still on therapy.
The safety and tolerability of the combination were consistent with those previously reported, Dr. Hurvitz said.
“In an era when we are thinking about value in oncology care, a demonstration of a robust sutvival difference I think substantially adds to a value proposition for products like ribociclib that were discussed here,” Dr. Burstein said.
“Hopefully, these data will enable access to this product to more women around the world, particularly in health care systems that assess value rigorously as part of their decisions for national access to drugs,” he added.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis. Dr. Burstein reported no relevant disclosures.
SOURCE: Hurvitz SA et al. ASCO 2019. Abstract LBA1008 .
REPORTING FROM ASCO 2019
Pembro as good as chemo for gastric cancers with less toxicity
CHICAGO – In gastric and gastroesophageal junction (GEJ) cancers, positive for PD-L1, treatment with the PD-1 inhibitor pembrolizumab offered comparable survival with fewer side effects, according to results of a phase 3 randomized clinical trial.
The checkpoint inhibitor also demonstrated a clinically meaningful improvement in patients who had high levels of PD-L1 expression, with a 2-year survival rate of 39% versus 22% for patients receiving the standard chemotherapy, which consisted of a platinum and a fluoropyrimidine, according to Josep Tabernero, MD, PhD, lead author of the KEYNOTE-062 study.
By contrast, the study failed to demonstrate that pembrolizumab immunotherapy combined with that chemotherapy backbone was superior to chemotherapy alone on survival endpoints, said Dr. Tabernero, Head of the Medical Oncology Department at the Vall d’Hebron Barcelona University Hospital and Institute of Oncology, Spain.
“There are several factors we are evaluating,” Dr. Tabernero said here in a press conference at the annual meeting of the American Society of Clinical Oncology (ASCO). “We still have to do more studies to understand why, with this chemotherapy backbone, we don’t see a clear synergistic effect for superiority in overall survival.”
Nevertheless, these findings make pembrolizumab a “preferred treatment” for many patients, particularly in light of its “substantially improved safety profile” versus chemotherapy, said ASCO Senior Vice President and Chief Medical Officer Richard L. Schilsky, MD.
“What I take away from this study is that for patients with advanced gastric and gastroesophageal cancer, pembrolizumab should really in many cases replace chemotherapy as a first-line treatment for this population,” Dr. Schilsky said in a press conference. “It’s certainly not worse, and it may well be better.”
The KEYNOTE-062 study included 763 patients with HER2-negative, PD-L1-positive advanced gastric or GEJ cancers randomized to one of three arms: pembrolizumab alone for up to 35 cycles, pembrolizumab for up to 35 cycles plus chemotherapy, or placebo plus chemotherapy.
Pembrolizumab alone was not inferior compared to chemotherapy, with median overall survival rates of 10.5 and 11.1 months, respectively (HR, 0.91; 99.2% CI, 0.69-1.18), Dr. Tabernero reported.
Overall survival appeared to be prolonged in patients with high levels of PD-L1 expression, defined as a combined positive score (CPS) of 10 or greater. The median survival in that subgroup was 17.4 months for those receiving pembrolizumab, and just 10.8 months for chemotherapy. However, the design of the study precluded an analysis of statistical significance for this finding, according to Dr. Tabernero.
Looking at the overall study population, pembrolizumab plus chemotherapy did not improve survival versus chemotherapy alone, he added, reporting median overall survivals of 12.5 and 11.1 months, respectively (P = .046).
Subgroup analysis suggested that Asian patients derived particular benefit from pembrolizumab as compared to chemotherapy, though Dr. Tabernero cautioned against overinterpretation of the finding, saying that it could be due to biology, or could be a statistical anomaly.
Funding for the study came from Merck & Co., Inc. Dr. Tabernero reported disclosures related to Bayer, Boehringer Ingelheim, Lilly, MSD, Merck Serono, Novartis, Sanofi, and others.
SOURCE: Tabernero J, et al. ASCO 2019. Abstract LBA4007.
CHICAGO – In gastric and gastroesophageal junction (GEJ) cancers, positive for PD-L1, treatment with the PD-1 inhibitor pembrolizumab offered comparable survival with fewer side effects, according to results of a phase 3 randomized clinical trial.
The checkpoint inhibitor also demonstrated a clinically meaningful improvement in patients who had high levels of PD-L1 expression, with a 2-year survival rate of 39% versus 22% for patients receiving the standard chemotherapy, which consisted of a platinum and a fluoropyrimidine, according to Josep Tabernero, MD, PhD, lead author of the KEYNOTE-062 study.
By contrast, the study failed to demonstrate that pembrolizumab immunotherapy combined with that chemotherapy backbone was superior to chemotherapy alone on survival endpoints, said Dr. Tabernero, Head of the Medical Oncology Department at the Vall d’Hebron Barcelona University Hospital and Institute of Oncology, Spain.
“There are several factors we are evaluating,” Dr. Tabernero said here in a press conference at the annual meeting of the American Society of Clinical Oncology (ASCO). “We still have to do more studies to understand why, with this chemotherapy backbone, we don’t see a clear synergistic effect for superiority in overall survival.”
Nevertheless, these findings make pembrolizumab a “preferred treatment” for many patients, particularly in light of its “substantially improved safety profile” versus chemotherapy, said ASCO Senior Vice President and Chief Medical Officer Richard L. Schilsky, MD.
“What I take away from this study is that for patients with advanced gastric and gastroesophageal cancer, pembrolizumab should really in many cases replace chemotherapy as a first-line treatment for this population,” Dr. Schilsky said in a press conference. “It’s certainly not worse, and it may well be better.”
The KEYNOTE-062 study included 763 patients with HER2-negative, PD-L1-positive advanced gastric or GEJ cancers randomized to one of three arms: pembrolizumab alone for up to 35 cycles, pembrolizumab for up to 35 cycles plus chemotherapy, or placebo plus chemotherapy.
Pembrolizumab alone was not inferior compared to chemotherapy, with median overall survival rates of 10.5 and 11.1 months, respectively (HR, 0.91; 99.2% CI, 0.69-1.18), Dr. Tabernero reported.
Overall survival appeared to be prolonged in patients with high levels of PD-L1 expression, defined as a combined positive score (CPS) of 10 or greater. The median survival in that subgroup was 17.4 months for those receiving pembrolizumab, and just 10.8 months for chemotherapy. However, the design of the study precluded an analysis of statistical significance for this finding, according to Dr. Tabernero.
Looking at the overall study population, pembrolizumab plus chemotherapy did not improve survival versus chemotherapy alone, he added, reporting median overall survivals of 12.5 and 11.1 months, respectively (P = .046).
Subgroup analysis suggested that Asian patients derived particular benefit from pembrolizumab as compared to chemotherapy, though Dr. Tabernero cautioned against overinterpretation of the finding, saying that it could be due to biology, or could be a statistical anomaly.
Funding for the study came from Merck & Co., Inc. Dr. Tabernero reported disclosures related to Bayer, Boehringer Ingelheim, Lilly, MSD, Merck Serono, Novartis, Sanofi, and others.
SOURCE: Tabernero J, et al. ASCO 2019. Abstract LBA4007.
CHICAGO – In gastric and gastroesophageal junction (GEJ) cancers, positive for PD-L1, treatment with the PD-1 inhibitor pembrolizumab offered comparable survival with fewer side effects, according to results of a phase 3 randomized clinical trial.
The checkpoint inhibitor also demonstrated a clinically meaningful improvement in patients who had high levels of PD-L1 expression, with a 2-year survival rate of 39% versus 22% for patients receiving the standard chemotherapy, which consisted of a platinum and a fluoropyrimidine, according to Josep Tabernero, MD, PhD, lead author of the KEYNOTE-062 study.
By contrast, the study failed to demonstrate that pembrolizumab immunotherapy combined with that chemotherapy backbone was superior to chemotherapy alone on survival endpoints, said Dr. Tabernero, Head of the Medical Oncology Department at the Vall d’Hebron Barcelona University Hospital and Institute of Oncology, Spain.
“There are several factors we are evaluating,” Dr. Tabernero said here in a press conference at the annual meeting of the American Society of Clinical Oncology (ASCO). “We still have to do more studies to understand why, with this chemotherapy backbone, we don’t see a clear synergistic effect for superiority in overall survival.”
Nevertheless, these findings make pembrolizumab a “preferred treatment” for many patients, particularly in light of its “substantially improved safety profile” versus chemotherapy, said ASCO Senior Vice President and Chief Medical Officer Richard L. Schilsky, MD.
“What I take away from this study is that for patients with advanced gastric and gastroesophageal cancer, pembrolizumab should really in many cases replace chemotherapy as a first-line treatment for this population,” Dr. Schilsky said in a press conference. “It’s certainly not worse, and it may well be better.”
The KEYNOTE-062 study included 763 patients with HER2-negative, PD-L1-positive advanced gastric or GEJ cancers randomized to one of three arms: pembrolizumab alone for up to 35 cycles, pembrolizumab for up to 35 cycles plus chemotherapy, or placebo plus chemotherapy.
Pembrolizumab alone was not inferior compared to chemotherapy, with median overall survival rates of 10.5 and 11.1 months, respectively (HR, 0.91; 99.2% CI, 0.69-1.18), Dr. Tabernero reported.
Overall survival appeared to be prolonged in patients with high levels of PD-L1 expression, defined as a combined positive score (CPS) of 10 or greater. The median survival in that subgroup was 17.4 months for those receiving pembrolizumab, and just 10.8 months for chemotherapy. However, the design of the study precluded an analysis of statistical significance for this finding, according to Dr. Tabernero.
Looking at the overall study population, pembrolizumab plus chemotherapy did not improve survival versus chemotherapy alone, he added, reporting median overall survivals of 12.5 and 11.1 months, respectively (P = .046).
Subgroup analysis suggested that Asian patients derived particular benefit from pembrolizumab as compared to chemotherapy, though Dr. Tabernero cautioned against overinterpretation of the finding, saying that it could be due to biology, or could be a statistical anomaly.
Funding for the study came from Merck & Co., Inc. Dr. Tabernero reported disclosures related to Bayer, Boehringer Ingelheim, Lilly, MSD, Merck Serono, Novartis, Sanofi, and others.
SOURCE: Tabernero J, et al. ASCO 2019. Abstract LBA4007.
REPORTING FROM ASCO 2019
SC-PEG comparable to pegaspargase in young ALL/LL patients
CHICAGO – Calaspargase pegol (SC-PEG) produces similar outcomes as standard pegaspargase in pediatric and young adult patients with newly diagnosed acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), according to a phase 2 trial.
Patients who received SC-PEG every 3 weeks had similar serum asparaginase activity (SAA), toxicities, and survival rates as patients who received standard pegaspargase every 2 weeks.
Lynda M. Vrooman, MD, of Dana-Farber Cancer Institute in Boston, presented these results at the annual meeting of the American Society of Clinical Oncology.
The trial (NCT01574274) enrolled 239 patients, 230 with ALL and 9 with LL. Most patients had B-cell (n = 207) disease. The patients’ median age was 5.2 years (range, 1.0-20.9 years).
“There were no differences in presenting features by randomization,” Dr. Vrooman noted.
The patients were randomized to receive pegaspargase (n = 120) or SC-PEG (n = 119), a pegylated asparaginase formulation with longer half-life. SC-PEG was given at 2,500 IU/m2 every 3 weeks, and pegaspargase was given at 2,500 IU/m2 every 2 weeks.
