User login
What are the cardiorenal differences between type 1 and type 2 diabetes?
While type 2 diabetes is associated with a greater risk for cardiovascular events than type 1 diabetes, the latter is more associated with chronic kidney complications, according to data from a French observational study.
That’s not to say that type 1 diabetes isn’t also associated with poor heart health that is of concern, according to Denis Angoulvant, MD, of Tours (France) Regional University Hospital and Trousseau Hospital in Paris.
“The difference is that, in the middle or older ages, we suddenly see a surge of cardiovascular events in type 1 diabetic patients,” he said at the annual meeting of the European Association for the Study of Diabetes. “As a cardiologist, I must say that we are barely see these patients ahead of those complications, so we advocate that there’s a gap to be filled here to prevent these events in these patients.”
Few studies have looked at the comparative risks for cardiovascular and renal outcomes between patients with type 1 and type 2 diabetes, Dr. Angoulvant said, so the aim of the study he presented was to look at this in more detail.
Comparing cardiovascular and renal outcomes
Data from the French hospital discharge database (PMSI), which covers more than 98% of the country’s population, were used to find all adults with type 1 or type 2 diabetes who had at least 5 years of follow-up data starting from 2013.
Not surprisingly, there were eight times as many individuals with type 2 diabetes (425,207) than those with type 1 diabetes (50,623), and patients with type 2 diabetes tended to be older than those with type 1 diabetes (mean age, 68.6 vs. 61.4 years).
There were many significant differences between the two groups of patients in terms of clinical variables, such as patients with type 2 diabetes having more cardiovascular risk factors or preexisting heart problems, and those with type 1 diabetes more likely to have diabetic eye disease.
Indeed, Dr. Angoulvant pointed out that those with type 2 diabetes were significantly more likely (all P < .0001) than those with type 1 diabetes to have: hypertension (70.8% vs. 50.5%), heart failure (35.7% vs. 16.4%), valvular heart disease (7.2% vs. 3.5%), dilated cardiomyopathy (5.5% vs. 2.7%), coronary artery disease (27.6 vs. 18.6%), previous MI (3.0% vs. 2.4%), peripheral vascular disease (22.0% vs. 15.5%), and ischemic stroke (3.3 vs. 2.2%).
“Regarding more specific microvascular diabetic complications, we had a higher incidence of chronic kidney disease in type 2 diabetes patients [10.2% vs. 9.1%], but a higher incidence of diabetic retinopathy in type 1 diabetes patients [6.6% vs. 12.2%],” Dr. Angoulvant said.
Considering more than 2 million person-years of follow-up, the annual rates of MI, new-onset heart failure, ischemic stroke, and chronic kidney disease for the whole study population were respective 1.4%, 5.4%, 1.2%, and 3.4%. The annual rates for death from any cause was 9.7%, and for a cardiovascular reason was 2.4%.
Cardiovascular disease prevalence and event rates
The mean follow-up period was 4.3 years, and over this time the age- and sex-adjusted prevalence of cardiovascular disease was found to be highest in individuals with type 2 diabetes, especially after the age of 40 years.
Looking at the rates of different cardiovascular events showed that both younger (18-29 years) and older (60+ years) people with type 1 diabetes had a 1.2-fold higher risk for MI than similarly aged individuals with type 2 diabetes.
Furthermore, younger and older type 1 diabetes individuals had a 1.1- to 1.4-fold greater risk of new-onset heart failure than those with type 2 diabetes.
“Interestingly, regarding the incidence of ischemic stroke in our population, we found no significant difference between patients with type 1 diabetes, and patients with type 2 diabetes,” Dr. Angoulvant said.
Chronic kidney disease and risk for death
Chronic kidney disease was most common in individuals with type 1 diabetes who were aged between 18 and 69 years, with a greater prevalence also seen in those with type 2 diabetes only after age 80.
The risk of new chronic kidney disease was significantly increased in patients with type 1 diabetes, compared with patients with type 2 diabetes, with a 1.1- to 2.4-fold increase seen, first in individuals aged 18-49 years, and then again after the age of 60 years.
Dr. Angoulvant reported that the risk of dying from any cause was 1.1-fold higher in people with type 1 diabetes, compared with those with type 2 diabetes, but after the age of 60 years.
The risk of death from cardiovascular events was also increased in people with type 1 diabetes, but between the ages of 60 and 69 years.
Asked what his take-home message might be, Dr. Angoulvant stressed the importance of heart failure, in all patients with diabetes but particularly in those with type 1 diabetes.
“I think there is room for improvement in terms of assessing who is going to have heart failure, how to assess heart failure, and more importantly, how to prevent heart failure,” perhaps by “introducing those drugs that have shown tremendous benefit regarding hospitalization, such as [sodium-glucose transporter 2] inhibitors” in patients with type 1 diabetes ahead of the events, he said.
Dr. Angoulvant had no conflicts of interest to disclose.
While type 2 diabetes is associated with a greater risk for cardiovascular events than type 1 diabetes, the latter is more associated with chronic kidney complications, according to data from a French observational study.
That’s not to say that type 1 diabetes isn’t also associated with poor heart health that is of concern, according to Denis Angoulvant, MD, of Tours (France) Regional University Hospital and Trousseau Hospital in Paris.
“The difference is that, in the middle or older ages, we suddenly see a surge of cardiovascular events in type 1 diabetic patients,” he said at the annual meeting of the European Association for the Study of Diabetes. “As a cardiologist, I must say that we are barely see these patients ahead of those complications, so we advocate that there’s a gap to be filled here to prevent these events in these patients.”
Few studies have looked at the comparative risks for cardiovascular and renal outcomes between patients with type 1 and type 2 diabetes, Dr. Angoulvant said, so the aim of the study he presented was to look at this in more detail.
Comparing cardiovascular and renal outcomes
Data from the French hospital discharge database (PMSI), which covers more than 98% of the country’s population, were used to find all adults with type 1 or type 2 diabetes who had at least 5 years of follow-up data starting from 2013.
Not surprisingly, there were eight times as many individuals with type 2 diabetes (425,207) than those with type 1 diabetes (50,623), and patients with type 2 diabetes tended to be older than those with type 1 diabetes (mean age, 68.6 vs. 61.4 years).
There were many significant differences between the two groups of patients in terms of clinical variables, such as patients with type 2 diabetes having more cardiovascular risk factors or preexisting heart problems, and those with type 1 diabetes more likely to have diabetic eye disease.
Indeed, Dr. Angoulvant pointed out that those with type 2 diabetes were significantly more likely (all P < .0001) than those with type 1 diabetes to have: hypertension (70.8% vs. 50.5%), heart failure (35.7% vs. 16.4%), valvular heart disease (7.2% vs. 3.5%), dilated cardiomyopathy (5.5% vs. 2.7%), coronary artery disease (27.6 vs. 18.6%), previous MI (3.0% vs. 2.4%), peripheral vascular disease (22.0% vs. 15.5%), and ischemic stroke (3.3 vs. 2.2%).
“Regarding more specific microvascular diabetic complications, we had a higher incidence of chronic kidney disease in type 2 diabetes patients [10.2% vs. 9.1%], but a higher incidence of diabetic retinopathy in type 1 diabetes patients [6.6% vs. 12.2%],” Dr. Angoulvant said.
Considering more than 2 million person-years of follow-up, the annual rates of MI, new-onset heart failure, ischemic stroke, and chronic kidney disease for the whole study population were respective 1.4%, 5.4%, 1.2%, and 3.4%. The annual rates for death from any cause was 9.7%, and for a cardiovascular reason was 2.4%.
Cardiovascular disease prevalence and event rates
The mean follow-up period was 4.3 years, and over this time the age- and sex-adjusted prevalence of cardiovascular disease was found to be highest in individuals with type 2 diabetes, especially after the age of 40 years.
Looking at the rates of different cardiovascular events showed that both younger (18-29 years) and older (60+ years) people with type 1 diabetes had a 1.2-fold higher risk for MI than similarly aged individuals with type 2 diabetes.
Furthermore, younger and older type 1 diabetes individuals had a 1.1- to 1.4-fold greater risk of new-onset heart failure than those with type 2 diabetes.
“Interestingly, regarding the incidence of ischemic stroke in our population, we found no significant difference between patients with type 1 diabetes, and patients with type 2 diabetes,” Dr. Angoulvant said.
Chronic kidney disease and risk for death
Chronic kidney disease was most common in individuals with type 1 diabetes who were aged between 18 and 69 years, with a greater prevalence also seen in those with type 2 diabetes only after age 80.
The risk of new chronic kidney disease was significantly increased in patients with type 1 diabetes, compared with patients with type 2 diabetes, with a 1.1- to 2.4-fold increase seen, first in individuals aged 18-49 years, and then again after the age of 60 years.
Dr. Angoulvant reported that the risk of dying from any cause was 1.1-fold higher in people with type 1 diabetes, compared with those with type 2 diabetes, but after the age of 60 years.
The risk of death from cardiovascular events was also increased in people with type 1 diabetes, but between the ages of 60 and 69 years.
Asked what his take-home message might be, Dr. Angoulvant stressed the importance of heart failure, in all patients with diabetes but particularly in those with type 1 diabetes.
“I think there is room for improvement in terms of assessing who is going to have heart failure, how to assess heart failure, and more importantly, how to prevent heart failure,” perhaps by “introducing those drugs that have shown tremendous benefit regarding hospitalization, such as [sodium-glucose transporter 2] inhibitors” in patients with type 1 diabetes ahead of the events, he said.
Dr. Angoulvant had no conflicts of interest to disclose.
While type 2 diabetes is associated with a greater risk for cardiovascular events than type 1 diabetes, the latter is more associated with chronic kidney complications, according to data from a French observational study.
That’s not to say that type 1 diabetes isn’t also associated with poor heart health that is of concern, according to Denis Angoulvant, MD, of Tours (France) Regional University Hospital and Trousseau Hospital in Paris.
“The difference is that, in the middle or older ages, we suddenly see a surge of cardiovascular events in type 1 diabetic patients,” he said at the annual meeting of the European Association for the Study of Diabetes. “As a cardiologist, I must say that we are barely see these patients ahead of those complications, so we advocate that there’s a gap to be filled here to prevent these events in these patients.”
Few studies have looked at the comparative risks for cardiovascular and renal outcomes between patients with type 1 and type 2 diabetes, Dr. Angoulvant said, so the aim of the study he presented was to look at this in more detail.
Comparing cardiovascular and renal outcomes
Data from the French hospital discharge database (PMSI), which covers more than 98% of the country’s population, were used to find all adults with type 1 or type 2 diabetes who had at least 5 years of follow-up data starting from 2013.
Not surprisingly, there were eight times as many individuals with type 2 diabetes (425,207) than those with type 1 diabetes (50,623), and patients with type 2 diabetes tended to be older than those with type 1 diabetes (mean age, 68.6 vs. 61.4 years).
There were many significant differences between the two groups of patients in terms of clinical variables, such as patients with type 2 diabetes having more cardiovascular risk factors or preexisting heart problems, and those with type 1 diabetes more likely to have diabetic eye disease.
Indeed, Dr. Angoulvant pointed out that those with type 2 diabetes were significantly more likely (all P < .0001) than those with type 1 diabetes to have: hypertension (70.8% vs. 50.5%), heart failure (35.7% vs. 16.4%), valvular heart disease (7.2% vs. 3.5%), dilated cardiomyopathy (5.5% vs. 2.7%), coronary artery disease (27.6 vs. 18.6%), previous MI (3.0% vs. 2.4%), peripheral vascular disease (22.0% vs. 15.5%), and ischemic stroke (3.3 vs. 2.2%).
“Regarding more specific microvascular diabetic complications, we had a higher incidence of chronic kidney disease in type 2 diabetes patients [10.2% vs. 9.1%], but a higher incidence of diabetic retinopathy in type 1 diabetes patients [6.6% vs. 12.2%],” Dr. Angoulvant said.
Considering more than 2 million person-years of follow-up, the annual rates of MI, new-onset heart failure, ischemic stroke, and chronic kidney disease for the whole study population were respective 1.4%, 5.4%, 1.2%, and 3.4%. The annual rates for death from any cause was 9.7%, and for a cardiovascular reason was 2.4%.
Cardiovascular disease prevalence and event rates
The mean follow-up period was 4.3 years, and over this time the age- and sex-adjusted prevalence of cardiovascular disease was found to be highest in individuals with type 2 diabetes, especially after the age of 40 years.
Looking at the rates of different cardiovascular events showed that both younger (18-29 years) and older (60+ years) people with type 1 diabetes had a 1.2-fold higher risk for MI than similarly aged individuals with type 2 diabetes.
Furthermore, younger and older type 1 diabetes individuals had a 1.1- to 1.4-fold greater risk of new-onset heart failure than those with type 2 diabetes.
“Interestingly, regarding the incidence of ischemic stroke in our population, we found no significant difference between patients with type 1 diabetes, and patients with type 2 diabetes,” Dr. Angoulvant said.
Chronic kidney disease and risk for death
Chronic kidney disease was most common in individuals with type 1 diabetes who were aged between 18 and 69 years, with a greater prevalence also seen in those with type 2 diabetes only after age 80.
The risk of new chronic kidney disease was significantly increased in patients with type 1 diabetes, compared with patients with type 2 diabetes, with a 1.1- to 2.4-fold increase seen, first in individuals aged 18-49 years, and then again after the age of 60 years.