Either asparaginase product was given as part of a 4-week induction regimen (vincristine, prednisone, doxorubicin, and methotrexate), a 3-week intensification regimen (intrathecal chemotherapy with or without radiotherapy) for central nervous system disease, and a 27-week second consolidation regimen (mercaptopurine, methotrexate, and, in high-risk patients, doxorubicin).
SAA
The researchers observed significantly longer SAA with SC-PEG during induction but not after.
During induction, at 25 days after the first asparaginase dose, 88% of patients on SC-PEG and 17% of those on pegaspargase had SAA of at least 0.10 IU/mL (P less than .001). Post-induction, at week 25, 100% of patients in each group had a nadir SAA of at least 0.10 IU/mL.
“The high nadir serum asparaginase activity levels observed for both preparations suggest dosing strategies could be further optimized,” Dr. Vrooman noted.
Safety
There were no significant differences in adverse events between the SC-PEG and pegaspargase arms during or after induction.
Adverse events during induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (0% and 1%), grade 2 or higher pancreatitis (3% in both), grade 2 or higher thrombosis (3% and 9%), grade 4 hyperbilirubinemia (3% and 1%), grade 3 or higher bacterial infection (12% and 9%), and grade 3 or higher fungal infection (4% and 5%).
Adverse events after induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (17% and 14%), grade 2 or higher pancreatitis (15% in both), grade 2 or higher thrombosis (18% and 13%), grade 4 hyperbilirubinemia (4% and 3%), grade 3 or higher bacterial infection (12% and 15%), grade 3 or higher fungal infection (2% and 1%), grade 2 or higher bone fracture (3% and 8%), and grade 2 or higher osteonecrosis (3% and 4%).
Response and survival
The complete response rate was 95% (109/115) in the SC-PEG arm and 99% (114/115) in the pegaspargase arm. Rates of induction failure were 3% (n = 4) and 1% (n = 1), respectively, and rates of relapse were 3% (n = 5) and 8% (n = 10), respectively.
There were two induction deaths and two remission deaths in the SC-PEG arm but no induction or remission deaths in the pegaspargase arm.
The median follow-up was 4 years. The 4-year event-free survival rate was 87.7% with SC-PEG and 90.2% with pegaspargase (P = .78). The 4-year overall survival rate was 94.8% and 95.6%, respectively (P = .74).
In closing, Dr. Vrooman said these data suggest SC-PEG provides similar results as standard pegaspargase. She noted that these data informed the U.S. approval of SC-PEG for pediatric and young adult ALL.
This trial was sponsored by the Dana-Farber Cancer Institute in collaboration with Shire and the National Cancer Institute. Dr. Vrooman said she had no relationships to disclose.
SOURCE: Vrooman LM et al. ASCO 2019. Abstract 10006.
CHICAGO – Calaspargase pegol (SC-PEG) produces similar outcomes as standard pegaspargase in pediatric and young adult patients with newly diagnosed acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), according to a phase 2 trial.
Patients who received SC-PEG every 3 weeks had similar serum asparaginase activity (SAA), toxicities, and survival rates as patients who received standard pegaspargase every 2 weeks.
Lynda M. Vrooman, MD, of Dana-Farber Cancer Institute in Boston, presented these results at the annual meeting of the American Society of Clinical Oncology.
The trial (NCT01574274) enrolled 239 patients, 230 with ALL and 9 with LL. Most patients had B-cell (n = 207) disease. The patients’ median age was 5.2 years (range, 1.0-20.9 years).
“There were no differences in presenting features by randomization,” Dr. Vrooman noted.
The patients were randomized to receive pegaspargase (n = 120) or SC-PEG (n = 119), a pegylated asparaginase formulation with longer half-life. SC-PEG was given at 2,500 IU/m2 every 3 weeks, and pegaspargase was given at 2,500 IU/m2 every 2 weeks.
Either asparaginase product was given as part of a 4-week induction regimen (vincristine, prednisone, doxorubicin, and methotrexate), a 3-week intensification regimen (intrathecal chemotherapy with or without radiotherapy) for central nervous system disease, and a 27-week second consolidation regimen (mercaptopurine, methotrexate, and, in high-risk patients, doxorubicin).
SAA
The researchers observed significantly longer SAA with SC-PEG during induction but not after.
During induction, at 25 days after the first asparaginase dose, 88% of patients on SC-PEG and 17% of those on pegaspargase had SAA of at least 0.10 IU/mL (P less than .001). Post-induction, at week 25, 100% of patients in each group had a nadir SAA of at least 0.10 IU/mL.
“The high nadir serum asparaginase activity levels observed for both preparations suggest dosing strategies could be further optimized,” Dr. Vrooman noted.
Safety
There were no significant differences in adverse events between the SC-PEG and pegaspargase arms during or after induction.
Adverse events during induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (0% and 1%), grade 2 or higher pancreatitis (3% in both), grade 2 or higher thrombosis (3% and 9%), grade 4 hyperbilirubinemia (3% and 1%), grade 3 or higher bacterial infection (12% and 9%), and grade 3 or higher fungal infection (4% and 5%).
Adverse events after induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (17% and 14%), grade 2 or higher pancreatitis (15% in both), grade 2 or higher thrombosis (18% and 13%), grade 4 hyperbilirubinemia (4% and 3%), grade 3 or higher bacterial infection (12% and 15%), grade 3 or higher fungal infection (2% and 1%), grade 2 or higher bone fracture (3% and 8%), and grade 2 or higher osteonecrosis (3% and 4%).
Response and survival
The complete response rate was 95% (109/115) in the SC-PEG arm and 99% (114/115) in the pegaspargase arm. Rates of induction failure were 3% (n = 4) and 1% (n = 1), respectively, and rates of relapse were 3% (n = 5) and 8% (n = 10), respectively.
There were two induction deaths and two remission deaths in the SC-PEG arm but no induction or remission deaths in the pegaspargase arm.
The median follow-up was 4 years. The 4-year event-free survival rate was 87.7% with SC-PEG and 90.2% with pegaspargase (P = .78). The 4-year overall survival rate was 94.8% and 95.6%, respectively (P = .74).
In closing, Dr. Vrooman said these data suggest SC-PEG provides similar results as standard pegaspargase. She noted that these data informed the U.S. approval of SC-PEG for pediatric and young adult ALL.
This trial was sponsored by the Dana-Farber Cancer Institute in collaboration with Shire and the National Cancer Institute. Dr. Vrooman said she had no relationships to disclose.
SOURCE: Vrooman LM et al. ASCO 2019. Abstract 10006.
CHICAGO – Calaspargase pegol (SC-PEG) produces similar outcomes as standard pegaspargase in pediatric and young adult patients with newly diagnosed acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), according to a phase 2 trial.
Patients who received SC-PEG every 3 weeks had similar serum asparaginase activity (SAA), toxicities, and survival rates as patients who received standard pegaspargase every 2 weeks.
Lynda M. Vrooman, MD, of Dana-Farber Cancer Institute in Boston, presented these results at the annual meeting of the American Society of Clinical Oncology.
The trial (NCT01574274) enrolled 239 patients, 230 with ALL and 9 with LL. Most patients had B-cell (n = 207) disease. The patients’ median age was 5.2 years (range, 1.0-20.9 years).
“There were no differences in presenting features by randomization,” Dr. Vrooman noted.
The patients were randomized to receive pegaspargase (n = 120) or SC-PEG (n = 119), a pegylated asparaginase formulation with longer half-life. SC-PEG was given at 2,500 IU/m2 every 3 weeks, and pegaspargase was given at 2,500 IU/m2 every 2 weeks.
Either asparaginase product was given as part of a 4-week induction regimen (vincristine, prednisone, doxorubicin, and methotrexate), a 3-week intensification regimen (intrathecal chemotherapy with or without radiotherapy) for central nervous system disease, and a 27-week second consolidation regimen (mercaptopurine, methotrexate, and, in high-risk patients, doxorubicin).
SAA
The researchers observed significantly longer SAA with SC-PEG during induction but not after.
During induction, at 25 days after the first asparaginase dose, 88% of patients on SC-PEG and 17% of those on pegaspargase had SAA of at least 0.10 IU/mL (P less than .001). Post-induction, at week 25, 100% of patients in each group had a nadir SAA of at least 0.10 IU/mL.
“The high nadir serum asparaginase activity levels observed for both preparations suggest dosing strategies could be further optimized,” Dr. Vrooman noted.
Safety
There were no significant differences in adverse events between the SC-PEG and pegaspargase arms during or after induction.
Adverse events during induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (0% and 1%), grade 2 or higher pancreatitis (3% in both), grade 2 or higher thrombosis (3% and 9%), grade 4 hyperbilirubinemia (3% and 1%), grade 3 or higher bacterial infection (12% and 9%), and grade 3 or higher fungal infection (4% and 5%).
Adverse events after induction (in the SC-PEG and pegaspargase arms, respectively) included grade 2 or higher asparaginase allergy (17% and 14%), grade 2 or higher pancreatitis (15% in both), grade 2 or higher thrombosis (18% and 13%), grade 4 hyperbilirubinemia (4% and 3%), grade 3 or higher bacterial infection (12% and 15%), grade 3 or higher fungal infection (2% and 1%), grade 2 or higher bone fracture (3% and 8%), and grade 2 or higher osteonecrosis (3% and 4%).
Response and survival
The complete response rate was 95% (109/115) in the SC-PEG arm and 99% (114/115) in the pegaspargase arm. Rates of induction failure were 3% (n = 4) and 1% (n = 1), respectively, and rates of relapse were 3% (n = 5) and 8% (n = 10), respectively.
There were two induction deaths and two remission deaths in the SC-PEG arm but no induction or remission deaths in the pegaspargase arm.
The median follow-up was 4 years. The 4-year event-free survival rate was 87.7% with SC-PEG and 90.2% with pegaspargase (P = .78). The 4-year overall survival rate was 94.8% and 95.6%, respectively (P = .74).
In closing, Dr. Vrooman said these data suggest SC-PEG provides similar results as standard pegaspargase. She noted that these data informed the U.S. approval of SC-PEG for pediatric and young adult ALL.
This trial was sponsored by the Dana-Farber Cancer Institute in collaboration with Shire and the National Cancer Institute. Dr. Vrooman said she had no relationships to disclose.
SOURCE: Vrooman LM et al. ASCO 2019. Abstract 10006.
REPORTING FROM ASCO 2019
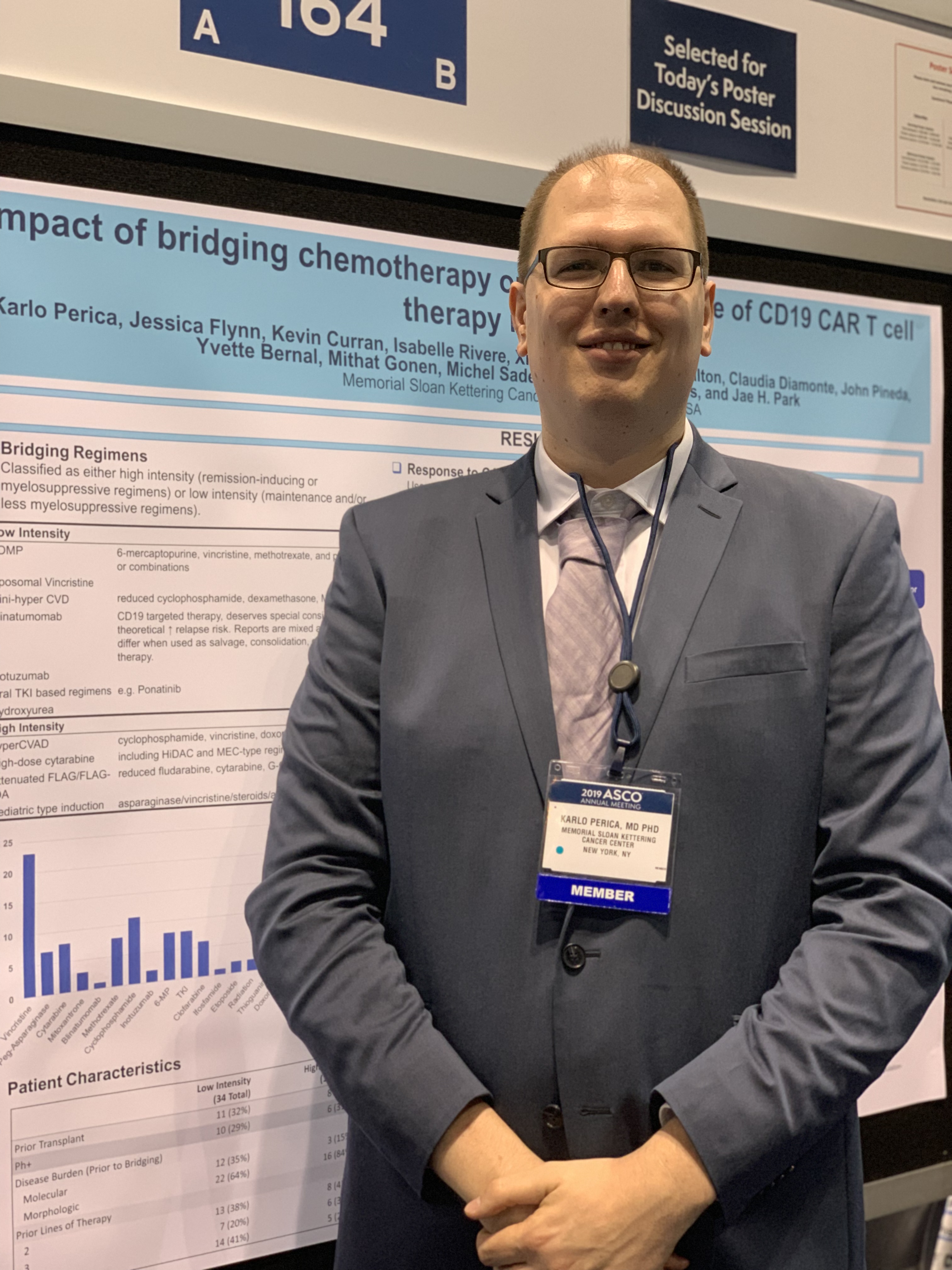
Low intensity bridging may be best path to CAR T in adult ALL
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
FROM ASCO 2019
Ribociclib plus endocrine therapy boosts survival of HR+/HER2- breast cancer
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis performed at 42 months of follow-up showed that the overall survival (OS) rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib (Kisqali) was 70%, compared with 46% for women randomized to endocrine therapy plus placebo.
The trial is the first study to evaluate a CDK4/6 inhibitor exclusively in premenopausal women, and the first to show a statistically significant improvement in overall survival with a CDK4/6 inhibitor in combination with endocrine therapy in patients with HR-positive, HER2-negative advanced breast cancer.
In a video interview at the American Society of Clinical Oncology annual meeting, Sara A. Hurvitz, MD, from the University of California Los Angeles Jonsson Comprehensive Cancer Center, describes the significance of the MONALEESA-7 findings and the potential for improving on the study results with other agents or combinations.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis.
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis performed at 42 months of follow-up showed that the overall survival (OS) rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib (Kisqali) was 70%, compared with 46% for women randomized to endocrine therapy plus placebo.
The trial is the first study to evaluate a CDK4/6 inhibitor exclusively in premenopausal women, and the first to show a statistically significant improvement in overall survival with a CDK4/6 inhibitor in combination with endocrine therapy in patients with HR-positive, HER2-negative advanced breast cancer.
In a video interview at the American Society of Clinical Oncology annual meeting, Sara A. Hurvitz, MD, from the University of California Los Angeles Jonsson Comprehensive Cancer Center, describes the significance of the MONALEESA-7 findings and the potential for improving on the study results with other agents or combinations.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis.
CHICAGO – Adding ribociclib to endocrine therapy significantly improved overall survival of premenopausal women with advanced hormone receptor positive, HER2-negative breast cancer, results of the randomized phase 3 MONALEESA-7 trial showed.
A landmark analysis performed at 42 months of follow-up showed that the overall survival (OS) rate for women randomized to receive endocrine therapy with either a nonsteroidal aromatase inhibitor (AI) or tamoxifen plus the cyclin-dependent kinase 4/6 (CDK4/6) inhibitor ribociclib (Kisqali) was 70%, compared with 46% for women randomized to endocrine therapy plus placebo.
The trial is the first study to evaluate a CDK4/6 inhibitor exclusively in premenopausal women, and the first to show a statistically significant improvement in overall survival with a CDK4/6 inhibitor in combination with endocrine therapy in patients with HR-positive, HER2-negative advanced breast cancer.
In a video interview at the American Society of Clinical Oncology annual meeting, Sara A. Hurvitz, MD, from the University of California Los Angeles Jonsson Comprehensive Cancer Center, describes the significance of the MONALEESA-7 findings and the potential for improving on the study results with other agents or combinations.
The MONALEESA-7 trial is supported by Novartis. Dr. Hurvitz reported travel and accommodation expenses from Novartis.
REPORTING FROM ASCO 2019
Pembro with or without chemo superior to EXTREME for advanced HNSCC
CHICAGO – Pembrolizumab with and without chemotherapy proved superior for overall survival compared with the EXTREME regimen when used first line in certain subgroups of patients with recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC), according to “practice-changing” final results from the randomized phase 3 KEYNOTE-048 study.
Compared with 300 patients randomized to receive the EXTREME regimen (a certuximab loading dose followed by carboplatin or cisplatin and 5-fluorouracil), 281 who received pembrolizumab plus chemotherapy (P+C) had superior overall survival (OS) with comparable safety–including both those with programmed death-Ligand 1 (PD-L1) combined positive score (CPS) of 20 or greater (median 14.7 vs 11.0 months; hazard ratio, 0.60) and with CPS of 1 or greater (median, 13.6 vs. 10.4 months; HR, 0.65), Danny Rischin, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The differences were highly statistically significant, said Dr. Rischin, a professor and director of the Division of Cancer Medicine and head of the Department of Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia.
“And this benefit in overall survival in CPS greater than or equal to 20 and greater than or equal to 1 appeared to be present across all the subgroups that we looked at,” he added.
The response rates did not differ between P+C and EXTREME groups, but the median duration of response was significantly greater with P+C vs. EXTREME in both the CPS of 20 or greater and 1 or greater (7.1 vs. 4.2 months and 6.7 vs. 4.3 months, respectively).
Additionally, the final results of the study showed an OS benefit with P+C vs. EXTREME in the total population (13.0 vs. 10.7 months; HR, 0.72), Dr. Rischin said.
The difference between the groups with respect to progression-free survival (PFS), however, was not statistically significant and did not reach the superiority threshold, he noted.
In the 301 patients who received pembrolizumab alone, OS was superior in the CPS 20 or greater and 1 or greater populations (median, 14.8 vs. 10.7 months; HR, 0.58 and 12.4 vs. 10.3 months; HR, 0.74, respectively), compared with EXTREME, but was noninferior in the total population (median 11.5 vs. 10.7 months; HR, 0.83), and safety was favorable .
Again, PFS did not differ between the groups (median, 2.3 vs. 5.2 months; HR, 1.34), and while the overall response rates did not differ significantly, the median duration of response was substantially longer with pembrolizumab at 22.6 vs. 4.5 months with EXTREME, he said.
Study participants had locally incurable R/M HNSCC and no prior systemic therapy in the R/M setting. Those in he P+C arm received pembrolizumab at 200 mg plus 6 cycles of cisplatin at 100 mg/m2 or carboplatin AUC 5, and 5-fluorouracil at a dose of 1000 mg/m2/day for 4 days every 3 weeks; those in the pembrolizumab alone arm received 200 mg every 3 weeks for up to 35 cycles, and those in the EXTREME arm received certuximab at a 400 mg/m2 loading dose followed by 250 mg/m2 weekly with carboplatin AUC 5 or cisplatin at 100 mg/m2, and 5-FU at 1000 mg/m2/day for 4 days for 6 cycles.
“The data from KEYNOTE-048 support pembrolizumab plus platinum-based chemotherapy and pembrolizumab monotherapy as new standard of care monotherapies for recurrent/metastatic head and neck squamous cell carcinoma,” he concluded.
Discussant Vanita Noronha, MD, a professor in the Department of Medical Oncology at Tata Memorial Hospital in Mumbai, India, said that while the findings are practice changing, they also raise a number of questions, such as which patients should get pembrolizumab and which should get P+C, why there is a differential effect of pembrolizumab based on PD-L1 by CPS–and what about those with CPS of 0 or 1-20, and why the response rates and PFS rates were not improved in the pembrolizumab groups.
Other important questions include whether there are predictive biomarkers for response, and whether sequential therapy would be of benefit, she added.
While these and other questions remain to be addressed, the KEYNOTE-048 findings have implications for practice going forward; based on the current data, her approach to treating patients with R/M HNSCC not amenable to radical therapy is to treat with pembrolizumab alone in those with disease-free interval of 6 months or less, she said.
For those with disease-free interval greater than 6 months and good performance status who have controlled comorbidities, are platinum eligible, and for whom the treatment is reimbursable/affordable, treatment depends on symptom severity; she would treat those with mild/moderate symptoms and CPS of 20 or greater with pembrolizumab alone, those with CPS of 1 or greater with P+C or pembrolizumab alone, and those with CPS of 0 or unknown CPS with EXTREME or a similar regimen or with P+C, and she would treat those with severe symptoms with P+C.
“If the patient were a bit borderline, had multiple comorbidities, could not receive platinum, or had financial constraints, I would treat the patient with singe-agent intravenous chemotherapy or with oral metronomic chemotherapy, single-agent targeted therapy or with best supportive care,” she said.
Dr. Rischin has received research funding from Amgen, Bristol-Myers Squibb, Genentech/Roche, GSK, Merck, and Regeneron. Dr. Noronha has received research funding (to her institution) from Amgen,and Sanofi Aventis.
SOURCE: D Rischin et al., ASCO 2019: Abstract 6000.
CHICAGO – Pembrolizumab with and without chemotherapy proved superior for overall survival compared with the EXTREME regimen when used first line in certain subgroups of patients with recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC), according to “practice-changing” final results from the randomized phase 3 KEYNOTE-048 study.