Dr. Angoulvant reported that the risk of dying from any cause was 1.1-fold higher in people with type 1 diabetes, compared with those with type 2 diabetes, but after the age of 60 years.
The risk of death from cardiovascular events was also increased in people with type 1 diabetes, but between the ages of 60 and 69 years.
Asked what his take-home message might be, Dr. Angoulvant stressed the importance of heart failure, in all patients with diabetes but particularly in those with type 1 diabetes.
“I think there is room for improvement in terms of assessing who is going to have heart failure, how to assess heart failure, and more importantly, how to prevent heart failure,” perhaps by “introducing those drugs that have shown tremendous benefit regarding hospitalization, such as [sodium-glucose transporter 2] inhibitors” in patients with type 1 diabetes ahead of the events, he said.
Dr. Angoulvant had no conflicts of interest to disclose.
FROM EASD 2021
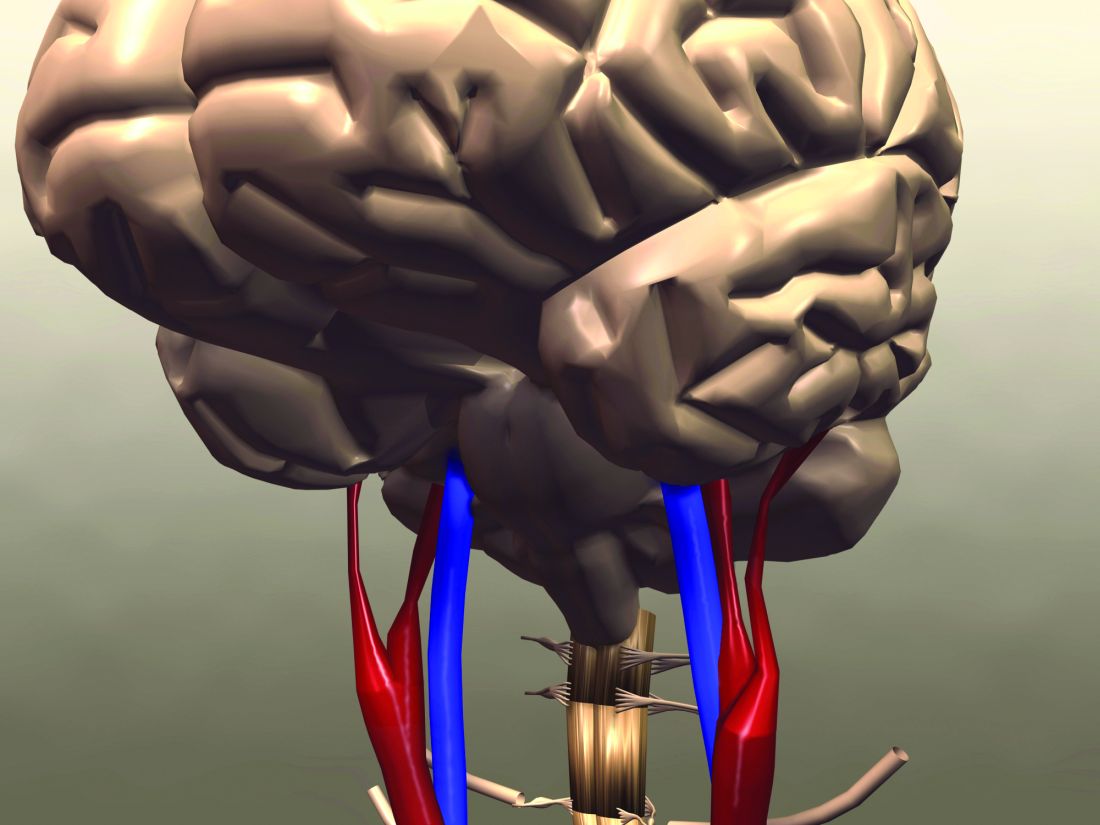
Estimating insulin resistance may help predict stroke, death in T2D
Calculating the estimated glucose disposal rate (eGDR) as a proxy for the level of insulin resistance may be useful way to determine if someone with type 2 diabetes (T2D) is at risk for having a first stroke, Swedish researchers have found.
In a large population-based study, the lower the eGDR score went, the higher the risk for having a first stroke became.
The eGDR score was also predictive of the chance of dying from any or a cardiovascular cause, Alexander Zabala, MD, reported at the annual meeting of the European Association for the Study of Diabetes (Abstract OP 01-4).
The link between insulin resistance and an increased risk for stroke has been known for some time, and not just in people with T2D. However, the current way of determining insulin resistance is not suitable for widespread practice.
“The goal standard technique for measuring insulin resistance is the euglycemic clamp method,” said Dr. Zabala, an internal medical resident at Södersjukhuset hospital and researcher at the Karolinska Institutet in Stockholm.
“For that reason, [the eGDR], a method based on readily available clinical factors – waist circumference, hypertension, and glycosylated hemoglobin was developed,” he explained. Body mass index can also be used in place of waist circumference, he qualified.
The eGDR has already been proven to be very precise in people with type 1 diabetes, said Dr. Zabala, and could be an “excellent tool to measure insulin resistance in a large patient population.”
Investigating the link between eGDR and first stroke risk
The aim of the study he presented was to see if changes in the eGDR were associated with changes in the risk of someone with T2D experiencing a first stroke, or dying from a cardiovascular or other cause.
An observational cohort was formed by first considering data on all adult patients with T2D who were logged in the Swedish National Diabetes Registry (NDR) during 2004-2016. Then anyone with a history of stroke, or with any missing data on the clinical variables needed to calculate the eGDR, were excluded.
This resulted in an overall population of 104,697 individuals, aged a mean of 63 years, who had developed T2D at around the age of 59 years. About 44% of the study population were women. The mean eGDR for the whole population was 5.6 mg/kg per min.
The study subjects were grouped according to four eGDR levels: 24,706 were in the lowest quartile of eGDR (less than 4 mg/kg per min), signifying the highest level of insulin resistance, and 18,762 were in the upper quartile of eGDR (greater than 8 mg/kg per min), signifying the lowest level of insulin resistance. The middle two groups had an eGDR between 4 and 6 mg/kg per min (40,187), and 6 and 8 mg/kg/min (21,042).
Data from the NDR were then combined with the Swedish Cause of Death register, the Swedish In-patient Care Diagnoses registry, and the Longitudinal Database for Health Insurance and Labour Market Studies (LISA) to determine the rates of stroke, ischemic stroke, hemorrhagic stroke, all-cause mortality, and cardiovascular mortality.
Increasing insulin resistance ups risk for stroke, death
After a median follow-up of 5.6 years, 4% (4,201) of the study population had had a stroke.
“We clearly see an increased occurrence of first-time stroke in the group with the lowest eGDR, indicating worst insulin resistance, in comparison with the group with the highest eGDR, indicating less insulin resistance,” Dr. Zabala reported.
After adjustment for potential confounding factors, including age at baseline, gender, diabetes duration, among other variables, the risk for stroke was lowest in those with a high eGDR value and highest for those with a low eGDR value.
Using individuals with the lowest eGDR (less than 4 mg/kg per min) and thus greatest risk of stroke as the reference, adjusted hazard ratios (aHR) for first-time stroke were: 0.60, 0.68, and 0.77 for those with an eGDR of greater than 8, 6-8, and 4-6 mg/kg per min, respectively.
The corresponding values for risk of ischemic stroke were 0.55, 0.68, and 0.75. Regarding hemorrhagic stroke, there was no statistically significant correlation between eGDR levels and stroke occurrence. This was due to the small number of cases recorded.
As for all-cause and cardiovascular mortality, a similar pattern was seen, with higher rates of death linked to increasing insulin resistance. Adjusted hazard ratios according to increasing insulin resistance (decreasing eGDR scores) for all-cause death were 0.68, 0.75, and 0.82 and for cardiovascular mortality were 0.65, 0.75, and 0.82.
A sensitivity analysis, using BMI instead of waist circumference to calculate the eGDR, showed a similar pattern, and “interestingly, a correlation between eGDR levels and risk of hemorrhagic stroke.” Dr. Zabala said.
Limitations and take-homes
Of course, this is an observational cohort study, so no conclusions on causality can be made and there are no data on the use of anti-diabetic treatments specifically. But there are strengths such as covering almost all adults with T2D in Sweden and a relatively long-follow-up time.
The findings suggest that “eGDR, which may reflect insulin resistance may be a useful risk marker for stroke and death in people with type 2 diabetes,” said Dr. Zabala.
“You had a very large cohort, and that certainly makes your results very valid,” observed Peter Novodvorsky, MUDr. (Hons), PhD, MRCP, a consultant diabetologist in Trenčín, Slovakia.
Dr. Novodvorsky, who chaired the session, picked up on the lack of information about how many people were taking newer diabetes drugs, such as the glucagon-like peptide 1 receptor antagonists and sodium glucose-lowering transport 2 inhibitors.
“As we all know, these might have protective effects which are not necessarily related to the glucose lowering or insulin resistance-lowering” effects, so could have influenced the results. In terms of how practical the eGDR is for clinical practice, Dr. Zabala observed in a press release: “eGDR could be used to help T2D patients better understand and manage their risk of stroke and death.
“It could also be of importance in research. In this era of personalized medicine, better stratification of type 2 diabetes patients will help optimize clinical trials and further vital research into treatment, diagnosis, care and prevention.”
The research was a collaboration between the Karolinska Institutet, Gothenburg University and the Swedish National Diabetes Registry. Dr. Zabala and coauthors reported having no conflicts of interest.
Calculating the estimated glucose disposal rate (eGDR) as a proxy for the level of insulin resistance may be useful way to determine if someone with type 2 diabetes (T2D) is at risk for having a first stroke, Swedish researchers have found.
In a large population-based study, the lower the eGDR score went, the higher the risk for having a first stroke became.
The eGDR score was also predictive of the chance of dying from any or a cardiovascular cause, Alexander Zabala, MD, reported at the annual meeting of the European Association for the Study of Diabetes (Abstract OP 01-4).
The link between insulin resistance and an increased risk for stroke has been known for some time, and not just in people with T2D. However, the current way of determining insulin resistance is not suitable for widespread practice.
“The goal standard technique for measuring insulin resistance is the euglycemic clamp method,” said Dr. Zabala, an internal medical resident at Södersjukhuset hospital and researcher at the Karolinska Institutet in Stockholm.
“For that reason, [the eGDR], a method based on readily available clinical factors – waist circumference, hypertension, and glycosylated hemoglobin was developed,” he explained. Body mass index can also be used in place of waist circumference, he qualified.
The eGDR has already been proven to be very precise in people with type 1 diabetes, said Dr. Zabala, and could be an “excellent tool to measure insulin resistance in a large patient population.”
Investigating the link between eGDR and first stroke risk
The aim of the study he presented was to see if changes in the eGDR were associated with changes in the risk of someone with T2D experiencing a first stroke, or dying from a cardiovascular or other cause.
An observational cohort was formed by first considering data on all adult patients with T2D who were logged in the Swedish National Diabetes Registry (NDR) during 2004-2016. Then anyone with a history of stroke, or with any missing data on the clinical variables needed to calculate the eGDR, were excluded.
This resulted in an overall population of 104,697 individuals, aged a mean of 63 years, who had developed T2D at around the age of 59 years. About 44% of the study population were women. The mean eGDR for the whole population was 5.6 mg/kg per min.
The study subjects were grouped according to four eGDR levels: 24,706 were in the lowest quartile of eGDR (less than 4 mg/kg per min), signifying the highest level of insulin resistance, and 18,762 were in the upper quartile of eGDR (greater than 8 mg/kg per min), signifying the lowest level of insulin resistance. The middle two groups had an eGDR between 4 and 6 mg/kg per min (40,187), and 6 and 8 mg/kg/min (21,042).
Data from the NDR were then combined with the Swedish Cause of Death register, the Swedish In-patient Care Diagnoses registry, and the Longitudinal Database for Health Insurance and Labour Market Studies (LISA) to determine the rates of stroke, ischemic stroke, hemorrhagic stroke, all-cause mortality, and cardiovascular mortality.
Increasing insulin resistance ups risk for stroke, death
After a median follow-up of 5.6 years, 4% (4,201) of the study population had had a stroke.
“We clearly see an increased occurrence of first-time stroke in the group with the lowest eGDR, indicating worst insulin resistance, in comparison with the group with the highest eGDR, indicating less insulin resistance,” Dr. Zabala reported.
After adjustment for potential confounding factors, including age at baseline, gender, diabetes duration, among other variables, the risk for stroke was lowest in those with a high eGDR value and highest for those with a low eGDR value.
Using individuals with the lowest eGDR (less than 4 mg/kg per min) and thus greatest risk of stroke as the reference, adjusted hazard ratios (aHR) for first-time stroke were: 0.60, 0.68, and 0.77 for those with an eGDR of greater than 8, 6-8, and 4-6 mg/kg per min, respectively.
The corresponding values for risk of ischemic stroke were 0.55, 0.68, and 0.75. Regarding hemorrhagic stroke, there was no statistically significant correlation between eGDR levels and stroke occurrence. This was due to the small number of cases recorded.
As for all-cause and cardiovascular mortality, a similar pattern was seen, with higher rates of death linked to increasing insulin resistance. Adjusted hazard ratios according to increasing insulin resistance (decreasing eGDR scores) for all-cause death were 0.68, 0.75, and 0.82 and for cardiovascular mortality were 0.65, 0.75, and 0.82.