Compared with 300 patients randomized to receive the EXTREME regimen (a certuximab loading dose followed by carboplatin or cisplatin and 5-fluorouracil), 281 who received pembrolizumab plus chemotherapy (P+C) had superior overall survival (OS) with comparable safety–including both those with programmed death-Ligand 1 (PD-L1) combined positive score (CPS) of 20 or greater (median 14.7 vs 11.0 months; hazard ratio, 0.60) and with CPS of 1 or greater (median, 13.6 vs. 10.4 months; HR, 0.65), Danny Rischin, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The differences were highly statistically significant, said Dr. Rischin, a professor and director of the Division of Cancer Medicine and head of the Department of Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia.
“And this benefit in overall survival in CPS greater than or equal to 20 and greater than or equal to 1 appeared to be present across all the subgroups that we looked at,” he added.
The response rates did not differ between P+C and EXTREME groups, but the median duration of response was significantly greater with P+C vs. EXTREME in both the CPS of 20 or greater and 1 or greater (7.1 vs. 4.2 months and 6.7 vs. 4.3 months, respectively).
Additionally, the final results of the study showed an OS benefit with P+C vs. EXTREME in the total population (13.0 vs. 10.7 months; HR, 0.72), Dr. Rischin said.
The difference between the groups with respect to progression-free survival (PFS), however, was not statistically significant and did not reach the superiority threshold, he noted.
In the 301 patients who received pembrolizumab alone, OS was superior in the CPS 20 or greater and 1 or greater populations (median, 14.8 vs. 10.7 months; HR, 0.58 and 12.4 vs. 10.3 months; HR, 0.74, respectively), compared with EXTREME, but was noninferior in the total population (median 11.5 vs. 10.7 months; HR, 0.83), and safety was favorable .
Again, PFS did not differ between the groups (median, 2.3 vs. 5.2 months; HR, 1.34), and while the overall response rates did not differ significantly, the median duration of response was substantially longer with pembrolizumab at 22.6 vs. 4.5 months with EXTREME, he said.
Study participants had locally incurable R/M HNSCC and no prior systemic therapy in the R/M setting. Those in he P+C arm received pembrolizumab at 200 mg plus 6 cycles of cisplatin at 100 mg/m2 or carboplatin AUC 5, and 5-fluorouracil at a dose of 1000 mg/m2/day for 4 days every 3 weeks; those in the pembrolizumab alone arm received 200 mg every 3 weeks for up to 35 cycles, and those in the EXTREME arm received certuximab at a 400 mg/m2 loading dose followed by 250 mg/m2 weekly with carboplatin AUC 5 or cisplatin at 100 mg/m2, and 5-FU at 1000 mg/m2/day for 4 days for 6 cycles.
“The data from KEYNOTE-048 support pembrolizumab plus platinum-based chemotherapy and pembrolizumab monotherapy as new standard of care monotherapies for recurrent/metastatic head and neck squamous cell carcinoma,” he concluded.
Discussant Vanita Noronha, MD, a professor in the Department of Medical Oncology at Tata Memorial Hospital in Mumbai, India, said that while the findings are practice changing, they also raise a number of questions, such as which patients should get pembrolizumab and which should get P+C, why there is a differential effect of pembrolizumab based on PD-L1 by CPS–and what about those with CPS of 0 or 1-20, and why the response rates and PFS rates were not improved in the pembrolizumab groups.
Other important questions include whether there are predictive biomarkers for response, and whether sequential therapy would be of benefit, she added.
While these and other questions remain to be addressed, the KEYNOTE-048 findings have implications for practice going forward; based on the current data, her approach to treating patients with R/M HNSCC not amenable to radical therapy is to treat with pembrolizumab alone in those with disease-free interval of 6 months or less, she said.
For those with disease-free interval greater than 6 months and good performance status who have controlled comorbidities, are platinum eligible, and for whom the treatment is reimbursable/affordable, treatment depends on symptom severity; she would treat those with mild/moderate symptoms and CPS of 20 or greater with pembrolizumab alone, those with CPS of 1 or greater with P+C or pembrolizumab alone, and those with CPS of 0 or unknown CPS with EXTREME or a similar regimen or with P+C, and she would treat those with severe symptoms with P+C.
“If the patient were a bit borderline, had multiple comorbidities, could not receive platinum, or had financial constraints, I would treat the patient with singe-agent intravenous chemotherapy or with oral metronomic chemotherapy, single-agent targeted therapy or with best supportive care,” she said.
Dr. Rischin has received research funding from Amgen, Bristol-Myers Squibb, Genentech/Roche, GSK, Merck, and Regeneron. Dr. Noronha has received research funding (to her institution) from Amgen,and Sanofi Aventis.
SOURCE: D Rischin et al., ASCO 2019: Abstract 6000.
CHICAGO – Pembrolizumab with and without chemotherapy proved superior for overall survival compared with the EXTREME regimen when used first line in certain subgroups of patients with recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC), according to “practice-changing” final results from the randomized phase 3 KEYNOTE-048 study.
Compared with 300 patients randomized to receive the EXTREME regimen (a certuximab loading dose followed by carboplatin or cisplatin and 5-fluorouracil), 281 who received pembrolizumab plus chemotherapy (P+C) had superior overall survival (OS) with comparable safety–including both those with programmed death-Ligand 1 (PD-L1) combined positive score (CPS) of 20 or greater (median 14.7 vs 11.0 months; hazard ratio, 0.60) and with CPS of 1 or greater (median, 13.6 vs. 10.4 months; HR, 0.65), Danny Rischin, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The differences were highly statistically significant, said Dr. Rischin, a professor and director of the Division of Cancer Medicine and head of the Department of Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia.
“And this benefit in overall survival in CPS greater than or equal to 20 and greater than or equal to 1 appeared to be present across all the subgroups that we looked at,” he added.
The response rates did not differ between P+C and EXTREME groups, but the median duration of response was significantly greater with P+C vs. EXTREME in both the CPS of 20 or greater and 1 or greater (7.1 vs. 4.2 months and 6.7 vs. 4.3 months, respectively).
Additionally, the final results of the study showed an OS benefit with P+C vs. EXTREME in the total population (13.0 vs. 10.7 months; HR, 0.72), Dr. Rischin said.
The difference between the groups with respect to progression-free survival (PFS), however, was not statistically significant and did not reach the superiority threshold, he noted.
In the 301 patients who received pembrolizumab alone, OS was superior in the CPS 20 or greater and 1 or greater populations (median, 14.8 vs. 10.7 months; HR, 0.58 and 12.4 vs. 10.3 months; HR, 0.74, respectively), compared with EXTREME, but was noninferior in the total population (median 11.5 vs. 10.7 months; HR, 0.83), and safety was favorable .
Again, PFS did not differ between the groups (median, 2.3 vs. 5.2 months; HR, 1.34), and while the overall response rates did not differ significantly, the median duration of response was substantially longer with pembrolizumab at 22.6 vs. 4.5 months with EXTREME, he said.
Study participants had locally incurable R/M HNSCC and no prior systemic therapy in the R/M setting. Those in he P+C arm received pembrolizumab at 200 mg plus 6 cycles of cisplatin at 100 mg/m2 or carboplatin AUC 5, and 5-fluorouracil at a dose of 1000 mg/m2/day for 4 days every 3 weeks; those in the pembrolizumab alone arm received 200 mg every 3 weeks for up to 35 cycles, and those in the EXTREME arm received certuximab at a 400 mg/m2 loading dose followed by 250 mg/m2 weekly with carboplatin AUC 5 or cisplatin at 100 mg/m2, and 5-FU at 1000 mg/m2/day for 4 days for 6 cycles.
“The data from KEYNOTE-048 support pembrolizumab plus platinum-based chemotherapy and pembrolizumab monotherapy as new standard of care monotherapies for recurrent/metastatic head and neck squamous cell carcinoma,” he concluded.
Discussant Vanita Noronha, MD, a professor in the Department of Medical Oncology at Tata Memorial Hospital in Mumbai, India, said that while the findings are practice changing, they also raise a number of questions, such as which patients should get pembrolizumab and which should get P+C, why there is a differential effect of pembrolizumab based on PD-L1 by CPS–and what about those with CPS of 0 or 1-20, and why the response rates and PFS rates were not improved in the pembrolizumab groups.
Other important questions include whether there are predictive biomarkers for response, and whether sequential therapy would be of benefit, she added.
While these and other questions remain to be addressed, the KEYNOTE-048 findings have implications for practice going forward; based on the current data, her approach to treating patients with R/M HNSCC not amenable to radical therapy is to treat with pembrolizumab alone in those with disease-free interval of 6 months or less, she said.
For those with disease-free interval greater than 6 months and good performance status who have controlled comorbidities, are platinum eligible, and for whom the treatment is reimbursable/affordable, treatment depends on symptom severity; she would treat those with mild/moderate symptoms and CPS of 20 or greater with pembrolizumab alone, those with CPS of 1 or greater with P+C or pembrolizumab alone, and those with CPS of 0 or unknown CPS with EXTREME or a similar regimen or with P+C, and she would treat those with severe symptoms with P+C.
“If the patient were a bit borderline, had multiple comorbidities, could not receive platinum, or had financial constraints, I would treat the patient with singe-agent intravenous chemotherapy or with oral metronomic chemotherapy, single-agent targeted therapy or with best supportive care,” she said.
Dr. Rischin has received research funding from Amgen, Bristol-Myers Squibb, Genentech/Roche, GSK, Merck, and Regeneron. Dr. Noronha has received research funding (to her institution) from Amgen,and Sanofi Aventis.
SOURCE: D Rischin et al., ASCO 2019: Abstract 6000.
REPORTING FROM ASCO 2019
Short-term ADT improves radiation salvage after prostatectomy
CHICAGO – Adding short-term androgen deprivation therapy (ADT) to radiotherapy as salvage treatment after radical prostatectomy was associated with significantly better metastasis-free survival at nearly 10 years compared with salvage radiation alone, long-term results of a randomized phase 3 trial show.
After a median follow-up of 112 months (9.3 years), the metastasis-free survival (MFS) rate for 369 patients assigned to receive salvage radiation and short-term goserelin was 75%, compared with 69% for 374 patients randomized to radiation alone (P = .034), reported Nicolas Magné, MD, from Jean Monnet Saint Etienne University in Saint-Priest en Jarez, France.
“We can conclude and do believe that short ADT, only two injections at 3-month intervals, could increase MFS at 10 years compared to radiation alone in patients with rising PSA after initial prostatectomy,“ he said at the annual meeting of the American Society of Clinical Oncology.
There was no significant difference, however, in the secondary endpoint of overall survival at 10 years.
Dr. Magné and co-investigators in the GETUG-AFU 16 trial had previously reported that after a median follow-up of 5.3 years, patients assigned to radiation plus goserelin were significantly more likely to be free of biochemical or clinical progression at 5 years than patients assigned to radiotherapy alone (80% vs, 62%, hazard ratio [HR] 0.50, P less than .0001).
The open-label trial enrolled men 18 or older from 43 French centers who had been treated for a histologically confirmed adenocarcinoma of the prostate but had not received prior androgen deprivation therapy (ADT) or pelvic radiation. The patients had either stage pT2 or pT3 cancers, or stage pT4a with invasive disease limited to the bladder neck. The patients all had biochemical failure, defined as a rising prostate-specific antigen (PSA) of 0.2 to 2.0 mcg/L following radical prostatectomy, with no clinically evident disease.
The patients were randomly assigned to receive standard salvage radiotherapy either alone or with hormonal therapy. Randomization was stratified by investigational site, radiotherapy modality, and prognosis.