A sensitivity analysis, using BMI instead of waist circumference to calculate the eGDR, showed a similar pattern, and “interestingly, a correlation between eGDR levels and risk of hemorrhagic stroke.” Dr. Zabala said.
Limitations and take-homes
Of course, this is an observational cohort study, so no conclusions on causality can be made and there are no data on the use of anti-diabetic treatments specifically. But there are strengths such as covering almost all adults with T2D in Sweden and a relatively long-follow-up time.
The findings suggest that “eGDR, which may reflect insulin resistance may be a useful risk marker for stroke and death in people with type 2 diabetes,” said Dr. Zabala.
“You had a very large cohort, and that certainly makes your results very valid,” observed Peter Novodvorsky, MUDr. (Hons), PhD, MRCP, a consultant diabetologist in Trenčín, Slovakia.
Dr. Novodvorsky, who chaired the session, picked up on the lack of information about how many people were taking newer diabetes drugs, such as the glucagon-like peptide 1 receptor antagonists and sodium glucose-lowering transport 2 inhibitors.
“As we all know, these might have protective effects which are not necessarily related to the glucose lowering or insulin resistance-lowering” effects, so could have influenced the results. In terms of how practical the eGDR is for clinical practice, Dr. Zabala observed in a press release: “eGDR could be used to help T2D patients better understand and manage their risk of stroke and death.
“It could also be of importance in research. In this era of personalized medicine, better stratification of type 2 diabetes patients will help optimize clinical trials and further vital research into treatment, diagnosis, care and prevention.”
The research was a collaboration between the Karolinska Institutet, Gothenburg University and the Swedish National Diabetes Registry. Dr. Zabala and coauthors reported having no conflicts of interest.
Calculating the estimated glucose disposal rate (eGDR) as a proxy for the level of insulin resistance may be useful way to determine if someone with type 2 diabetes (T2D) is at risk for having a first stroke, Swedish researchers have found.
In a large population-based study, the lower the eGDR score went, the higher the risk for having a first stroke became.
The eGDR score was also predictive of the chance of dying from any or a cardiovascular cause, Alexander Zabala, MD, reported at the annual meeting of the European Association for the Study of Diabetes (Abstract OP 01-4).
The link between insulin resistance and an increased risk for stroke has been known for some time, and not just in people with T2D. However, the current way of determining insulin resistance is not suitable for widespread practice.
“The goal standard technique for measuring insulin resistance is the euglycemic clamp method,” said Dr. Zabala, an internal medical resident at Södersjukhuset hospital and researcher at the Karolinska Institutet in Stockholm.
“For that reason, [the eGDR], a method based on readily available clinical factors – waist circumference, hypertension, and glycosylated hemoglobin was developed,” he explained. Body mass index can also be used in place of waist circumference, he qualified.
The eGDR has already been proven to be very precise in people with type 1 diabetes, said Dr. Zabala, and could be an “excellent tool to measure insulin resistance in a large patient population.”
Investigating the link between eGDR and first stroke risk
The aim of the study he presented was to see if changes in the eGDR were associated with changes in the risk of someone with T2D experiencing a first stroke, or dying from a cardiovascular or other cause.
An observational cohort was formed by first considering data on all adult patients with T2D who were logged in the Swedish National Diabetes Registry (NDR) during 2004-2016. Then anyone with a history of stroke, or with any missing data on the clinical variables needed to calculate the eGDR, were excluded.
This resulted in an overall population of 104,697 individuals, aged a mean of 63 years, who had developed T2D at around the age of 59 years. About 44% of the study population were women. The mean eGDR for the whole population was 5.6 mg/kg per min.
The study subjects were grouped according to four eGDR levels: 24,706 were in the lowest quartile of eGDR (less than 4 mg/kg per min), signifying the highest level of insulin resistance, and 18,762 were in the upper quartile of eGDR (greater than 8 mg/kg per min), signifying the lowest level of insulin resistance. The middle two groups had an eGDR between 4 and 6 mg/kg per min (40,187), and 6 and 8 mg/kg/min (21,042).
Data from the NDR were then combined with the Swedish Cause of Death register, the Swedish In-patient Care Diagnoses registry, and the Longitudinal Database for Health Insurance and Labour Market Studies (LISA) to determine the rates of stroke, ischemic stroke, hemorrhagic stroke, all-cause mortality, and cardiovascular mortality.
Increasing insulin resistance ups risk for stroke, death
After a median follow-up of 5.6 years, 4% (4,201) of the study population had had a stroke.
“We clearly see an increased occurrence of first-time stroke in the group with the lowest eGDR, indicating worst insulin resistance, in comparison with the group with the highest eGDR, indicating less insulin resistance,” Dr. Zabala reported.
After adjustment for potential confounding factors, including age at baseline, gender, diabetes duration, among other variables, the risk for stroke was lowest in those with a high eGDR value and highest for those with a low eGDR value.
Using individuals with the lowest eGDR (less than 4 mg/kg per min) and thus greatest risk of stroke as the reference, adjusted hazard ratios (aHR) for first-time stroke were: 0.60, 0.68, and 0.77 for those with an eGDR of greater than 8, 6-8, and 4-6 mg/kg per min, respectively.
The corresponding values for risk of ischemic stroke were 0.55, 0.68, and 0.75. Regarding hemorrhagic stroke, there was no statistically significant correlation between eGDR levels and stroke occurrence. This was due to the small number of cases recorded.
As for all-cause and cardiovascular mortality, a similar pattern was seen, with higher rates of death linked to increasing insulin resistance. Adjusted hazard ratios according to increasing insulin resistance (decreasing eGDR scores) for all-cause death were 0.68, 0.75, and 0.82 and for cardiovascular mortality were 0.65, 0.75, and 0.82.
A sensitivity analysis, using BMI instead of waist circumference to calculate the eGDR, showed a similar pattern, and “interestingly, a correlation between eGDR levels and risk of hemorrhagic stroke.” Dr. Zabala said.
Limitations and take-homes
Of course, this is an observational cohort study, so no conclusions on causality can be made and there are no data on the use of anti-diabetic treatments specifically. But there are strengths such as covering almost all adults with T2D in Sweden and a relatively long-follow-up time.
The findings suggest that “eGDR, which may reflect insulin resistance may be a useful risk marker for stroke and death in people with type 2 diabetes,” said Dr. Zabala.
“You had a very large cohort, and that certainly makes your results very valid,” observed Peter Novodvorsky, MUDr. (Hons), PhD, MRCP, a consultant diabetologist in Trenčín, Slovakia.
Dr. Novodvorsky, who chaired the session, picked up on the lack of information about how many people were taking newer diabetes drugs, such as the glucagon-like peptide 1 receptor antagonists and sodium glucose-lowering transport 2 inhibitors.
“As we all know, these might have protective effects which are not necessarily related to the glucose lowering or insulin resistance-lowering” effects, so could have influenced the results. In terms of how practical the eGDR is for clinical practice, Dr. Zabala observed in a press release: “eGDR could be used to help T2D patients better understand and manage their risk of stroke and death.
“It could also be of importance in research. In this era of personalized medicine, better stratification of type 2 diabetes patients will help optimize clinical trials and further vital research into treatment, diagnosis, care and prevention.”
The research was a collaboration between the Karolinska Institutet, Gothenburg University and the Swedish National Diabetes Registry. Dr. Zabala and coauthors reported having no conflicts of interest.
FROM EASD 2021
Dropping weight beneficial but some effects of obesity persist
It’s hard for people to completely escape a history of obesity, even when they later achieve a healthy weight.
American adults who once had obesity but later achieved and maintained a healthy body mass index (BMI) normalized some, but not all, of the excess clinical risk associated with obesity in a review of data collected from about 20,000 people during a series of eight NHANES surveys.
Maia P. Smith, MD, reported the findings at the virtual European Association for the Study of Diabetes (EASD) 2021 Annual Meeting.
“For some conditions, such as hypertension and dyslipidemia, the recovery [following a sharp drop in BMI] appears to be total, while for other conditions, like diabetes, the recovery is probabilistic. Some recover, but some don’t,” explained Dr. Smith in an interview.
“Weight loss reverses all, or essentially all, of the damage done by obesity in some people, but does not cause full reversal of the harm and does not fully resolve [type 2] diabetes in many others,” added Dr. Smith, an epidemiologist in the Department of Public Health and Preventive Medicine at St. George’s University, Grenada.
“The fact that ... analyses comparing formerly obese people to normal weight populations demonstrated improvement in population mean levels of hypertension and dyslipidemia is remarkable,” commented Rebecca T. Emeny, PhD, an epidemiologist at the Dartmouth Institute of Health Policy and Clinical Practice in Lebanon, New Hampshire, who was not involved with Dr. Smith’s study.
“The observation that the individuals who were able to maintain normal weight after past obesity were still at greater risk for diabetes compared with the normal weight group speaks to the recent discussion of obesity as a metabolic disorder rather than a problem of calories in and calories out,” said Dr. Emeny in an interview.
She cited a recent article that proposed a carbohydrate-insulin model for obesity in place of an energy-balance model. This, however, is still somewhat contentious.
Dr. Emeny also cautioned that “the results of this study compare populations. The design and analysis do not allow for interpretation of individual risk resulting from changes in weight.”
Those who formerly had obesity can reverse hypertension, dyslipidemia
The study by Dr. Smith and associates used data collected in the National Health and Nutrition Examination Survey (NHANES), which is performed every 2 years by the U.S. Centers for Disease Control and Prevention.
They used data from eight consecutive surveys starting in 1999-2000 and continuing through 2013-2014, yielding data from nearly 40,000 adults who were at least 20 years old.
In addition to the 326 people who formerly had obesity at some time previously during their life (BMI ≥30 kg/m2) but now had a healthy BMI, and 6,235 who were consistently at a healthy BMI, they also included 13,710 people who currently had obesity. They dropped the remaining survey participants who did not fit into one of these three categories.
The participants who formerly had obesity averaged 54 years old, compared with a mean age of 48 years among those with current obesity and 41 years among those who currently had a healthy BMI (who had never had obesity). The results showed no differences by sex, but those who formerly had obesity had a much higher smoking prevalence.
The people who reported a healthy BMI (18.5-24.9 kg/m2) after previously having obesity had current prevalence rates of hypertension and dyslipidemia that were, respectively, 8% and 13% higher than the prevalence rates among adults who consistently maintained a healthy BMI – differences that were not significant.
In contrast, people who had current BMIs that indicated obesity had prevalence rates of hypertension and dyslipidemia that were each a significant threefold higher than those with a healthy BMI.
The 326 respondents who formerly had obesity but now were at a healthy BMI had a threefold higher prevalence of diabetes than did the 6,235 who consistently had maintained a healthy BMI. This was substantially less than the over sevenfold higher prevalence of diabetes among those who currently had obesity compared with those who always had a healthy BMI.
All these analyses were adjusted for the potential confounders of age, sex, smoking history, and ethnicity.
‘Quitting’ obesity better than current obesity
The finding that reaching a healthy BMI after a period of obesity could reverse some but not all risks associated with obesity is reminiscent of the effects of smoking, noted Dr. Smith.
“Never is better than ever, but quitting,” or dropping weight to reach a healthy BMI, “is better than current,” she concluded.
But Dr. Emeny said this interpretation, “while motivating and catchy, places emphasis on individual responsibility and choice rather than on social circumstances.”
Social effects “must be considered when evaluating population-level disparities in obesity-related cardiometabolic risk,” cautioned Dr. Emeny.
“’Quitting’ obesity is much more complicated than individual choice or ability.”
Dr. Smith also conceded that her analyses did not correct for the possible confounding effects that changes in diet or physical activity may have had on the observations.
“Neither diet nor physical activity has a well-known summary measure that we could have included as an adjuster,” she explained.
Dr. Smith and Dr. Emeny have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s hard for people to completely escape a history of obesity, even when they later achieve a healthy weight.
American adults who once had obesity but later achieved and maintained a healthy body mass index (BMI) normalized some, but not all, of the excess clinical risk associated with obesity in a review of data collected from about 20,000 people during a series of eight NHANES surveys.
Maia P. Smith, MD, reported the findings at the virtual European Association for the Study of Diabetes (EASD) 2021 Annual Meeting.
“For some conditions, such as hypertension and dyslipidemia, the recovery [following a sharp drop in BMI] appears to be total, while for other conditions, like diabetes, the recovery is probabilistic. Some recover, but some don’t,” explained Dr. Smith in an interview.
“Weight loss reverses all, or essentially all, of the damage done by obesity in some people, but does not cause full reversal of the harm and does not fully resolve [type 2] diabetes in many others,” added Dr. Smith, an epidemiologist in the Department of Public Health and Preventive Medicine at St. George’s University, Grenada.
“The fact that ... analyses comparing formerly obese people to normal weight populations demonstrated improvement in population mean levels of hypertension and dyslipidemia is remarkable,” commented Rebecca T. Emeny, PhD, an epidemiologist at the Dartmouth Institute of Health Policy and Clinical Practice in Lebanon, New Hampshire, who was not involved with Dr. Smith’s study.
“The observation that the individuals who were able to maintain normal weight after past obesity were still at greater risk for diabetes compared with the normal weight group speaks to the recent discussion of obesity as a metabolic disorder rather than a problem of calories in and calories out,” said Dr. Emeny in an interview.
She cited a recent article that proposed a carbohydrate-insulin model for obesity in place of an energy-balance model. This, however, is still somewhat contentious.