Radiotherapy consisted of either 3-D conformal radiotherapy or intensity modulated radiotherapy, delivered in 66 Gy doses divided into 33 fractions of 2 Gy each 5 days a week for 7 weeks.
Patients assigned to hormonal therapy in addition to radiation received one subcutaneous injection of goserelin 10.8 mg on the first day of radiation, and a second injection 3 months later.
Progression-free survival (PFS), the primary endpoint, was significantly better with the combination than with radiation alone for both low-risk patients (HR 0.47, 95% confidence interval [CI] 0.28-0.80), and high-risk patients (HR 0.56, CI 0.44-0.83).
As noted before, metastasis-free survival was also significantly better in the combination arm ( HR, 0.73, P = .034) at 10 years.
Invited discussant Daniel Spratt, MD, from the University of Michigan in Ann Arbor, commented that the study results “do show, just like they did in 2016, that bicochemical control is improved, which is linked to their primary endpoint of PFS, but I always caution that this alone will always be improved with testosterone suppression.”
He noted that if you give ADT to patients with low-risk prostate cancer “that we don’t usually even treat today,” adding hormonal therapy will produce a nearly identical improvement in biochemical control, suggesting more of a signal than a clinical benefit.
The improvement in MFS, however, is indeed a clinical benefit, “but it is a small difference, and one thing to note is that when you give these patients about 6 months of hormonal therapy, depending on the age of the patient, it can be about 6 months until they recover testosterone, and at their median follow-up, you can see that the delay in MFS, which is usually the trigger to start hormone therapy, is about 12 months. So it’s important when you counsel these patients that [for] about potentially 6 months to a year of symptoms you may delay the need for hormone therapy by about 12 months,” he said.
The study was supported by UNICANCER and AstraZeneca. Dr. Magné reported no relevant disclosures. Dr. Spratt reported amconsulting or advisory role with Blue Earth Diagnostics and Janssen Oncology.
SOURCE: Magn é D et al. ASCO 2019. Abstract 5001.
CHICAGO – Adding short-term androgen deprivation therapy (ADT) to radiotherapy as salvage treatment after radical prostatectomy was associated with significantly better metastasis-free survival at nearly 10 years compared with salvage radiation alone, long-term results of a randomized phase 3 trial show.
After a median follow-up of 112 months (9.3 years), the metastasis-free survival (MFS) rate for 369 patients assigned to receive salvage radiation and short-term goserelin was 75%, compared with 69% for 374 patients randomized to radiation alone (P = .034), reported Nicolas Magné, MD, from Jean Monnet Saint Etienne University in Saint-Priest en Jarez, France.
“We can conclude and do believe that short ADT, only two injections at 3-month intervals, could increase MFS at 10 years compared to radiation alone in patients with rising PSA after initial prostatectomy,“ he said at the annual meeting of the American Society of Clinical Oncology.
There was no significant difference, however, in the secondary endpoint of overall survival at 10 years.
Dr. Magné and co-investigators in the GETUG-AFU 16 trial had previously reported that after a median follow-up of 5.3 years, patients assigned to radiation plus goserelin were significantly more likely to be free of biochemical or clinical progression at 5 years than patients assigned to radiotherapy alone (80% vs, 62%, hazard ratio [HR] 0.50, P less than .0001).
The open-label trial enrolled men 18 or older from 43 French centers who had been treated for a histologically confirmed adenocarcinoma of the prostate but had not received prior androgen deprivation therapy (ADT) or pelvic radiation. The patients had either stage pT2 or pT3 cancers, or stage pT4a with invasive disease limited to the bladder neck. The patients all had biochemical failure, defined as a rising prostate-specific antigen (PSA) of 0.2 to 2.0 mcg/L following radical prostatectomy, with no clinically evident disease.
The patients were randomly assigned to receive standard salvage radiotherapy either alone or with hormonal therapy. Randomization was stratified by investigational site, radiotherapy modality, and prognosis.
Radiotherapy consisted of either 3-D conformal radiotherapy or intensity modulated radiotherapy, delivered in 66 Gy doses divided into 33 fractions of 2 Gy each 5 days a week for 7 weeks.
Patients assigned to hormonal therapy in addition to radiation received one subcutaneous injection of goserelin 10.8 mg on the first day of radiation, and a second injection 3 months later.
Progression-free survival (PFS), the primary endpoint, was significantly better with the combination than with radiation alone for both low-risk patients (HR 0.47, 95% confidence interval [CI] 0.28-0.80), and high-risk patients (HR 0.56, CI 0.44-0.83).
As noted before, metastasis-free survival was also significantly better in the combination arm ( HR, 0.73, P = .034) at 10 years.
Invited discussant Daniel Spratt, MD, from the University of Michigan in Ann Arbor, commented that the study results “do show, just like they did in 2016, that bicochemical control is improved, which is linked to their primary endpoint of PFS, but I always caution that this alone will always be improved with testosterone suppression.”
He noted that if you give ADT to patients with low-risk prostate cancer “that we don’t usually even treat today,” adding hormonal therapy will produce a nearly identical improvement in biochemical control, suggesting more of a signal than a clinical benefit.
The improvement in MFS, however, is indeed a clinical benefit, “but it is a small difference, and one thing to note is that when you give these patients about 6 months of hormonal therapy, depending on the age of the patient, it can be about 6 months until they recover testosterone, and at their median follow-up, you can see that the delay in MFS, which is usually the trigger to start hormone therapy, is about 12 months. So it’s important when you counsel these patients that [for] about potentially 6 months to a year of symptoms you may delay the need for hormone therapy by about 12 months,” he said.
The study was supported by UNICANCER and AstraZeneca. Dr. Magné reported no relevant disclosures. Dr. Spratt reported amconsulting or advisory role with Blue Earth Diagnostics and Janssen Oncology.
SOURCE: Magn é D et al. ASCO 2019. Abstract 5001.
CHICAGO – Adding short-term androgen deprivation therapy (ADT) to radiotherapy as salvage treatment after radical prostatectomy was associated with significantly better metastasis-free survival at nearly 10 years compared with salvage radiation alone, long-term results of a randomized phase 3 trial show.
After a median follow-up of 112 months (9.3 years), the metastasis-free survival (MFS) rate for 369 patients assigned to receive salvage radiation and short-term goserelin was 75%, compared with 69% for 374 patients randomized to radiation alone (P = .034), reported Nicolas Magné, MD, from Jean Monnet Saint Etienne University in Saint-Priest en Jarez, France.
“We can conclude and do believe that short ADT, only two injections at 3-month intervals, could increase MFS at 10 years compared to radiation alone in patients with rising PSA after initial prostatectomy,“ he said at the annual meeting of the American Society of Clinical Oncology.
There was no significant difference, however, in the secondary endpoint of overall survival at 10 years.
Dr. Magné and co-investigators in the GETUG-AFU 16 trial had previously reported that after a median follow-up of 5.3 years, patients assigned to radiation plus goserelin were significantly more likely to be free of biochemical or clinical progression at 5 years than patients assigned to radiotherapy alone (80% vs, 62%, hazard ratio [HR] 0.50, P less than .0001).
The open-label trial enrolled men 18 or older from 43 French centers who had been treated for a histologically confirmed adenocarcinoma of the prostate but had not received prior androgen deprivation therapy (ADT) or pelvic radiation. The patients had either stage pT2 or pT3 cancers, or stage pT4a with invasive disease limited to the bladder neck. The patients all had biochemical failure, defined as a rising prostate-specific antigen (PSA) of 0.2 to 2.0 mcg/L following radical prostatectomy, with no clinically evident disease.
The patients were randomly assigned to receive standard salvage radiotherapy either alone or with hormonal therapy. Randomization was stratified by investigational site, radiotherapy modality, and prognosis.
Radiotherapy consisted of either 3-D conformal radiotherapy or intensity modulated radiotherapy, delivered in 66 Gy doses divided into 33 fractions of 2 Gy each 5 days a week for 7 weeks.
Patients assigned to hormonal therapy in addition to radiation received one subcutaneous injection of goserelin 10.8 mg on the first day of radiation, and a second injection 3 months later.
Progression-free survival (PFS), the primary endpoint, was significantly better with the combination than with radiation alone for both low-risk patients (HR 0.47, 95% confidence interval [CI] 0.28-0.80), and high-risk patients (HR 0.56, CI 0.44-0.83).
As noted before, metastasis-free survival was also significantly better in the combination arm ( HR, 0.73, P = .034) at 10 years.
Invited discussant Daniel Spratt, MD, from the University of Michigan in Ann Arbor, commented that the study results “do show, just like they did in 2016, that bicochemical control is improved, which is linked to their primary endpoint of PFS, but I always caution that this alone will always be improved with testosterone suppression.”
He noted that if you give ADT to patients with low-risk prostate cancer “that we don’t usually even treat today,” adding hormonal therapy will produce a nearly identical improvement in biochemical control, suggesting more of a signal than a clinical benefit.
The improvement in MFS, however, is indeed a clinical benefit, “but it is a small difference, and one thing to note is that when you give these patients about 6 months of hormonal therapy, depending on the age of the patient, it can be about 6 months until they recover testosterone, and at their median follow-up, you can see that the delay in MFS, which is usually the trigger to start hormone therapy, is about 12 months. So it’s important when you counsel these patients that [for] about potentially 6 months to a year of symptoms you may delay the need for hormone therapy by about 12 months,” he said.
The study was supported by UNICANCER and AstraZeneca. Dr. Magné reported no relevant disclosures. Dr. Spratt reported amconsulting or advisory role with Blue Earth Diagnostics and Janssen Oncology.
SOURCE: Magn é D et al. ASCO 2019. Abstract 5001.
REPORTING FROM ASCO 2019
Antibodies may have role in ‘TKI world’ of EGFR-mutant NSCLC
CHICAGO – While tyrosine kinase inhibitors (TKIs) have long dominated treatment approaches for EGFR-driven advanced non-small cell lung cancer, a few newer antibodies are showing early promise as potential new strategies to use after progression, recent reports show.
Both JNJ-372, an EGFR and MET bispecific antibody, and U3-1402, a HER3-directed antibody-drug conjugate (ADC), demonstrated manageable safety profiles and preliminary antitumor activity in phase 1 study results presented here at the annual meeting of the American Society of Clinical Oncology.
“There is definitely a role to play for antibodies in the TKI world,” said Jessica Ruth Bauman, MD, of Fox Chase Cancer Center, Philadelphia, Pa., a discussant on both abstracts.
These two antibodies harness new mechanisms of action that are not specific to a resistance mechanism, which may lead to broad applicability, according to Dr. Bauman.
“Mechanisms of acquired resistance have been the Achilles heel of EGFR TKI treatment,” she said.
The JNJ-372 bispecific antibody has preclinical data consistent with several proposed mechanisms of action, including inhibition of EGFR and cMet signaling, receptor degradation, and antibody-dependent cellular cytotoxicity, said investigator Eric B. Haura, MD, of H. Lee Moffitt Cancer Center & Research Institute, Tampa, Fla.
In the phase 1 study, which included patients with diverse EGFR mutations, 32 out of 108 patients (30%) had a best response of partial response (PR) after treatment with JNJ-372, Dr. Haura reported in an oral abstract presentation.
Responses were seen in patients with mutations that represent areas of high unmet need, including those with EGFR C797S-mediated or cMet-mediated resistance to the third-generation TKI osimertinib, and those with TKI-naïve EGFR exon 20 insertions, he emphasized in his presentation.
The safety profile was “manageable” and consistent with EGFR inhibition, he said, with a low (9%) rate of grade 3 or greater toxicities and frequent infusion-related reactions, mostly after the first dose.
Enrollment of patients with high unmet need is ongoing, according to Dr. Haura.
U3-1402, the antibody-drug conjugate that may have a place in the TKI world, consists of a fully human HER3-targeted antibody linked to a topoisomerase I inhibitor payload.
“Targeting HER3 with U3-1402 may be a practical approach to treat EGFR-mutant NSCLC with diverse mechanisms of resistance to EGFR TKIs,” said investigator Pasi A. Jänne, MD, PhD, of Dana-Farber Cancer Institute, Boston, Mass.
That’s because mechanisms of resistance to TKIs in EGFR-mutant NSCLC are turning out to be so diverse, that trying to combat each individual resistance mechanism is likely “impractical,” Dr. Jänne said.
Targeting HER3, the perhaps lesser-known of the four members of the EGFR tyrosine kinase family, may address multiple resistance mechanisms, and 57% to 67% of EGFR-mutant NSCLCs have at least some level of HER3 expression, according to the presenter.
In the phase 1 study data reported at the meeting, the response rate following U3-1402 treatment was about 31%, or 5 out of 16 patients, including 4 confirmed partial responses. Most treatment-emergent adverse events were grade 1 or 2, and only one patient discontinued due to an adverse event, according to Dr. Jänne, who said the study is ongoing.
Taken together, findings for U3-1402 and JNJ-372 show that there may be room for other approaches beyond TKIs to address the need for new therapies to overcome resistance, Dr. Bauman said in her commentary on these studies.
“Additional research will enable us to determine who will benefit from these compounds, what biomarkers are predictive, and novel combinations to consider,” she added.
Dr. Bauman reported a consulting or advisory role with Pfizer. Dr. Haura provided disclosures related to Bristol-Myers Squibb; Janssen Oncology, Boehringer Ingelheim, FORMA Therapeutics, Ignyta, Janssen, Lilly, and Ventana, plus a patent pending on technology related to kinase inhibitor sensitivity biomarkers. Dr. Jänne reported disclosures related to Gatekeeper Pharmaceuticals, Loxo, Araxes Pharma, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Lilly, and others.
SOURCE: Haura EB, et al. ASCO 2019. Abstract 9009, Jänne PA, et al. ASCO 2019. Abstract 9010.
CHICAGO – While tyrosine kinase inhibitors (TKIs) have long dominated treatment approaches for EGFR-driven advanced non-small cell lung cancer, a few newer antibodies are showing early promise as potential new strategies to use after progression, recent reports show.
Both JNJ-372, an EGFR and MET bispecific antibody, and U3-1402, a HER3-directed antibody-drug conjugate (ADC), demonstrated manageable safety profiles and preliminary antitumor activity in phase 1 study results presented here at the annual meeting of the American Society of Clinical Oncology.
“There is definitely a role to play for antibodies in the TKI world,” said Jessica Ruth Bauman, MD, of Fox Chase Cancer Center, Philadelphia, Pa., a discussant on both abstracts.
These two antibodies harness new mechanisms of action that are not specific to a resistance mechanism, which may lead to broad applicability, according to Dr. Bauman.
“Mechanisms of acquired resistance have been the Achilles heel of EGFR TKI treatment,” she said.
The JNJ-372 bispecific antibody has preclinical data consistent with several proposed mechanisms of action, including inhibition of EGFR and cMet signaling, receptor degradation, and antibody-dependent cellular cytotoxicity, said investigator Eric B. Haura, MD, of H. Lee Moffitt Cancer Center & Research Institute, Tampa, Fla.
In the phase 1 study, which included patients with diverse EGFR mutations, 32 out of 108 patients (30%) had a best response of partial response (PR) after treatment with JNJ-372, Dr. Haura reported in an oral abstract presentation.
Responses were seen in patients with mutations that represent areas of high unmet need, including those with EGFR C797S-mediated or cMet-mediated resistance to the third-generation TKI osimertinib, and those with TKI-naïve EGFR exon 20 insertions, he emphasized in his presentation.
The safety profile was “manageable” and consistent with EGFR inhibition, he said, with a low (9%) rate of grade 3 or greater toxicities and frequent infusion-related reactions, mostly after the first dose.
Enrollment of patients with high unmet need is ongoing, according to Dr. Haura.
U3-1402, the antibody-drug conjugate that may have a place in the TKI world, consists of a fully human HER3-targeted antibody linked to a topoisomerase I inhibitor payload.
“Targeting HER3 with U3-1402 may be a practical approach to treat EGFR-mutant NSCLC with diverse mechanisms of resistance to EGFR TKIs,” said investigator Pasi A. Jänne, MD, PhD, of Dana-Farber Cancer Institute, Boston, Mass.
That’s because mechanisms of resistance to TKIs in EGFR-mutant NSCLC are turning out to be so diverse, that trying to combat each individual resistance mechanism is likely “impractical,” Dr. Jänne said.
Targeting HER3, the perhaps lesser-known of the four members of the EGFR tyrosine kinase family, may address multiple resistance mechanisms, and 57% to 67% of EGFR-mutant NSCLCs have at least some level of HER3 expression, according to the presenter.
In the phase 1 study data reported at the meeting, the response rate following U3-1402 treatment was about 31%, or 5 out of 16 patients, including 4 confirmed partial responses. Most treatment-emergent adverse events were grade 1 or 2, and only one patient discontinued due to an adverse event, according to Dr. Jänne, who said the study is ongoing.
Taken together, findings for U3-1402 and JNJ-372 show that there may be room for other approaches beyond TKIs to address the need for new therapies to overcome resistance, Dr. Bauman said in her commentary on these studies.
“Additional research will enable us to determine who will benefit from these compounds, what biomarkers are predictive, and novel combinations to consider,” she added.
Dr. Bauman reported a consulting or advisory role with Pfizer. Dr. Haura provided disclosures related to Bristol-Myers Squibb; Janssen Oncology, Boehringer Ingelheim, FORMA Therapeutics, Ignyta, Janssen, Lilly, and Ventana, plus a patent pending on technology related to kinase inhibitor sensitivity biomarkers. Dr. Jänne reported disclosures related to Gatekeeper Pharmaceuticals, Loxo, Araxes Pharma, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Lilly, and others.
SOURCE: Haura EB, et al. ASCO 2019. Abstract 9009, Jänne PA, et al. ASCO 2019. Abstract 9010.
CHICAGO – While tyrosine kinase inhibitors (TKIs) have long dominated treatment approaches for EGFR-driven advanced non-small cell lung cancer, a few newer antibodies are showing early promise as potential new strategies to use after progression, recent reports show.
Both JNJ-372, an EGFR and MET bispecific antibody, and U3-1402, a HER3-directed antibody-drug conjugate (ADC), demonstrated manageable safety profiles and preliminary antitumor activity in phase 1 study results presented here at the annual meeting of the American Society of Clinical Oncology.
“There is definitely a role to play for antibodies in the TKI world,” said Jessica Ruth Bauman, MD, of Fox Chase Cancer Center, Philadelphia, Pa., a discussant on both abstracts.
These two antibodies harness new mechanisms of action that are not specific to a resistance mechanism, which may lead to broad applicability, according to Dr. Bauman.
“Mechanisms of acquired resistance have been the Achilles heel of EGFR TKI treatment,” she said.
The JNJ-372 bispecific antibody has preclinical data consistent with several proposed mechanisms of action, including inhibition of EGFR and cMet signaling, receptor degradation, and antibody-dependent cellular cytotoxicity, said investigator Eric B. Haura, MD, of H. Lee Moffitt Cancer Center & Research Institute, Tampa, Fla.
In the phase 1 study, which included patients with diverse EGFR mutations, 32 out of 108 patients (30%) had a best response of partial response (PR) after treatment with JNJ-372, Dr. Haura reported in an oral abstract presentation.
Responses were seen in patients with mutations that represent areas of high unmet need, including those with EGFR C797S-mediated or cMet-mediated resistance to the third-generation TKI osimertinib, and those with TKI-naïve EGFR exon 20 insertions, he emphasized in his presentation.
The safety profile was “manageable” and consistent with EGFR inhibition, he said, with a low (9%) rate of grade 3 or greater toxicities and frequent infusion-related reactions, mostly after the first dose.
Enrollment of patients with high unmet need is ongoing, according to Dr. Haura.
U3-1402, the antibody-drug conjugate that may have a place in the TKI world, consists of a fully human HER3-targeted antibody linked to a topoisomerase I inhibitor payload.
“Targeting HER3 with U3-1402 may be a practical approach to treat EGFR-mutant NSCLC with diverse mechanisms of resistance to EGFR TKIs,” said investigator Pasi A. Jänne, MD, PhD, of Dana-Farber Cancer Institute, Boston, Mass.
That’s because mechanisms of resistance to TKIs in EGFR-mutant NSCLC are turning out to be so diverse, that trying to combat each individual resistance mechanism is likely “impractical,” Dr. Jänne said.
Targeting HER3, the perhaps lesser-known of the four members of the EGFR tyrosine kinase family, may address multiple resistance mechanisms, and 57% to 67% of EGFR-mutant NSCLCs have at least some level of HER3 expression, according to the presenter.
In the phase 1 study data reported at the meeting, the response rate following U3-1402 treatment was about 31%, or 5 out of 16 patients, including 4 confirmed partial responses. Most treatment-emergent adverse events were grade 1 or 2, and only one patient discontinued due to an adverse event, according to Dr. Jänne, who said the study is ongoing.
Taken together, findings for U3-1402 and JNJ-372 show that there may be room for other approaches beyond TKIs to address the need for new therapies to overcome resistance, Dr. Bauman said in her commentary on these studies.
“Additional research will enable us to determine who will benefit from these compounds, what biomarkers are predictive, and novel combinations to consider,” she added.
Dr. Bauman reported a consulting or advisory role with Pfizer. Dr. Haura provided disclosures related to Bristol-Myers Squibb; Janssen Oncology, Boehringer Ingelheim, FORMA Therapeutics, Ignyta, Janssen, Lilly, and Ventana, plus a patent pending on technology related to kinase inhibitor sensitivity biomarkers. Dr. Jänne reported disclosures related to Gatekeeper Pharmaceuticals, Loxo, Araxes Pharma, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Lilly, and others.
SOURCE: Haura EB, et al. ASCO 2019. Abstract 9009, Jänne PA, et al. ASCO 2019. Abstract 9010.
REPORTING FROM ASCO 2019
Combo produces ‘best response rate’ after first relapse in kids with AML
CHICAGO – Administering CPX-351 prior to a three-drug regimen produced a high response rate in pediatric patients with acute myeloid leukemia (AML) in first relapse.
In a phase 1/2 trial, CPX-351 followed by fludarabine, cytarabine, and filgrastim (FLAG) produced an overall response rate of 81%, and 70% of responders had their best response while receiving CPX-351.
“This is the best response rate published in North America for those [pediatric AML patients] in first relapse,” said Todd Cooper, DO, of Seattle Children’s Hospital in Washington.
Dr. Cooper presented results from the phase 1/2 AAML1421 trial (NCT02642965) at the annual meeting of the American Society of Clinical Oncology.