Dr. Emeny also cautioned that “the results of this study compare populations. The design and analysis do not allow for interpretation of individual risk resulting from changes in weight.”
Those who formerly had obesity can reverse hypertension, dyslipidemia
The study by Dr. Smith and associates used data collected in the National Health and Nutrition Examination Survey (NHANES), which is performed every 2 years by the U.S. Centers for Disease Control and Prevention.
They used data from eight consecutive surveys starting in 1999-2000 and continuing through 2013-2014, yielding data from nearly 40,000 adults who were at least 20 years old.
In addition to the 326 people who formerly had obesity at some time previously during their life (BMI ≥30 kg/m2) but now had a healthy BMI, and 6,235 who were consistently at a healthy BMI, they also included 13,710 people who currently had obesity. They dropped the remaining survey participants who did not fit into one of these three categories.
The participants who formerly had obesity averaged 54 years old, compared with a mean age of 48 years among those with current obesity and 41 years among those who currently had a healthy BMI (who had never had obesity). The results showed no differences by sex, but those who formerly had obesity had a much higher smoking prevalence.
The people who reported a healthy BMI (18.5-24.9 kg/m2) after previously having obesity had current prevalence rates of hypertension and dyslipidemia that were, respectively, 8% and 13% higher than the prevalence rates among adults who consistently maintained a healthy BMI – differences that were not significant.
In contrast, people who had current BMIs that indicated obesity had prevalence rates of hypertension and dyslipidemia that were each a significant threefold higher than those with a healthy BMI.
The 326 respondents who formerly had obesity but now were at a healthy BMI had a threefold higher prevalence of diabetes than did the 6,235 who consistently had maintained a healthy BMI. This was substantially less than the over sevenfold higher prevalence of diabetes among those who currently had obesity compared with those who always had a healthy BMI.
All these analyses were adjusted for the potential confounders of age, sex, smoking history, and ethnicity.
‘Quitting’ obesity better than current obesity
The finding that reaching a healthy BMI after a period of obesity could reverse some but not all risks associated with obesity is reminiscent of the effects of smoking, noted Dr. Smith.
“Never is better than ever, but quitting,” or dropping weight to reach a healthy BMI, “is better than current,” she concluded.
But Dr. Emeny said this interpretation, “while motivating and catchy, places emphasis on individual responsibility and choice rather than on social circumstances.”
Social effects “must be considered when evaluating population-level disparities in obesity-related cardiometabolic risk,” cautioned Dr. Emeny.
“’Quitting’ obesity is much more complicated than individual choice or ability.”
Dr. Smith also conceded that her analyses did not correct for the possible confounding effects that changes in diet or physical activity may have had on the observations.
“Neither diet nor physical activity has a well-known summary measure that we could have included as an adjuster,” she explained.
Dr. Smith and Dr. Emeny have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s hard for people to completely escape a history of obesity, even when they later achieve a healthy weight.
American adults who once had obesity but later achieved and maintained a healthy body mass index (BMI) normalized some, but not all, of the excess clinical risk associated with obesity in a review of data collected from about 20,000 people during a series of eight NHANES surveys.
Maia P. Smith, MD, reported the findings at the virtual European Association for the Study of Diabetes (EASD) 2021 Annual Meeting.
“For some conditions, such as hypertension and dyslipidemia, the recovery [following a sharp drop in BMI] appears to be total, while for other conditions, like diabetes, the recovery is probabilistic. Some recover, but some don’t,” explained Dr. Smith in an interview.
“Weight loss reverses all, or essentially all, of the damage done by obesity in some people, but does not cause full reversal of the harm and does not fully resolve [type 2] diabetes in many others,” added Dr. Smith, an epidemiologist in the Department of Public Health and Preventive Medicine at St. George’s University, Grenada.
“The fact that ... analyses comparing formerly obese people to normal weight populations demonstrated improvement in population mean levels of hypertension and dyslipidemia is remarkable,” commented Rebecca T. Emeny, PhD, an epidemiologist at the Dartmouth Institute of Health Policy and Clinical Practice in Lebanon, New Hampshire, who was not involved with Dr. Smith’s study.
“The observation that the individuals who were able to maintain normal weight after past obesity were still at greater risk for diabetes compared with the normal weight group speaks to the recent discussion of obesity as a metabolic disorder rather than a problem of calories in and calories out,” said Dr. Emeny in an interview.
She cited a recent article that proposed a carbohydrate-insulin model for obesity in place of an energy-balance model. This, however, is still somewhat contentious.
Dr. Emeny also cautioned that “the results of this study compare populations. The design and analysis do not allow for interpretation of individual risk resulting from changes in weight.”
Those who formerly had obesity can reverse hypertension, dyslipidemia
The study by Dr. Smith and associates used data collected in the National Health and Nutrition Examination Survey (NHANES), which is performed every 2 years by the U.S. Centers for Disease Control and Prevention.
They used data from eight consecutive surveys starting in 1999-2000 and continuing through 2013-2014, yielding data from nearly 40,000 adults who were at least 20 years old.
In addition to the 326 people who formerly had obesity at some time previously during their life (BMI ≥30 kg/m2) but now had a healthy BMI, and 6,235 who were consistently at a healthy BMI, they also included 13,710 people who currently had obesity. They dropped the remaining survey participants who did not fit into one of these three categories.
The participants who formerly had obesity averaged 54 years old, compared with a mean age of 48 years among those with current obesity and 41 years among those who currently had a healthy BMI (who had never had obesity). The results showed no differences by sex, but those who formerly had obesity had a much higher smoking prevalence.
The people who reported a healthy BMI (18.5-24.9 kg/m2) after previously having obesity had current prevalence rates of hypertension and dyslipidemia that were, respectively, 8% and 13% higher than the prevalence rates among adults who consistently maintained a healthy BMI – differences that were not significant.
In contrast, people who had current BMIs that indicated obesity had prevalence rates of hypertension and dyslipidemia that were each a significant threefold higher than those with a healthy BMI.
The 326 respondents who formerly had obesity but now were at a healthy BMI had a threefold higher prevalence of diabetes than did the 6,235 who consistently had maintained a healthy BMI. This was substantially less than the over sevenfold higher prevalence of diabetes among those who currently had obesity compared with those who always had a healthy BMI.
All these analyses were adjusted for the potential confounders of age, sex, smoking history, and ethnicity.
‘Quitting’ obesity better than current obesity
The finding that reaching a healthy BMI after a period of obesity could reverse some but not all risks associated with obesity is reminiscent of the effects of smoking, noted Dr. Smith.
“Never is better than ever, but quitting,” or dropping weight to reach a healthy BMI, “is better than current,” she concluded.
But Dr. Emeny said this interpretation, “while motivating and catchy, places emphasis on individual responsibility and choice rather than on social circumstances.”
Social effects “must be considered when evaluating population-level disparities in obesity-related cardiometabolic risk,” cautioned Dr. Emeny.
“’Quitting’ obesity is much more complicated than individual choice or ability.”
Dr. Smith also conceded that her analyses did not correct for the possible confounding effects that changes in diet or physical activity may have had on the observations.
“Neither diet nor physical activity has a well-known summary measure that we could have included as an adjuster,” she explained.
Dr. Smith and Dr. Emeny have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
from easd 2021
‘Push the bar higher’: New statement on type 1 diabetes in adults
A newly published consensus statement on the management of type 1 diabetes in adults addresses the unique clinical needs of the population compared with those of children with type 1 diabetes or adults with type 2 diabetes.
“The focus on adults is kind of new and it is important. ... I do think it’s a bit of a forgotten population. Whenever we talk about diabetes in adults it’s assumed to be about type 2,” document coauthor M. Sue Kirkman, MD, said in an interview.
The document covers diagnosis of type 1 diabetes, goals and targets, schedule of care, self-management education and lifestyle, glucose monitoring, insulin therapy, hypoglycemia, psychosocial care, diabetic ketoacidosis (DKA), pancreas transplant/islet cell transplantation, adjunctive therapies, special populations (pregnant, older, hospitalized), and emergent and future perspectives.
Initially presented in draft form in June at the American Diabetes Association (ADA) 81st scientific sessions, the final version of the joint ADA/EASD statement was presented Oct. 1 at the annual meeting of the European Association for the Study of Diabetes and simultaneously published in Diabetologia and Diabetes Care.
“We are aware of the many and rapid advances in the diagnosis and treatment of type 1 diabetes ... However, despite these advances, there is also a growing recognition of the psychosocial burden of living with type 1 diabetes,” writing group cochair Richard I.G. Holt, MB BChir, PhD, professor of diabetes and endocrinology at the University of Southampton, England, said when introducing the 90-minute EASD session.
“Although there is guidance for the management of type 1 diabetes, the aim of this report is to highlight the major areas that health care professionals should consider when managing adults with type 1 diabetes,” he added.
Noting that the joint EASD/ADA consensus report on type 2 diabetes has been “highly influential,” Dr. Holt said, “EASD and ADA recognized the need to develop a comparable consensus report specifically addressing type 1 diabetes.”
The overriding goals, Dr. Holt said, are to “support people with type 1 diabetes to live a long and healthy life” with four specific strategies: delivery of insulin to keep glucose levels as close to target as possible to prevent complications while minimizing hypoglycemia and preventing DKA; managing cardiovascular risk factors; minimizing psychosocial burden; and promoting psychological well-being.
Diagnostic algorithm
Another coauthor, J. Hans de Vries, MD, PhD, professor of internal medicine at the University of Amsterdam, explained the recommended approach to distinguishing type 1 diabetes from type 2 diabetes or monogenic diabetes in adults, which is often a clinical challenge.
This also was the topic prompting the most questions during the EASD session.
“Especially in adults, misdiagnosis of type of diabetes is common, occurring in up to 40% of patients diagnosed after the age of 30 years,” Dr. de Vries said.
Among the many reasons for the confusion are that C-peptide levels, a reflection of endogenous insulin secretion, can still be relatively high at the time of clinical onset of type 1 diabetes, but islet antibodies don’t have 100% positive predictive value.
Obesity and type 2 diabetes are increasingly seen at younger ages, and DKA can occur in type 2 diabetes (“ketosis-prone”). In addition, monogenic forms of diabetes can be disguised as type 1 diabetes.
“So, we thought there was a need for a diagnostic algorithm,” Dr. de Vries said, adding that the algorithm – displayed as a graphic in the statement – is only for adults in whom type 1 diabetes is suspected, not other types. Also, it’s based on data from White European populations.
The first step is to test islet autoantibodies. If positive, the diagnosis of type 1 diabetes can be made. If negative and the person is younger than 35 years and without signs of type 2 diabetes, testing C-peptide is advised. If that’s below 200 pmol/L, type 1 diabetes is the diagnosis. If above 200 pmol/L, genetic testing for monogenic diabetes is advised. If there are signs of type 2 diabetes and/or the person is over age 35, type 2 diabetes is the most likely diagnosis.
And if uncertainty remains, the recommendation is to try noninsulin therapy and retest C-peptide again in 3 years, as by that time it will be below 200 pmol/L in a person with type 1 diabetes.
Dr. Kirkman commented regarding the algorithm: “It’s very much from a European population perspective. In some ways that’s a limitation, especially in the U.S. where the population is diverse, but I do think it’s still useful to help guide people through how to think about somebody who presents as an adult where it’s not obviously type 2 or type 1 ... There is a lot of in-between stuff.”
Psychosocial support: Essential but often overlooked
Frank J. Snoek, PhD, professor of psychology at Amsterdam University Medical Centers, Vrije Universiteit, presented the section on behavioral and psychosocial care. He pointed out that diabetes-related emotional distress is reported by 20%-40% of adults with type 1 diabetes, and that the risk of such distress is especially high at the time of diagnosis and when complications develop.
About 15% of people with type 1 diabetes have depression, which is linked to elevated A1c levels, increased complication risk, and mortality. Anxiety also is very common and linked with diabetes-specific fears including hypoglycemia. Eating disorders are more prevalent among people with type 1 diabetes than in the general population and can further complicate diabetes management.
Recommendations include periodic evaluation of psychological health and social barriers to self-management and having clear referral pathways and access to psychological or psychiatric care for individuals in need. “All members of the diabetes care team have a responsibility when it comes to offering psychosocial support as part of ongoing diabetes care and education.”
Dr. Kirkman had identified this section as noteworthy: “I think the focus on psychosocial care and making that an ongoing part of diabetes care and assessment is important.”
More data needed on diets, many other areas
During the discussion, several attendees asked about low-carbohydrate diets, embraced by many individuals with type 1 diabetes.
The document states: “While low-carbohydrate and very low-carbohydrate eating patterns have become increasingly popular and reduce A1c levels in the short term, it is important to incorporate these in conjunction with healthy eating guidelines. Additional components of the meal, including high fat and/or high protein, may contribute to delayed hyperglycemia and the need for insulin dose adjustments. Since this is highly variable between individuals, postprandial glucose measurements for up to 3 hours or more may be needed to determine initial dose adjustments.”
Beyond that, Tomasz Klupa, MD, PhD, of the department of metabolic diseases, Jagiellonian University, Krakow, Poland, responded: “We don’t have much data on low-carb diets in type 1 diabetes. ... Compliance to those diets is pretty poor. We don’t have long-term follow-up and the studies are simply not conclusive. Initial results do show reductions in body weight and A1c, but with time the compliance goes down dramatically.”
“Certainly, when we think of low-carb diets, we have to meet our patients where they are,” said Amy Hess-Fischl, a nutritionist and certified diabetes care and education specialist at the University of Chicago. “We don’t have enough data to really say there’s positive long-term evidence. But we can find a happy medium to find some benefits in glycemic and weight control. ... It’s really that collaboration with that person to identify what’s going to work for them in a healthy way.”
The EASD session concluded with writing group cochair Anne L. Peters, MD, director of clinical diabetes programs at the University of Southern California, Los Angeles, summing up the many other knowledge gaps, including personalizing use of diabetes technology, the problems of health disparities and lack of access to care, and the feasibility of prevention and/or cure.
She observed: “There is no one-size-fits-all approach to diabetes care, and the more we can individualize our approaches, the more successful we are likely to be. ... Hopefully this consensus statement has pushed the bar a bit higher, telling the powers that be that people with type 1 diabetes need and deserve the best.
“We have a very long way to go before all of our patients reach their goals and health equity is achieved. ... We need to provide each and every person the access to the care we describe in this consensus statement, so that all can prosper and thrive and look forward to a long and healthy life lived with type 1 diabetes.”
Dr. Holt has financial relationships with Novo Nordisk, Abbott, Eli Lilly, Otsuka, and Roche. Dr. de Vries has financial relationships with Afon, Eli Lilly, Novo Nordisk, Adocia, and Zealand Pharma. Ms. Hess-Fischl has financial relationships with Abbott Diabetes Care and Xeris. Dr. Klupa has financial relationships with numerous drug and device companies. Dr. Snoek has financial relationships with Abbott, Eli Lilly, Sanofi, and Novo Nordisk. Dr. Peters has financial relationships with Abbott Diabetes Care, Dexcom, Eli Lilly, Insulet, Novo Nordisk, Medscape, and Zealand Pharmaceuticals. She holds stock options in Omada Health and Livongo and is a special government employee of the Food and Drug Administration.
A version of this article first appeared on Medscape.com.
A newly published consensus statement on the management of type 1 diabetes in adults addresses the unique clinical needs of the population compared with those of children with type 1 diabetes or adults with type 2 diabetes.
“The focus on adults is kind of new and it is important. ... I do think it’s a bit of a forgotten population. Whenever we talk about diabetes in adults it’s assumed to be about type 2,” document coauthor M. Sue Kirkman, MD, said in an interview.
The document covers diagnosis of type 1 diabetes, goals and targets, schedule of care, self-management education and lifestyle, glucose monitoring, insulin therapy, hypoglycemia, psychosocial care, diabetic ketoacidosis (DKA), pancreas transplant/islet cell transplantation, adjunctive therapies, special populations (pregnant, older, hospitalized), and emergent and future perspectives.
Initially presented in draft form in June at the American Diabetes Association (ADA) 81st scientific sessions, the final version of the joint ADA/EASD statement was presented Oct. 1 at the annual meeting of the European Association for the Study of Diabetes and simultaneously published in Diabetologia and Diabetes Care.
“We are aware of the many and rapid advances in the diagnosis and treatment of type 1 diabetes ... However, despite these advances, there is also a growing recognition of the psychosocial burden of living with type 1 diabetes,” writing group cochair Richard I.G. Holt, MB BChir, PhD, professor of diabetes and endocrinology at the University of Southampton, England, said when introducing the 90-minute EASD session.
“Although there is guidance for the management of type 1 diabetes, the aim of this report is to highlight the major areas that health care professionals should consider when managing adults with type 1 diabetes,” he added.
Noting that the joint EASD/ADA consensus report on type 2 diabetes has been “highly influential,” Dr. Holt said, “EASD and ADA recognized the need to develop a comparable consensus report specifically addressing type 1 diabetes.”
The overriding goals, Dr. Holt said, are to “support people with type 1 diabetes to live a long and healthy life” with four specific strategies: delivery of insulin to keep glucose levels as close to target as possible to prevent complications while minimizing hypoglycemia and preventing DKA; managing cardiovascular risk factors; minimizing psychosocial burden; and promoting psychological well-being.
Diagnostic algorithm
Another coauthor, J. Hans de Vries, MD, PhD, professor of internal medicine at the University of Amsterdam, explained the recommended approach to distinguishing type 1 diabetes from type 2 diabetes or monogenic diabetes in adults, which is often a clinical challenge.
This also was the topic prompting the most questions during the EASD session.
“Especially in adults, misdiagnosis of type of diabetes is common, occurring in up to 40% of patients diagnosed after the age of 30 years,” Dr. de Vries said.
Among the many reasons for the confusion are that C-peptide levels, a reflection of endogenous insulin secretion, can still be relatively high at the time of clinical onset of type 1 diabetes, but islet antibodies don’t have 100% positive predictive value.
Obesity and type 2 diabetes are increasingly seen at younger ages, and DKA can occur in type 2 diabetes (“ketosis-prone”). In addition, monogenic forms of diabetes can be disguised as type 1 diabetes.
“So, we thought there was a need for a diagnostic algorithm,” Dr. de Vries said, adding that the algorithm – displayed as a graphic in the statement – is only for adults in whom type 1 diabetes is suspected, not other types. Also, it’s based on data from White European populations.
The first step is to test islet autoantibodies. If positive, the diagnosis of type 1 diabetes can be made. If negative and the person is younger than 35 years and without signs of type 2 diabetes, testing C-peptide is advised. If that’s below 200 pmol/L, type 1 diabetes is the diagnosis. If above 200 pmol/L, genetic testing for monogenic diabetes is advised. If there are signs of type 2 diabetes and/or the person is over age 35, type 2 diabetes is the most likely diagnosis.
And if uncertainty remains, the recommendation is to try noninsulin therapy and retest C-peptide again in 3 years, as by that time it will be below 200 pmol/L in a person with type 1 diabetes.
Dr. Kirkman commented regarding the algorithm: “It’s very much from a European population perspective. In some ways that’s a limitation, especially in the U.S. where the population is diverse, but I do think it’s still useful to help guide people through how to think about somebody who presents as an adult where it’s not obviously type 2 or type 1 ... There is a lot of in-between stuff.”
Psychosocial support: Essential but often overlooked
Frank J. Snoek, PhD, professor of psychology at Amsterdam University Medical Centers, Vrije Universiteit, presented the section on behavioral and psychosocial care. He pointed out that diabetes-related emotional distress is reported by 20%-40% of adults with type 1 diabetes, and that the risk of such distress is especially high at the time of diagnosis and when complications develop.
About 15% of people with type 1 diabetes have depression, which is linked to elevated A1c levels, increased complication risk, and mortality. Anxiety also is very common and linked with diabetes-specific fears including hypoglycemia. Eating disorders are more prevalent among people with type 1 diabetes than in the general population and can further complicate diabetes management.
Recommendations include periodic evaluation of psychological health and social barriers to self-management and having clear referral pathways and access to psychological or psychiatric care for individuals in need. “All members of the diabetes care team have a responsibility when it comes to offering psychosocial support as part of ongoing diabetes care and education.”
Dr. Kirkman had identified this section as noteworthy: “I think the focus on psychosocial care and making that an ongoing part of diabetes care and assessment is important.”
More data needed on diets, many other areas
During the discussion, several attendees asked about low-carbohydrate diets, embraced by many individuals with type 1 diabetes.
The document states: “While low-carbohydrate and very low-carbohydrate eating patterns have become increasingly popular and reduce A1c levels in the short term, it is important to incorporate these in conjunction with healthy eating guidelines. Additional components of the meal, including high fat and/or high protein, may contribute to delayed hyperglycemia and the need for insulin dose adjustments. Since this is highly variable between individuals, postprandial glucose measurements for up to 3 hours or more may be needed to determine initial dose adjustments.”
Beyond that, Tomasz Klupa, MD, PhD, of the department of metabolic diseases, Jagiellonian University, Krakow, Poland, responded: “We don’t have much data on low-carb diets in type 1 diabetes. ... Compliance to those diets is pretty poor. We don’t have long-term follow-up and the studies are simply not conclusive. Initial results do show reductions in body weight and A1c, but with time the compliance goes down dramatically.”
“Certainly, when we think of low-carb diets, we have to meet our patients where they are,” said Amy Hess-Fischl, a nutritionist and certified diabetes care and education specialist at the University of Chicago. “We don’t have enough data to really say there’s positive long-term evidence. But we can find a happy medium to find some benefits in glycemic and weight control. ... It’s really that collaboration with that person to identify what’s going to work for them in a healthy way.”
The EASD session concluded with writing group cochair Anne L. Peters, MD, director of clinical diabetes programs at the University of Southern California, Los Angeles, summing up the many other knowledge gaps, including personalizing use of diabetes technology, the problems of health disparities and lack of access to care, and the feasibility of prevention and/or cure.
She observed: “There is no one-size-fits-all approach to diabetes care, and the more we can individualize our approaches, the more successful we are likely to be. ... Hopefully this consensus statement has pushed the bar a bit higher, telling the powers that be that people with type 1 diabetes need and deserve the best.
“We have a very long way to go before all of our patients reach their goals and health equity is achieved. ... We need to provide each and every person the access to the care we describe in this consensus statement, so that all can prosper and thrive and look forward to a long and healthy life lived with type 1 diabetes.”
Dr. Holt has financial relationships with Novo Nordisk, Abbott, Eli Lilly, Otsuka, and Roche. Dr. de Vries has financial relationships with Afon, Eli Lilly, Novo Nordisk, Adocia, and Zealand Pharma. Ms. Hess-Fischl has financial relationships with Abbott Diabetes Care and Xeris. Dr. Klupa has financial relationships with numerous drug and device companies. Dr. Snoek has financial relationships with Abbott, Eli Lilly, Sanofi, and Novo Nordisk. Dr. Peters has financial relationships with Abbott Diabetes Care, Dexcom, Eli Lilly, Insulet, Novo Nordisk, Medscape, and Zealand Pharmaceuticals. She holds stock options in Omada Health and Livongo and is a special government employee of the Food and Drug Administration.
A version of this article first appeared on Medscape.com.
A newly published consensus statement on the management of type 1 diabetes in adults addresses the unique clinical needs of the population compared with those of children with type 1 diabetes or adults with type 2 diabetes.
“The focus on adults is kind of new and it is important. ... I do think it’s a bit of a forgotten population. Whenever we talk about diabetes in adults it’s assumed to be about type 2,” document coauthor M. Sue Kirkman, MD, said in an interview.
The document covers diagnosis of type 1 diabetes, goals and targets, schedule of care, self-management education and lifestyle, glucose monitoring, insulin therapy, hypoglycemia, psychosocial care, diabetic ketoacidosis (DKA), pancreas transplant/islet cell transplantation, adjunctive therapies, special populations (pregnant, older, hospitalized), and emergent and future perspectives.
Initially presented in draft form in June at the American Diabetes Association (ADA) 81st scientific sessions, the final version of the joint ADA/EASD statement was presented Oct. 1 at the annual meeting of the European Association for the Study of Diabetes and simultaneously published in Diabetologia and Diabetes Care.
“We are aware of the many and rapid advances in the diagnosis and treatment of type 1 diabetes ... However, despite these advances, there is also a growing recognition of the psychosocial burden of living with type 1 diabetes,” writing group cochair Richard I.G. Holt, MB BChir, PhD, professor of diabetes and endocrinology at the University of Southampton, England, said when introducing the 90-minute EASD session.
“Although there is guidance for the management of type 1 diabetes, the aim of this report is to highlight the major areas that health care professionals should consider when managing adults with type 1 diabetes,” he added.
Noting that the joint EASD/ADA consensus report on type 2 diabetes has been “highly influential,” Dr. Holt said, “EASD and ADA recognized the need to develop a comparable consensus report specifically addressing type 1 diabetes.”
The overriding goals, Dr. Holt said, are to “support people with type 1 diabetes to live a long and healthy life” with four specific strategies: delivery of insulin to keep glucose levels as close to target as possible to prevent complications while minimizing hypoglycemia and preventing DKA; managing cardiovascular risk factors; minimizing psychosocial burden; and promoting psychological well-being.
Diagnostic algorithm
Another coauthor, J. Hans de Vries, MD, PhD, professor of internal medicine at the University of Amsterdam, explained the recommended approach to distinguishing type 1 diabetes from type 2 diabetes or monogenic diabetes in adults, which is often a clinical challenge.
This also was the topic prompting the most questions during the EASD session.
“Especially in adults, misdiagnosis of type of diabetes is common, occurring in up to 40% of patients diagnosed after the age of 30 years,” Dr. de Vries said.
Among the many reasons for the confusion are that C-peptide levels, a reflection of endogenous insulin secretion, can still be relatively high at the time of clinical onset of type 1 diabetes, but islet antibodies don’t have 100% positive predictive value.
Obesity and type 2 diabetes are increasingly seen at younger ages, and DKA can occur in type 2 diabetes (“ketosis-prone”). In addition, monogenic forms of diabetes can be disguised as type 1 diabetes.
“So, we thought there was a need for a diagnostic algorithm,” Dr. de Vries said, adding that the algorithm – displayed as a graphic in the statement – is only for adults in whom type 1 diabetes is suspected, not other types. Also, it’s based on data from White European populations.