The primary objective of phase 1 was to determine the recommended phase 2 dose and toxicities of CPX-351, a liposomal preparation of cytarabine and daunorubicin. The primary objective of phase 2 was to assess the best response in patients who received CPX-351 in cycle 1 and FLAG in cycle 2.
The trial enrolled 38 AML patients, 6 in the dose-finding phase and 32 in the efficacy phase. The patients’ median age at study entry was 11.91 years (range, 1.81-21.5). Most patients (88.9%) had CNS 1 disease, and most (73.7%) had not received a transplant.
Half of patients had a first complete response (CR) that lasted 180 to 365 days, 13.2% had a first CR lasting less than 180 days, and 36.8% had a first CR lasting more than 1 year.
Dosing and toxicity
During the dose-finding portion of the study, the first dose level of CPX-351 was 135 units/m2 on days 1, 3, and 5. There was one dose-limiting toxicity — grade 3 decrease in ejection fraction — so 135 units/m2 was deemed the recommended phase 2 dose.
The most common grade 3 or higher adverse events observed with CPX-351 in cycle 1 were infections and infestations (47.4%), febrile neutropenia (44.7%), maculopapular rash (39.5%), and prolonged QT interval (18.4%).
The most common grade 3 or higher adverse events observed with FLAG in cycle 2 were febrile neutropenia (23.1%), prolonged QT interval (23.1%), and infections and infestations (19.2%).
Response and survival
There were 37 patients evaluable for response. The overall response rate was defined as CR plus CR without platelet recovery (CRp) plus CR with incomplete hematologic recovery (CRi).
The overall response rate was 81.1% (n = 30), which included 20 CRs (54.1%), 5 CRps (13.5%), and 5 CRis (13.5%). Five patients had a partial response (13.5%), and two patients had treatment failure (5.4%).
During CPX-351 treatment (n = 37), the CR rate was 37.8% (n = 14), the CRp rate was 5.4% (n = 2), and the CRi rate was 32.4% (n = 12).
During FLAG treatment (n = 27), the CR rate was 48.1% (n = 13), the CRp rate was 25.9% (n = 7), and the CRi rate was 7.4% (n = 2).
Of the 25 patients who achieved a CR or CRp at any time, 21 (84%) were minimal residual disease negative by flow cytometry. Twelve patients were minimal residual disease negative after cycle 1.
Most patients who achieved a CRi or better (83.3%) went on to hematopoietic stem cell transplant.
The 2-year overall survival was 47% for all patients and 60% for responders. None of the non-responders were still alive 2 years after therapy.
“The results certainly warrant a phase 3 study of CPX-351,” Dr. Cooper said. “In fact, it is the lead molecule that’s going to be incorporated into the next COG phase 3 study.”
AAML1421 was sponsored by the Children’s Oncology Group in collaboration with the National Cancer Institute. Dr. Cooper disclosed relationships with Juno Therapeutics and Celgene.
SOURCE: Cooper TM et al. ASCO 2019. Abstract 10003.
CHICAGO – Administering CPX-351 prior to a three-drug regimen produced a high response rate in pediatric patients with acute myeloid leukemia (AML) in first relapse.
In a phase 1/2 trial, CPX-351 followed by fludarabine, cytarabine, and filgrastim (FLAG) produced an overall response rate of 81%, and 70% of responders had their best response while receiving CPX-351.
“This is the best response rate published in North America for those [pediatric AML patients] in first relapse,” said Todd Cooper, DO, of Seattle Children’s Hospital in Washington.
Dr. Cooper presented results from the phase 1/2 AAML1421 trial (NCT02642965) at the annual meeting of the American Society of Clinical Oncology.
The primary objective of phase 1 was to determine the recommended phase 2 dose and toxicities of CPX-351, a liposomal preparation of cytarabine and daunorubicin. The primary objective of phase 2 was to assess the best response in patients who received CPX-351 in cycle 1 and FLAG in cycle 2.
The trial enrolled 38 AML patients, 6 in the dose-finding phase and 32 in the efficacy phase. The patients’ median age at study entry was 11.91 years (range, 1.81-21.5). Most patients (88.9%) had CNS 1 disease, and most (73.7%) had not received a transplant.
Half of patients had a first complete response (CR) that lasted 180 to 365 days, 13.2% had a first CR lasting less than 180 days, and 36.8% had a first CR lasting more than 1 year.
Dosing and toxicity
During the dose-finding portion of the study, the first dose level of CPX-351 was 135 units/m2 on days 1, 3, and 5. There was one dose-limiting toxicity — grade 3 decrease in ejection fraction — so 135 units/m2 was deemed the recommended phase 2 dose.
The most common grade 3 or higher adverse events observed with CPX-351 in cycle 1 were infections and infestations (47.4%), febrile neutropenia (44.7%), maculopapular rash (39.5%), and prolonged QT interval (18.4%).
The most common grade 3 or higher adverse events observed with FLAG in cycle 2 were febrile neutropenia (23.1%), prolonged QT interval (23.1%), and infections and infestations (19.2%).
Response and survival
There were 37 patients evaluable for response. The overall response rate was defined as CR plus CR without platelet recovery (CRp) plus CR with incomplete hematologic recovery (CRi).
The overall response rate was 81.1% (n = 30), which included 20 CRs (54.1%), 5 CRps (13.5%), and 5 CRis (13.5%). Five patients had a partial response (13.5%), and two patients had treatment failure (5.4%).
During CPX-351 treatment (n = 37), the CR rate was 37.8% (n = 14), the CRp rate was 5.4% (n = 2), and the CRi rate was 32.4% (n = 12).
During FLAG treatment (n = 27), the CR rate was 48.1% (n = 13), the CRp rate was 25.9% (n = 7), and the CRi rate was 7.4% (n = 2).
Of the 25 patients who achieved a CR or CRp at any time, 21 (84%) were minimal residual disease negative by flow cytometry. Twelve patients were minimal residual disease negative after cycle 1.
Most patients who achieved a CRi or better (83.3%) went on to hematopoietic stem cell transplant.
The 2-year overall survival was 47% for all patients and 60% for responders. None of the non-responders were still alive 2 years after therapy.
“The results certainly warrant a phase 3 study of CPX-351,” Dr. Cooper said. “In fact, it is the lead molecule that’s going to be incorporated into the next COG phase 3 study.”
AAML1421 was sponsored by the Children’s Oncology Group in collaboration with the National Cancer Institute. Dr. Cooper disclosed relationships with Juno Therapeutics and Celgene.
SOURCE: Cooper TM et al. ASCO 2019. Abstract 10003.
CHICAGO – Administering CPX-351 prior to a three-drug regimen produced a high response rate in pediatric patients with acute myeloid leukemia (AML) in first relapse.
In a phase 1/2 trial, CPX-351 followed by fludarabine, cytarabine, and filgrastim (FLAG) produced an overall response rate of 81%, and 70% of responders had their best response while receiving CPX-351.
“This is the best response rate published in North America for those [pediatric AML patients] in first relapse,” said Todd Cooper, DO, of Seattle Children’s Hospital in Washington.
Dr. Cooper presented results from the phase 1/2 AAML1421 trial (NCT02642965) at the annual meeting of the American Society of Clinical Oncology.
The primary objective of phase 1 was to determine the recommended phase 2 dose and toxicities of CPX-351, a liposomal preparation of cytarabine and daunorubicin. The primary objective of phase 2 was to assess the best response in patients who received CPX-351 in cycle 1 and FLAG in cycle 2.
The trial enrolled 38 AML patients, 6 in the dose-finding phase and 32 in the efficacy phase. The patients’ median age at study entry was 11.91 years (range, 1.81-21.5). Most patients (88.9%) had CNS 1 disease, and most (73.7%) had not received a transplant.
Half of patients had a first complete response (CR) that lasted 180 to 365 days, 13.2% had a first CR lasting less than 180 days, and 36.8% had a first CR lasting more than 1 year.
Dosing and toxicity
During the dose-finding portion of the study, the first dose level of CPX-351 was 135 units/m2 on days 1, 3, and 5. There was one dose-limiting toxicity — grade 3 decrease in ejection fraction — so 135 units/m2 was deemed the recommended phase 2 dose.
The most common grade 3 or higher adverse events observed with CPX-351 in cycle 1 were infections and infestations (47.4%), febrile neutropenia (44.7%), maculopapular rash (39.5%), and prolonged QT interval (18.4%).
The most common grade 3 or higher adverse events observed with FLAG in cycle 2 were febrile neutropenia (23.1%), prolonged QT interval (23.1%), and infections and infestations (19.2%).
Response and survival
There were 37 patients evaluable for response. The overall response rate was defined as CR plus CR without platelet recovery (CRp) plus CR with incomplete hematologic recovery (CRi).
The overall response rate was 81.1% (n = 30), which included 20 CRs (54.1%), 5 CRps (13.5%), and 5 CRis (13.5%). Five patients had a partial response (13.5%), and two patients had treatment failure (5.4%).
During CPX-351 treatment (n = 37), the CR rate was 37.8% (n = 14), the CRp rate was 5.4% (n = 2), and the CRi rate was 32.4% (n = 12).
During FLAG treatment (n = 27), the CR rate was 48.1% (n = 13), the CRp rate was 25.9% (n = 7), and the CRi rate was 7.4% (n = 2).
Of the 25 patients who achieved a CR or CRp at any time, 21 (84%) were minimal residual disease negative by flow cytometry. Twelve patients were minimal residual disease negative after cycle 1.
Most patients who achieved a CRi or better (83.3%) went on to hematopoietic stem cell transplant.
The 2-year overall survival was 47% for all patients and 60% for responders. None of the non-responders were still alive 2 years after therapy.
“The results certainly warrant a phase 3 study of CPX-351,” Dr. Cooper said. “In fact, it is the lead molecule that’s going to be incorporated into the next COG phase 3 study.”
AAML1421 was sponsored by the Children’s Oncology Group in collaboration with the National Cancer Institute. Dr. Cooper disclosed relationships with Juno Therapeutics and Celgene.
SOURCE: Cooper TM et al. ASCO 2019. Abstract 10003.
REPORTING FROM ASCO 2019
Trial matches pediatric cancer patients to targeted therapies
Researchers have found they can screen pediatric cancer patients for genetic alterations and match those patients to appropriate targeted therapies.
Thus far, 24% of the patients screened have been matched and assigned to a treatment, and 10% have been enrolled on treatment protocols.
The patients were screened and matched as part of the National Cancer Institute–Children’s Oncology Group Pediatric MATCH (Molecular Analysis for Therapy Choice) trial.
Results from this trial are scheduled to be presented at the annual meeting of the American Society of Clinical Oncology.
Donald Williams Parsons, MD, PhD, of Baylor College of Medicine in Houston, Tex., presented some results at a press briefing in advance of the meeting. “[T]he last 10 years have been an incredible time in terms of learning more about the genetics and underlying molecular basis of both adult and pediatric cancers,” Dr. Parsons said.
He pointed out, however, that it is not yet known if this information will be useful in guiding the treatment of pediatric cancers. Specifically, how many pediatric patients can be matched to targeted therapies, and how effective will those therapies be?
The Pediatric MATCH trial (NCT03155620) was developed to answer these questions. Researchers plan to enroll at least 1,000 patients in this trial. Patients are eligible if they are 1-21 years of age and have refractory or recurrent solid tumors, non-Hodgkin lymphomas, or histiocytic disorders.