The first step is to test islet autoantibodies. If positive, the diagnosis of type 1 diabetes can be made. If negative and the person is younger than 35 years and without signs of type 2 diabetes, testing C-peptide is advised. If that’s below 200 pmol/L, type 1 diabetes is the diagnosis. If above 200 pmol/L, genetic testing for monogenic diabetes is advised. If there are signs of type 2 diabetes and/or the person is over age 35, type 2 diabetes is the most likely diagnosis.
And if uncertainty remains, the recommendation is to try noninsulin therapy and retest C-peptide again in 3 years, as by that time it will be below 200 pmol/L in a person with type 1 diabetes.
Dr. Kirkman commented regarding the algorithm: “It’s very much from a European population perspective. In some ways that’s a limitation, especially in the U.S. where the population is diverse, but I do think it’s still useful to help guide people through how to think about somebody who presents as an adult where it’s not obviously type 2 or type 1 ... There is a lot of in-between stuff.”
Psychosocial support: Essential but often overlooked
Frank J. Snoek, PhD, professor of psychology at Amsterdam University Medical Centers, Vrije Universiteit, presented the section on behavioral and psychosocial care. He pointed out that diabetes-related emotional distress is reported by 20%-40% of adults with type 1 diabetes, and that the risk of such distress is especially high at the time of diagnosis and when complications develop.
About 15% of people with type 1 diabetes have depression, which is linked to elevated A1c levels, increased complication risk, and mortality. Anxiety also is very common and linked with diabetes-specific fears including hypoglycemia. Eating disorders are more prevalent among people with type 1 diabetes than in the general population and can further complicate diabetes management.
Recommendations include periodic evaluation of psychological health and social barriers to self-management and having clear referral pathways and access to psychological or psychiatric care for individuals in need. “All members of the diabetes care team have a responsibility when it comes to offering psychosocial support as part of ongoing diabetes care and education.”
Dr. Kirkman had identified this section as noteworthy: “I think the focus on psychosocial care and making that an ongoing part of diabetes care and assessment is important.”
More data needed on diets, many other areas
During the discussion, several attendees asked about low-carbohydrate diets, embraced by many individuals with type 1 diabetes.
The document states: “While low-carbohydrate and very low-carbohydrate eating patterns have become increasingly popular and reduce A1c levels in the short term, it is important to incorporate these in conjunction with healthy eating guidelines. Additional components of the meal, including high fat and/or high protein, may contribute to delayed hyperglycemia and the need for insulin dose adjustments. Since this is highly variable between individuals, postprandial glucose measurements for up to 3 hours or more may be needed to determine initial dose adjustments.”
Beyond that, Tomasz Klupa, MD, PhD, of the department of metabolic diseases, Jagiellonian University, Krakow, Poland, responded: “We don’t have much data on low-carb diets in type 1 diabetes. ... Compliance to those diets is pretty poor. We don’t have long-term follow-up and the studies are simply not conclusive. Initial results do show reductions in body weight and A1c, but with time the compliance goes down dramatically.”
“Certainly, when we think of low-carb diets, we have to meet our patients where they are,” said Amy Hess-Fischl, a nutritionist and certified diabetes care and education specialist at the University of Chicago. “We don’t have enough data to really say there’s positive long-term evidence. But we can find a happy medium to find some benefits in glycemic and weight control. ... It’s really that collaboration with that person to identify what’s going to work for them in a healthy way.”
The EASD session concluded with writing group cochair Anne L. Peters, MD, director of clinical diabetes programs at the University of Southern California, Los Angeles, summing up the many other knowledge gaps, including personalizing use of diabetes technology, the problems of health disparities and lack of access to care, and the feasibility of prevention and/or cure.
She observed: “There is no one-size-fits-all approach to diabetes care, and the more we can individualize our approaches, the more successful we are likely to be. ... Hopefully this consensus statement has pushed the bar a bit higher, telling the powers that be that people with type 1 diabetes need and deserve the best.
“We have a very long way to go before all of our patients reach their goals and health equity is achieved. ... We need to provide each and every person the access to the care we describe in this consensus statement, so that all can prosper and thrive and look forward to a long and healthy life lived with type 1 diabetes.”
Dr. Holt has financial relationships with Novo Nordisk, Abbott, Eli Lilly, Otsuka, and Roche. Dr. de Vries has financial relationships with Afon, Eli Lilly, Novo Nordisk, Adocia, and Zealand Pharma. Ms. Hess-Fischl has financial relationships with Abbott Diabetes Care and Xeris. Dr. Klupa has financial relationships with numerous drug and device companies. Dr. Snoek has financial relationships with Abbott, Eli Lilly, Sanofi, and Novo Nordisk. Dr. Peters has financial relationships with Abbott Diabetes Care, Dexcom, Eli Lilly, Insulet, Novo Nordisk, Medscape, and Zealand Pharmaceuticals. She holds stock options in Omada Health and Livongo and is a special government employee of the Food and Drug Administration.
A version of this article first appeared on Medscape.com.
FROM EASD 2021
Men die more often than women after bariatric surgery
Men had a much higher rate of death following bariatric surgery performed in Austria during 2010-2018, compared with women in a retrospective analysis of nearly 20,000 patients based on health insurance records.
The reason may be that men undergoing bariatric surgery have “worse overall health at the time of surgery” than women, Hannes Beiglböck, MD, suggested at the annual meeting of the European Association for the Study of Diabetes.
The results also showed that “men tend to be older [at time of surgery] and that might have the biggest impact on outcomes after bariatric surgery,” said Dr. Beiglböck, a researcher in the division of endocrinology and metabolism at the Medical University of Vienna.
The findings confirm those of prior studies in various worldwide locations, he noted; that is, men undergoing bariatric surgery tend to be older than women and have more comorbidities and perioperative mortality.
Dr. Beiglböck also highlighted earlier reports that indicate “profound” sex-specific differences in why patients undergo bariatric surgery, with men often driven by a medical condition and women motivated by appearance.
Hence, for men, it may be important to focus on preoperative counseling to try to get them to think about bariatric surgery earlier, “which may improve their postsurgical mortality rate,” he observed.
Nearly threefold higher mortality among men
Dr. Beiglböck and associates used medical claims data filed with the Austrian health system, which includes nearly all residents. In 2010-2018, 19,901 Austrian patients underwent bariatric surgery, and researchers tracked their outcomes for a median of 5.4 years, through April 2020.
During the 9-year period, 74% of patients who underwent bariatric surgery were women, again, a finding consistent with prior reports from other countries.
The 5,220 men were an average of 41.8 years old, with 65% undergoing gastric bypass and 30% gastric banding. The 14,681 women were an average of 40.1 years old, with 70% undergoing gastric bypass and 22% gastric banding.
During follow-up, 367 patients (1.8%) died. Among men, the overall mortality rate was 2.6-fold higher, compared with women (1.3% vs. 3.4%) and average mortality per year was 2.8-fold higher (0.64% vs. 0.24%).
The rate of death on the day of surgery among men also substantially exceeded that of women (0.29% vs. 0.05%), as did death within 30 days of surgery (0.48% vs. 0.08%). All of these between-sex differences were significant.
Baseline prevalence of four categories of comorbidities and how these differed by sex among patients who died during follow-up was also examined. Underlying cardiovascular disease was prevalent in 299 patients (81% of the deceased group), 200 (54%) had a psychiatric disorder, 138 (38%) had diabetes, and 132 (36%) had a malignancy.
The prevalence of cardiovascular disease and psychiatric disorders was roughly the same in men and women. Men had a significantly higher prevalence of diabetes, and a higher proportion of women had a malignancy.
Consistent with U.S. studies
A U.S. report in 2015 documented a higher prevalence of comorbidities and more severe illness among men undergoing bariatric surgery, compared with women, noted session chair Zhila Semnani-Azad, PhD, a researcher in the department of nutrition at Harvard School of Public Health in Boston.
“I think the [Austrian] data presented have relevance to the U.S. population,” Dr. Semnani-Azad said in an interview.
“The main limitation of these univariate analyses is they don’t account for potential confounding variables that could affect the association, such as lifestyle variables, age, and family history. There is always potential for other variables” to influence apparent sex-specific associations, she commented. Another limitation is the small total number of deaths analyzed, at 367.
“These results are a good starting point for future studies. More work is needed to better understand the impact of comorbidities and sex on postsurgical mortality,” Dr. Semnani-Azad concluded.
Dr. Beiglböck and Dr. Semnani-Azad have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Men had a much higher rate of death following bariatric surgery performed in Austria during 2010-2018, compared with women in a retrospective analysis of nearly 20,000 patients based on health insurance records.
The reason may be that men undergoing bariatric surgery have “worse overall health at the time of surgery” than women, Hannes Beiglböck, MD, suggested at the annual meeting of the European Association for the Study of Diabetes.
The results also showed that “men tend to be older [at time of surgery] and that might have the biggest impact on outcomes after bariatric surgery,” said Dr. Beiglböck, a researcher in the division of endocrinology and metabolism at the Medical University of Vienna.
The findings confirm those of prior studies in various worldwide locations, he noted; that is, men undergoing bariatric surgery tend to be older than women and have more comorbidities and perioperative mortality.
Dr. Beiglböck also highlighted earlier reports that indicate “profound” sex-specific differences in why patients undergo bariatric surgery, with men often driven by a medical condition and women motivated by appearance.
Hence, for men, it may be important to focus on preoperative counseling to try to get them to think about bariatric surgery earlier, “which may improve their postsurgical mortality rate,” he observed.
Nearly threefold higher mortality among men
Dr. Beiglböck and associates used medical claims data filed with the Austrian health system, which includes nearly all residents. In 2010-2018, 19,901 Austrian patients underwent bariatric surgery, and researchers tracked their outcomes for a median of 5.4 years, through April 2020.
During the 9-year period, 74% of patients who underwent bariatric surgery were women, again, a finding consistent with prior reports from other countries.
The 5,220 men were an average of 41.8 years old, with 65% undergoing gastric bypass and 30% gastric banding. The 14,681 women were an average of 40.1 years old, with 70% undergoing gastric bypass and 22% gastric banding.
During follow-up, 367 patients (1.8%) died. Among men, the overall mortality rate was 2.6-fold higher, compared with women (1.3% vs. 3.4%) and average mortality per year was 2.8-fold higher (0.64% vs. 0.24%).
The rate of death on the day of surgery among men also substantially exceeded that of women (0.29% vs. 0.05%), as did death within 30 days of surgery (0.48% vs. 0.08%). All of these between-sex differences were significant.
Baseline prevalence of four categories of comorbidities and how these differed by sex among patients who died during follow-up was also examined. Underlying cardiovascular disease was prevalent in 299 patients (81% of the deceased group), 200 (54%) had a psychiatric disorder, 138 (38%) had diabetes, and 132 (36%) had a malignancy.
The prevalence of cardiovascular disease and psychiatric disorders was roughly the same in men and women. Men had a significantly higher prevalence of diabetes, and a higher proportion of women had a malignancy.
Consistent with U.S. studies
A U.S. report in 2015 documented a higher prevalence of comorbidities and more severe illness among men undergoing bariatric surgery, compared with women, noted session chair Zhila Semnani-Azad, PhD, a researcher in the department of nutrition at Harvard School of Public Health in Boston.
“I think the [Austrian] data presented have relevance to the U.S. population,” Dr. Semnani-Azad said in an interview.
“The main limitation of these univariate analyses is they don’t account for potential confounding variables that could affect the association, such as lifestyle variables, age, and family history. There is always potential for other variables” to influence apparent sex-specific associations, she commented. Another limitation is the small total number of deaths analyzed, at 367.
“These results are a good starting point for future studies. More work is needed to better understand the impact of comorbidities and sex on postsurgical mortality,” Dr. Semnani-Azad concluded.
Dr. Beiglböck and Dr. Semnani-Azad have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Men had a much higher rate of death following bariatric surgery performed in Austria during 2010-2018, compared with women in a retrospective analysis of nearly 20,000 patients based on health insurance records.
The reason may be that men undergoing bariatric surgery have “worse overall health at the time of surgery” than women, Hannes Beiglböck, MD, suggested at the annual meeting of the European Association for the Study of Diabetes.
The results also showed that “men tend to be older [at time of surgery] and that might have the biggest impact on outcomes after bariatric surgery,” said Dr. Beiglböck, a researcher in the division of endocrinology and metabolism at the Medical University of Vienna.
The findings confirm those of prior studies in various worldwide locations, he noted; that is, men undergoing bariatric surgery tend to be older than women and have more comorbidities and perioperative mortality.
Dr. Beiglböck also highlighted earlier reports that indicate “profound” sex-specific differences in why patients undergo bariatric surgery, with men often driven by a medical condition and women motivated by appearance.
Hence, for men, it may be important to focus on preoperative counseling to try to get them to think about bariatric surgery earlier, “which may improve their postsurgical mortality rate,” he observed.
Nearly threefold higher mortality among men
Dr. Beiglböck and associates used medical claims data filed with the Austrian health system, which includes nearly all residents. In 2010-2018, 19,901 Austrian patients underwent bariatric surgery, and researchers tracked their outcomes for a median of 5.4 years, through April 2020.
During the 9-year period, 74% of patients who underwent bariatric surgery were women, again, a finding consistent with prior reports from other countries.
The 5,220 men were an average of 41.8 years old, with 65% undergoing gastric bypass and 30% gastric banding. The 14,681 women were an average of 40.1 years old, with 70% undergoing gastric bypass and 22% gastric banding.
During follow-up, 367 patients (1.8%) died. Among men, the overall mortality rate was 2.6-fold higher, compared with women (1.3% vs. 3.4%) and average mortality per year was 2.8-fold higher (0.64% vs. 0.24%).
The rate of death on the day of surgery among men also substantially exceeded that of women (0.29% vs. 0.05%), as did death within 30 days of surgery (0.48% vs. 0.08%). All of these between-sex differences were significant.
Baseline prevalence of four categories of comorbidities and how these differed by sex among patients who died during follow-up was also examined. Underlying cardiovascular disease was prevalent in 299 patients (81% of the deceased group), 200 (54%) had a psychiatric disorder, 138 (38%) had diabetes, and 132 (36%) had a malignancy.
The prevalence of cardiovascular disease and psychiatric disorders was roughly the same in men and women. Men had a significantly higher prevalence of diabetes, and a higher proportion of women had a malignancy.
Consistent with U.S. studies
A U.S. report in 2015 documented a higher prevalence of comorbidities and more severe illness among men undergoing bariatric surgery, compared with women, noted session chair Zhila Semnani-Azad, PhD, a researcher in the department of nutrition at Harvard School of Public Health in Boston.
“I think the [Austrian] data presented have relevance to the U.S. population,” Dr. Semnani-Azad said in an interview.
“The main limitation of these univariate analyses is they don’t account for potential confounding variables that could affect the association, such as lifestyle variables, age, and family history. There is always potential for other variables” to influence apparent sex-specific associations, she commented. Another limitation is the small total number of deaths analyzed, at 367.
“These results are a good starting point for future studies. More work is needed to better understand the impact of comorbidities and sex on postsurgical mortality,” Dr. Semnani-Azad concluded.
Dr. Beiglböck and Dr. Semnani-Azad have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EASD 2021
Hypoglycemia awareness program helps tricky-to-treat T1D
People with insulin-treated type 1 diabetes who had problems avoiding hypoglycemic episodes despite optimal care were helped significantly by a new psychoeducational program called HARPdoc, it was reported at the annual meeting of the European Association for the Study of Diabetes.
In a randomized controlled trial (RCT), both HARPdoc and the more established Blood Glucose Awareness Training (BGAT) were effective at reducing the number of severe hypoglycemia episodes seen, from five episodes at baseline to one at 1 year in both groups, and one and none at 2-years’ follow-up, respectively.
“HARPdoc is not superior to BGAT in its ability to restore hypoglycemia awareness and reduce severe hypoglycemia,” said Stephanie Amiel, MD, FRCP, the chief investigator for the trial. However, “it does reduce cognitive barriers to hypoglycemia avoidance, so it achieves what it set out to do.”
Dr. Amiel, professor of diabetes research at Kings College London, added that it was important to note that HARPdoc was better than BGAT at improving participants’ mental health, “producing a clinically important and sustainable reduction in diabetes distress, anxiety, and depression.”
What’s HARPdoc?
The Hypoglycaemia Awareness Restoration Programme for people with type 1 diabetes and problematic hypoglycaemia persisting despite optimised self-care (HARPdoc) was designed to specifically address why some people with type 1 diabetes find it difficult to avoid recurrent hypoglycemia.
“It’s a psychoeducational program with clinical knowledge about hypoglycemia and group learning, but also explicit topics on mindset and behavior change,” explained Nicole de Zoysa, DClinPsych, one of the clinical psychologists involved in the trial.
Over the course of the 6-week program, there are four group sessions (weeks 1-3, and week 6) and two individual sessions (weeks 4 and 5) that address important “cognitive barriers” or “thinking traps” to avoiding hypoglycemia that were identified during prior qualitative research.
HARPdoc is thus “an attempt to make sense of people’s reluctance or seeming reluctance to take action around hypoglycemia, Dr. de Zoysa said. The intervention draws on both cognitive behavioral theory “to work with the beliefs” and motivational interviewing “to work with the resistance.”
The HARPdoc RCT
Starting in 2017 and ending earlier this year, the HARPdoc RCT was a parallel group study conducted at three specialist diabetes centers in the United Kingdom and one in the United States.
A total of 99 adults with insulin-treated type 1 diabetes and impaired hypoglycemia awareness were enrolled – with 49 randomized to the HARPdoc arm and 50 to the BGAT arm. All had been offered technologies to help them potentially bring their hypoglycemia under better control, such as continuous glucose monitoring, insulin pumps, or closed loop systems, and received structured education on flexible insulin dosing.
The aim was to show superiority of the HARPdoc program over BGAT, in helping people avoid episodes of severe hypoglycemia, defined as episodes that needed other people’s intervention to help resolve.
BGAT is also a psychoeducation program that has been around since the 1980s but barely used in the United Kingdom, Dr. Amiel noted.
Baseline demographic characteristics were similar for the HARPdoc and BGAT arms: The mean age was 57 versus 52 years, there was a long (30+ years) duration of diabetes, over half of the participants were male, and almost all were White.
Primary endpoint not met, but still ‘impressive’
Although the primary endpoint of the trial was not met, the reductions in severe hypoglycemia seen are still “impressive,” said Ramzi Ajjan, MD, FRCP, of Leeds (England) University and Leeds Teaching Hospitals Trust.
“I was really blown away,” by the improvement in both study arms, said Dr. Ajjan, who was not involved in the trial. “These people have had proper clinical input,” he stressed, noting that both interventions worked, with no difference between them in terms of severe hypoglycemia.
Dr. Ajjan was not surprised by the better cognition scores measured using the A2A questionnaire seen with HARPdoc versus BGAT, as “this is what the intervention was designed to address.”
In terms of the mental health benefits seen, HARPdoc significantly reduced the level of diabetes distress as measured using the Problem Areas In Diabetes (PAID) questionnaire versus the BGAT intervention.
The PAID score was around 30 in both groups at baseline, this fell to about 26 at 1 year, and around 20 at 2 years in the HARPdoc group, which was significantly lower than the score seen in the BGAT group which rose slightly then fell back to baseline levels.
A similar pattern was seen in the levels of depression and anxiety, which were measured by the HADS-D and HADS-A instruments. So HARPdoc was more effective at improving psychological and mental health outcomes than BGAT, Dr. Ajjan observed.
The HARPdoc project is funded by the Juvenile Diabetes Research Foundation with additional support from the UK’s National Institute of Health Research. The HARPdoc RCT was jointly sponsored by King’s College London and King’s College Hospital NHS Foundation Trust. Dr. Amiel has served on advisory panels for Roche, Medtronic, and Novo Nordisk. Dr. de Zoysa did not state having any conflicts of interest. Dr. Ajjan disclosed that he has financial relationships with multiple pharmaceutical companies.
People with insulin-treated type 1 diabetes who had problems avoiding hypoglycemic episodes despite optimal care were helped significantly by a new psychoeducational program called HARPdoc, it was reported at the annual meeting of the European Association for the Study of Diabetes.
In a randomized controlled trial (RCT), both HARPdoc and the more established Blood Glucose Awareness Training (BGAT) were effective at reducing the number of severe hypoglycemia episodes seen, from five episodes at baseline to one at 1 year in both groups, and one and none at 2-years’ follow-up, respectively.
“HARPdoc is not superior to BGAT in its ability to restore hypoglycemia awareness and reduce severe hypoglycemia,” said Stephanie Amiel, MD, FRCP, the chief investigator for the trial. However, “it does reduce cognitive barriers to hypoglycemia avoidance, so it achieves what it set out to do.”
Dr. Amiel, professor of diabetes research at Kings College London, added that it was important to note that HARPdoc was better than BGAT at improving participants’ mental health, “producing a clinically important and sustainable reduction in diabetes distress, anxiety, and depression.”
What’s HARPdoc?
The Hypoglycaemia Awareness Restoration Programme for people with type 1 diabetes and problematic hypoglycaemia persisting despite optimised self-care (HARPdoc) was designed to specifically address why some people with type 1 diabetes find it difficult to avoid recurrent hypoglycemia.
“It’s a psychoeducational program with clinical knowledge about hypoglycemia and group learning, but also explicit topics on mindset and behavior change,” explained Nicole de Zoysa, DClinPsych, one of the clinical psychologists involved in the trial.
Over the course of the 6-week program, there are four group sessions (weeks 1-3, and week 6) and two individual sessions (weeks 4 and 5) that address important “cognitive barriers” or “thinking traps” to avoiding hypoglycemia that were identified during prior qualitative research.
HARPdoc is thus “an attempt to make sense of people’s reluctance or seeming reluctance to take action around hypoglycemia, Dr. de Zoysa said. The intervention draws on both cognitive behavioral theory “to work with the beliefs” and motivational interviewing “to work with the resistance.”
The HARPdoc RCT
Starting in 2017 and ending earlier this year, the HARPdoc RCT was a parallel group study conducted at three specialist diabetes centers in the United Kingdom and one in the United States.
A total of 99 adults with insulin-treated type 1 diabetes and impaired hypoglycemia awareness were enrolled – with 49 randomized to the HARPdoc arm and 50 to the BGAT arm. All had been offered technologies to help them potentially bring their hypoglycemia under better control, such as continuous glucose monitoring, insulin pumps, or closed loop systems, and received structured education on flexible insulin dosing.
The aim was to show superiority of the HARPdoc program over BGAT, in helping people avoid episodes of severe hypoglycemia, defined as episodes that needed other people’s intervention to help resolve.
BGAT is also a psychoeducation program that has been around since the 1980s but barely used in the United Kingdom, Dr. Amiel noted.
Baseline demographic characteristics were similar for the HARPdoc and BGAT arms: The mean age was 57 versus 52 years, there was a long (30+ years) duration of diabetes, over half of the participants were male, and almost all were White.
Primary endpoint not met, but still ‘impressive’
Although the primary endpoint of the trial was not met, the reductions in severe hypoglycemia seen are still “impressive,” said Ramzi Ajjan, MD, FRCP, of Leeds (England) University and Leeds Teaching Hospitals Trust.
“I was really blown away,” by the improvement in both study arms, said Dr. Ajjan, who was not involved in the trial. “These people have had proper clinical input,” he stressed, noting that both interventions worked, with no difference between them in terms of severe hypoglycemia.
Dr. Ajjan was not surprised by the better cognition scores measured using the A2A questionnaire seen with HARPdoc versus BGAT, as “this is what the intervention was designed to address.”
In terms of the mental health benefits seen, HARPdoc significantly reduced the level of diabetes distress as measured using the Problem Areas In Diabetes (PAID) questionnaire versus the BGAT intervention.
The PAID score was around 30 in both groups at baseline, this fell to about 26 at 1 year, and around 20 at 2 years in the HARPdoc group, which was significantly lower than the score seen in the BGAT group which rose slightly then fell back to baseline levels.
A similar pattern was seen in the levels of depression and anxiety, which were measured by the HADS-D and HADS-A instruments. So HARPdoc was more effective at improving psychological and mental health outcomes than BGAT, Dr. Ajjan observed.
The HARPdoc project is funded by the Juvenile Diabetes Research Foundation with additional support from the UK’s National Institute of Health Research. The HARPdoc RCT was jointly sponsored by King’s College London and King’s College Hospital NHS Foundation Trust. Dr. Amiel has served on advisory panels for Roche, Medtronic, and Novo Nordisk. Dr. de Zoysa did not state having any conflicts of interest. Dr. Ajjan disclosed that he has financial relationships with multiple pharmaceutical companies.
People with insulin-treated type 1 diabetes who had problems avoiding hypoglycemic episodes despite optimal care were helped significantly by a new psychoeducational program called HARPdoc, it was reported at the annual meeting of the European Association for the Study of Diabetes.
In a randomized controlled trial (RCT), both HARPdoc and the more established Blood Glucose Awareness Training (BGAT) were effective at reducing the number of severe hypoglycemia episodes seen, from five episodes at baseline to one at 1 year in both groups, and one and none at 2-years’ follow-up, respectively.
“HARPdoc is not superior to BGAT in its ability to restore hypoglycemia awareness and reduce severe hypoglycemia,” said Stephanie Amiel, MD, FRCP, the chief investigator for the trial. However, “it does reduce cognitive barriers to hypoglycemia avoidance, so it achieves what it set out to do.”
Dr. Amiel, professor of diabetes research at Kings College London, added that it was important to note that HARPdoc was better than BGAT at improving participants’ mental health, “producing a clinically important and sustainable reduction in diabetes distress, anxiety, and depression.”
What’s HARPdoc?
The Hypoglycaemia Awareness Restoration Programme for people with type 1 diabetes and problematic hypoglycaemia persisting despite optimised self-care (HARPdoc) was designed to specifically address why some people with type 1 diabetes find it difficult to avoid recurrent hypoglycemia.
“It’s a psychoeducational program with clinical knowledge about hypoglycemia and group learning, but also explicit topics on mindset and behavior change,” explained Nicole de Zoysa, DClinPsych, one of the clinical psychologists involved in the trial.
Over the course of the 6-week program, there are four group sessions (weeks 1-3, and week 6) and two individual sessions (weeks 4 and 5) that address important “cognitive barriers” or “thinking traps” to avoiding hypoglycemia that were identified during prior qualitative research.
HARPdoc is thus “an attempt to make sense of people’s reluctance or seeming reluctance to take action around hypoglycemia, Dr. de Zoysa said. The intervention draws on both cognitive behavioral theory “to work with the beliefs” and motivational interviewing “to work with the resistance.”
The HARPdoc RCT
Starting in 2017 and ending earlier this year, the HARPdoc RCT was a parallel group study conducted at three specialist diabetes centers in the United Kingdom and one in the United States.