After patients are enrolled in the trial, their tumor samples undergo DNA and RNA sequencing, and the results are used to match each patient to a targeted therapy. At present, the trial can match patients to one of 10 drugs:
- larotrectinib (targeting NTRK fusions).
- erdafitinib (targeting FGFR1/2/3/4).
- tazemetostat (targeting EZH2 or members of the SWI/SNF complex).
- LY3023414 (targeting the PI3K/MTOR pathway).
- selumetinib (targeting the MAPK pathway).
- ensartinib (targeting ALK or ROS1).
- vemurafenib (targeting BRAF V600 mutations).
- olaparib (targeting defects in DNA damage repair).
- palbociclib (targeting alterations in cell cycle genes).
- ulixertinib (targeting MAPK pathway mutations).
Early results
From July 2017 through December 2018, 422 patients were enrolled in the trial. The patients had more than 60 different diagnoses, including brain tumors, sarcomas, neuroblastoma, renal and liver cancers, and other malignancies.
The researchers received tumor samples from 390 patients, attempted sequencing of 370 samples (95%), and completed sequencing of 357 samples (92%).
A treatment target was found in 112 (29%) patients, 95 (24%) of those patients were assigned to a treatment, and 39 (10%) were enrolled in a protocol. The median turnaround time from sample receipt to treatment assignment was 15 days.
“In addition to the sequencing being successful, the patients are being matched to the different treatments,” Dr. Parsons said. He added that the study is ongoing, so more of the matched and assigned patients will be enrolled in protocols in the future.
Dr. Parsons also presented results by tumor type. A targetable alteration was identified in 26% (67/255) of all non–central nervous system solid tumors, 13% (10/75) of osteosarcomas, 50% (18/36) of rhabdomyosarcomas, 21% (7/33) of Ewing sarcomas, 25% (9/36) of other sarcomas, 19% (5/26) of renal cancers, 16% (3/19) of carcinomas, 44% (8/18) of neuroblastomas, 43% (3/7) of liver cancers, and 29% (4/14) of “other” tumors.
Drilling down further, Dr. Parsons presented details on specific alterations in one cancer type: astrocytomas. Targetable alterations were found in 74% (29/39) of astrocytomas. This includes NF1 mutations (18%), BRAF V600E (15%), FGFR1 fusions/mutations (10%), BRAF fusions (10%), PIK3CA mutations (8%), NRAS/KRAS mutations (5%), and other alterations.
“Pretty remarkably, in this one diagnosis, there are patients who have been matched to nine of the ten different treatment arms,” Dr. Parsons said. “This study is allowing us to evaluate targeted therapies – specific types of investigational drugs – in patients with many different cancer types, some common, some very rare. So, hopefully, we can study these agents and identify signals of activity where some of these drugs may work for our patients.”
The Pediatric MATCH trial is sponsored by the National Cancer Institute. Dr. Parsons has patents, royalties, and other intellectual property related to genes discovered through sequencing of several adult cancer types.
SOURCE: Parsons DW et al. ASCO 2019, Abstract 10011.
Researchers have found they can screen pediatric cancer patients for genetic alterations and match those patients to appropriate targeted therapies.
Thus far, 24% of the patients screened have been matched and assigned to a treatment, and 10% have been enrolled on treatment protocols.
The patients were screened and matched as part of the National Cancer Institute–Children’s Oncology Group Pediatric MATCH (Molecular Analysis for Therapy Choice) trial.
Results from this trial are scheduled to be presented at the annual meeting of the American Society of Clinical Oncology.
Donald Williams Parsons, MD, PhD, of Baylor College of Medicine in Houston, Tex., presented some results at a press briefing in advance of the meeting. “[T]he last 10 years have been an incredible time in terms of learning more about the genetics and underlying molecular basis of both adult and pediatric cancers,” Dr. Parsons said.
He pointed out, however, that it is not yet known if this information will be useful in guiding the treatment of pediatric cancers. Specifically, how many pediatric patients can be matched to targeted therapies, and how effective will those therapies be?
The Pediatric MATCH trial (NCT03155620) was developed to answer these questions. Researchers plan to enroll at least 1,000 patients in this trial. Patients are eligible if they are 1-21 years of age and have refractory or recurrent solid tumors, non-Hodgkin lymphomas, or histiocytic disorders.
After patients are enrolled in the trial, their tumor samples undergo DNA and RNA sequencing, and the results are used to match each patient to a targeted therapy. At present, the trial can match patients to one of 10 drugs:
- larotrectinib (targeting NTRK fusions).
- erdafitinib (targeting FGFR1/2/3/4).
- tazemetostat (targeting EZH2 or members of the SWI/SNF complex).
- LY3023414 (targeting the PI3K/MTOR pathway).
- selumetinib (targeting the MAPK pathway).
- ensartinib (targeting ALK or ROS1).
- vemurafenib (targeting BRAF V600 mutations).
- olaparib (targeting defects in DNA damage repair).
- palbociclib (targeting alterations in cell cycle genes).
- ulixertinib (targeting MAPK pathway mutations).
Early results
From July 2017 through December 2018, 422 patients were enrolled in the trial. The patients had more than 60 different diagnoses, including brain tumors, sarcomas, neuroblastoma, renal and liver cancers, and other malignancies.
The researchers received tumor samples from 390 patients, attempted sequencing of 370 samples (95%), and completed sequencing of 357 samples (92%).
A treatment target was found in 112 (29%) patients, 95 (24%) of those patients were assigned to a treatment, and 39 (10%) were enrolled in a protocol. The median turnaround time from sample receipt to treatment assignment was 15 days.
“In addition to the sequencing being successful, the patients are being matched to the different treatments,” Dr. Parsons said. He added that the study is ongoing, so more of the matched and assigned patients will be enrolled in protocols in the future.
Dr. Parsons also presented results by tumor type. A targetable alteration was identified in 26% (67/255) of all non–central nervous system solid tumors, 13% (10/75) of osteosarcomas, 50% (18/36) of rhabdomyosarcomas, 21% (7/33) of Ewing sarcomas, 25% (9/36) of other sarcomas, 19% (5/26) of renal cancers, 16% (3/19) of carcinomas, 44% (8/18) of neuroblastomas, 43% (3/7) of liver cancers, and 29% (4/14) of “other” tumors.
Drilling down further, Dr. Parsons presented details on specific alterations in one cancer type: astrocytomas. Targetable alterations were found in 74% (29/39) of astrocytomas. This includes NF1 mutations (18%), BRAF V600E (15%), FGFR1 fusions/mutations (10%), BRAF fusions (10%), PIK3CA mutations (8%), NRAS/KRAS mutations (5%), and other alterations.
“Pretty remarkably, in this one diagnosis, there are patients who have been matched to nine of the ten different treatment arms,” Dr. Parsons said. “This study is allowing us to evaluate targeted therapies – specific types of investigational drugs – in patients with many different cancer types, some common, some very rare. So, hopefully, we can study these agents and identify signals of activity where some of these drugs may work for our patients.”
The Pediatric MATCH trial is sponsored by the National Cancer Institute. Dr. Parsons has patents, royalties, and other intellectual property related to genes discovered through sequencing of several adult cancer types.
SOURCE: Parsons DW et al. ASCO 2019, Abstract 10011.
Researchers have found they can screen pediatric cancer patients for genetic alterations and match those patients to appropriate targeted therapies.
Thus far, 24% of the patients screened have been matched and assigned to a treatment, and 10% have been enrolled on treatment protocols.
The patients were screened and matched as part of the National Cancer Institute–Children’s Oncology Group Pediatric MATCH (Molecular Analysis for Therapy Choice) trial.
Results from this trial are scheduled to be presented at the annual meeting of the American Society of Clinical Oncology.
Donald Williams Parsons, MD, PhD, of Baylor College of Medicine in Houston, Tex., presented some results at a press briefing in advance of the meeting. “[T]he last 10 years have been an incredible time in terms of learning more about the genetics and underlying molecular basis of both adult and pediatric cancers,” Dr. Parsons said.
He pointed out, however, that it is not yet known if this information will be useful in guiding the treatment of pediatric cancers. Specifically, how many pediatric patients can be matched to targeted therapies, and how effective will those therapies be?
The Pediatric MATCH trial (NCT03155620) was developed to answer these questions. Researchers plan to enroll at least 1,000 patients in this trial. Patients are eligible if they are 1-21 years of age and have refractory or recurrent solid tumors, non-Hodgkin lymphomas, or histiocytic disorders.
After patients are enrolled in the trial, their tumor samples undergo DNA and RNA sequencing, and the results are used to match each patient to a targeted therapy. At present, the trial can match patients to one of 10 drugs:
- larotrectinib (targeting NTRK fusions).
- erdafitinib (targeting FGFR1/2/3/4).
- tazemetostat (targeting EZH2 or members of the SWI/SNF complex).
- LY3023414 (targeting the PI3K/MTOR pathway).
- selumetinib (targeting the MAPK pathway).
- ensartinib (targeting ALK or ROS1).
- vemurafenib (targeting BRAF V600 mutations).
- olaparib (targeting defects in DNA damage repair).
- palbociclib (targeting alterations in cell cycle genes).
- ulixertinib (targeting MAPK pathway mutations).
Early results
From July 2017 through December 2018, 422 patients were enrolled in the trial. The patients had more than 60 different diagnoses, including brain tumors, sarcomas, neuroblastoma, renal and liver cancers, and other malignancies.
The researchers received tumor samples from 390 patients, attempted sequencing of 370 samples (95%), and completed sequencing of 357 samples (92%).
A treatment target was found in 112 (29%) patients, 95 (24%) of those patients were assigned to a treatment, and 39 (10%) were enrolled in a protocol. The median turnaround time from sample receipt to treatment assignment was 15 days.
“In addition to the sequencing being successful, the patients are being matched to the different treatments,” Dr. Parsons said. He added that the study is ongoing, so more of the matched and assigned patients will be enrolled in protocols in the future.
Dr. Parsons also presented results by tumor type. A targetable alteration was identified in 26% (67/255) of all non–central nervous system solid tumors, 13% (10/75) of osteosarcomas, 50% (18/36) of rhabdomyosarcomas, 21% (7/33) of Ewing sarcomas, 25% (9/36) of other sarcomas, 19% (5/26) of renal cancers, 16% (3/19) of carcinomas, 44% (8/18) of neuroblastomas, 43% (3/7) of liver cancers, and 29% (4/14) of “other” tumors.
Drilling down further, Dr. Parsons presented details on specific alterations in one cancer type: astrocytomas. Targetable alterations were found in 74% (29/39) of astrocytomas. This includes NF1 mutations (18%), BRAF V600E (15%), FGFR1 fusions/mutations (10%), BRAF fusions (10%), PIK3CA mutations (8%), NRAS/KRAS mutations (5%), and other alterations.
“Pretty remarkably, in this one diagnosis, there are patients who have been matched to nine of the ten different treatment arms,” Dr. Parsons said. “This study is allowing us to evaluate targeted therapies – specific types of investigational drugs – in patients with many different cancer types, some common, some very rare. So, hopefully, we can study these agents and identify signals of activity where some of these drugs may work for our patients.”
The Pediatric MATCH trial is sponsored by the National Cancer Institute. Dr. Parsons has patents, royalties, and other intellectual property related to genes discovered through sequencing of several adult cancer types.
SOURCE: Parsons DW et al. ASCO 2019, Abstract 10011.
REPORTING FROM ASCO 2019