A total of 99 adults with insulin-treated type 1 diabetes and impaired hypoglycemia awareness were enrolled – with 49 randomized to the HARPdoc arm and 50 to the BGAT arm. All had been offered technologies to help them potentially bring their hypoglycemia under better control, such as continuous glucose monitoring, insulin pumps, or closed loop systems, and received structured education on flexible insulin dosing.
The aim was to show superiority of the HARPdoc program over BGAT, in helping people avoid episodes of severe hypoglycemia, defined as episodes that needed other people’s intervention to help resolve.
BGAT is also a psychoeducation program that has been around since the 1980s but barely used in the United Kingdom, Dr. Amiel noted.
Baseline demographic characteristics were similar for the HARPdoc and BGAT arms: The mean age was 57 versus 52 years, there was a long (30+ years) duration of diabetes, over half of the participants were male, and almost all were White.
Primary endpoint not met, but still ‘impressive’
Although the primary endpoint of the trial was not met, the reductions in severe hypoglycemia seen are still “impressive,” said Ramzi Ajjan, MD, FRCP, of Leeds (England) University and Leeds Teaching Hospitals Trust.
“I was really blown away,” by the improvement in both study arms, said Dr. Ajjan, who was not involved in the trial. “These people have had proper clinical input,” he stressed, noting that both interventions worked, with no difference between them in terms of severe hypoglycemia.
Dr. Ajjan was not surprised by the better cognition scores measured using the A2A questionnaire seen with HARPdoc versus BGAT, as “this is what the intervention was designed to address.”
In terms of the mental health benefits seen, HARPdoc significantly reduced the level of diabetes distress as measured using the Problem Areas In Diabetes (PAID) questionnaire versus the BGAT intervention.
The PAID score was around 30 in both groups at baseline, this fell to about 26 at 1 year, and around 20 at 2 years in the HARPdoc group, which was significantly lower than the score seen in the BGAT group which rose slightly then fell back to baseline levels.
A similar pattern was seen in the levels of depression and anxiety, which were measured by the HADS-D and HADS-A instruments. So HARPdoc was more effective at improving psychological and mental health outcomes than BGAT, Dr. Ajjan observed.
The HARPdoc project is funded by the Juvenile Diabetes Research Foundation with additional support from the UK’s National Institute of Health Research. The HARPdoc RCT was jointly sponsored by King’s College London and King’s College Hospital NHS Foundation Trust. Dr. Amiel has served on advisory panels for Roche, Medtronic, and Novo Nordisk. Dr. de Zoysa did not state having any conflicts of interest. Dr. Ajjan disclosed that he has financial relationships with multiple pharmaceutical companies.
FROM EASD 2021
Primary goal in T2D should be weight loss, diabetologists say
Although this proposition currently has formal backing from just the four authors of the article published in the Lancet, their recommendation to elevate substantial weight loss to the front line of management for many patients with type 2 diabetes drew quick support from leaders of several diabetes organizations, albeit with some caveats.
“Our main message is that treatment of obesity should be the future of diabetes treatment,” summed up Ildiko Lingvay, MD, lead author of the new review and proposal, at the annual meeting of the European Association for the Study of Diabetes.
“Right now, a relatively small percentage of clinicians [who treat patients with type 2 diabetes] address obesity and know how to treat it. That has to change. Every clinician who treats diabetes needs to know how to treat obesity,” said Dr. Lingvay, a professor in the division of endocrinology at the University of Texas Southwestern Medical Center, Dallas.
This requires a sea change in the way clinicians approach treating patients with type 2 diabetes, which until now has generally involved “exclusive focus on glycemic control,” the authors wrote. “Practice management should refocus to effectively incorporate weight management to treat patients with type 2 diabetes.”
Successfully implementing their new, proposed change in focus “will take fundamental change,” noted Dr. Lingvay, who expressed hope that international guidelines will soon endorse this approach, an action that would be “a huge step in the right direction.”
Target weight-loss drugs to the right patients.
Initial reactions from representatives of several diabetes and obesity groups suggested that official endorsements of this management strategy for at least a subset of patients with type 2 diabetes may be forthcoming.
“The American Diabetes Association’s standards of care is aligned with this approach in focusing on obesity as a target of management in people with type 2 diabetes,” commented Nuha A. El Sayed, MD, vice president for health care improvement for the ADA. An “area of discussion” is the specific weight-loss target of at least 15%, because patients benefit from more modest weight losses of 5%-7%, and a target loss of 15% may not be achievable for some patients, she noted in a statement.
The ADA’s leadership and its professional practice committee will “carefully consider” the new, published proposal, added Dr. El Sayed, a diabetologist at the Joslin Diabetes Center in Boston.
Similar caution over generalizability of the 15% loss target came from Stefano Del Prato, MD, president of the European Society for the Study of Diabetes.
“Not everyone responds to the same extent” to the newest pharmaceuticals for facilitating weight loss, such as the glucagonlike peptide-1 receptor agonists, so the ideal would be to try to “identify patients who respond better to weight loss and can lose at least 15% of their weight. We need to improve our ability to identify patients who respond better,” said Dr. Del Prato, a professor of endocrinology and metabolism at the University of Pisa (Italy).
Despite this, he agreed in an interview that “a significant reduction in body weight should be seen as a target for treatment of type 2 diabetes,”
“Appropriate training for obesity management is essential for those working on type 2 diabetes prevention or management,” commented Jason C.G. Halford, PhD, a professor of biological psychology at the University Of Leeds (England), and president of the European Association for the Study of Obesity.
For some patients with type 2 diabetes “losing 10%-15% of body weight can mean their diabetes goes into remission,” and “losing even a small amount of weight can be life changing, it can help people better manage their blood sugars and blood pressure, and reduce their risk for developing diabetes complications like heart disease and sight loss,” commented Lucy Chambers, PhD, head of research communications for Diabetes UK.
15% loss is a ‘reachable’ goal
Dr. Lingvay and coauthors acknowledged that weight loss of less than 15% can benefit many patients with type 2 diabetes, but they felt that a loss of at least 15% gives patients a realistic and potentially potent goal to strive for.
At least 15% loss “is a goal that is beneficial and reachable for many patients. Not everyone will get there, but the closer that patients get to this, or beyond, the bigger their benefit,” she explained. “There is no magic number” for exactly how much weight a patient needs to lose to improve their health. Dr. Lingvay also highlighted that weight loss is a better target for patients than remission of their diabetes because remission may no longer be possible in patients with longstanding type 2 diabetes.
The review divides patients with type 2 diabetes into three subgroups: those with adiposity-related disease, which includes about 40%-70% of patients with type 2 diabetes; patients with cardiovascular disease as their most prominent comorbidity, a subgroup that includes about a third of patients with type 2 diabetes; and the remaining patients with primarily beta-cell dysfunction with a principle morbidity of hyperglycemia, comprising about 10%-20% of patients with type 2 diabetes. Patients in the adiposity-related diabetes subgroup form the primary target group for interventions focused on weight loss.
Incretin-based weight-loss agents propel change.
The review also links the timing of the new recommendations to recent evidence that treatment with relatively new medications from classes such as the GLP-1 receptor agonists can produce weight loss of at least 15% in most patients with type 2 diabetes, especially those with the adiposity-related form of the disease.
“The number of patients who can achieve and maintain weight loss with lifestyle alone is limited, and while bariatric surgery is very effective [for producing substantial weight loss], only a minority of patients have access to it,” and the necessary scalability of surgery is doubtful, said Priya Sumithran, MBBS, PhD, an endocrinologist and leader of the obesity research group at the University of Melbourne, and a coauthor on the new review. Compelling evidence now exists that the gap between lifestyle interventions and bariatric surgery can now be filled by a new generation of incretin-based agents that can safely produce substantial weight loss.
New agents that work as GLP-1 receptor agonists and on related incretin pathways “have changed how we think about treating type 2 diabetes,” Dr. Lingvay declared.
Dr. Lingvay and Dr. Del Prato have each been consultants to numerous drug companies. Dr. Sumithran has been an adviser to and speaker on behalf of Novo Nordisk. Dr. El Sayed, Dr. Halford, and Dr. Chambers had no relevant disclosures.
Although this proposition currently has formal backing from just the four authors of the article published in the Lancet, their recommendation to elevate substantial weight loss to the front line of management for many patients with type 2 diabetes drew quick support from leaders of several diabetes organizations, albeit with some caveats.
“Our main message is that treatment of obesity should be the future of diabetes treatment,” summed up Ildiko Lingvay, MD, lead author of the new review and proposal, at the annual meeting of the European Association for the Study of Diabetes.
“Right now, a relatively small percentage of clinicians [who treat patients with type 2 diabetes] address obesity and know how to treat it. That has to change. Every clinician who treats diabetes needs to know how to treat obesity,” said Dr. Lingvay, a professor in the division of endocrinology at the University of Texas Southwestern Medical Center, Dallas.
This requires a sea change in the way clinicians approach treating patients with type 2 diabetes, which until now has generally involved “exclusive focus on glycemic control,” the authors wrote. “Practice management should refocus to effectively incorporate weight management to treat patients with type 2 diabetes.”
Successfully implementing their new, proposed change in focus “will take fundamental change,” noted Dr. Lingvay, who expressed hope that international guidelines will soon endorse this approach, an action that would be “a huge step in the right direction.”
Target weight-loss drugs to the right patients.
Initial reactions from representatives of several diabetes and obesity groups suggested that official endorsements of this management strategy for at least a subset of patients with type 2 diabetes may be forthcoming.
“The American Diabetes Association’s standards of care is aligned with this approach in focusing on obesity as a target of management in people with type 2 diabetes,” commented Nuha A. El Sayed, MD, vice president for health care improvement for the ADA. An “area of discussion” is the specific weight-loss target of at least 15%, because patients benefit from more modest weight losses of 5%-7%, and a target loss of 15% may not be achievable for some patients, she noted in a statement.
The ADA’s leadership and its professional practice committee will “carefully consider” the new, published proposal, added Dr. El Sayed, a diabetologist at the Joslin Diabetes Center in Boston.
Similar caution over generalizability of the 15% loss target came from Stefano Del Prato, MD, president of the European Society for the Study of Diabetes.
“Not everyone responds to the same extent” to the newest pharmaceuticals for facilitating weight loss, such as the glucagonlike peptide-1 receptor agonists, so the ideal would be to try to “identify patients who respond better to weight loss and can lose at least 15% of their weight. We need to improve our ability to identify patients who respond better,” said Dr. Del Prato, a professor of endocrinology and metabolism at the University of Pisa (Italy).
Despite this, he agreed in an interview that “a significant reduction in body weight should be seen as a target for treatment of type 2 diabetes,”
“Appropriate training for obesity management is essential for those working on type 2 diabetes prevention or management,” commented Jason C.G. Halford, PhD, a professor of biological psychology at the University Of Leeds (England), and president of the European Association for the Study of Obesity.
For some patients with type 2 diabetes “losing 10%-15% of body weight can mean their diabetes goes into remission,” and “losing even a small amount of weight can be life changing, it can help people better manage their blood sugars and blood pressure, and reduce their risk for developing diabetes complications like heart disease and sight loss,” commented Lucy Chambers, PhD, head of research communications for Diabetes UK.
15% loss is a ‘reachable’ goal
Dr. Lingvay and coauthors acknowledged that weight loss of less than 15% can benefit many patients with type 2 diabetes, but they felt that a loss of at least 15% gives patients a realistic and potentially potent goal to strive for.
At least 15% loss “is a goal that is beneficial and reachable for many patients. Not everyone will get there, but the closer that patients get to this, or beyond, the bigger their benefit,” she explained. “There is no magic number” for exactly how much weight a patient needs to lose to improve their health. Dr. Lingvay also highlighted that weight loss is a better target for patients than remission of their diabetes because remission may no longer be possible in patients with longstanding type 2 diabetes.
The review divides patients with type 2 diabetes into three subgroups: those with adiposity-related disease, which includes about 40%-70% of patients with type 2 diabetes; patients with cardiovascular disease as their most prominent comorbidity, a subgroup that includes about a third of patients with type 2 diabetes; and the remaining patients with primarily beta-cell dysfunction with a principle morbidity of hyperglycemia, comprising about 10%-20% of patients with type 2 diabetes. Patients in the adiposity-related diabetes subgroup form the primary target group for interventions focused on weight loss.
Incretin-based weight-loss agents propel change.
The review also links the timing of the new recommendations to recent evidence that treatment with relatively new medications from classes such as the GLP-1 receptor agonists can produce weight loss of at least 15% in most patients with type 2 diabetes, especially those with the adiposity-related form of the disease.
“The number of patients who can achieve and maintain weight loss with lifestyle alone is limited, and while bariatric surgery is very effective [for producing substantial weight loss], only a minority of patients have access to it,” and the necessary scalability of surgery is doubtful, said Priya Sumithran, MBBS, PhD, an endocrinologist and leader of the obesity research group at the University of Melbourne, and a coauthor on the new review. Compelling evidence now exists that the gap between lifestyle interventions and bariatric surgery can now be filled by a new generation of incretin-based agents that can safely produce substantial weight loss.
New agents that work as GLP-1 receptor agonists and on related incretin pathways “have changed how we think about treating type 2 diabetes,” Dr. Lingvay declared.
Dr. Lingvay and Dr. Del Prato have each been consultants to numerous drug companies. Dr. Sumithran has been an adviser to and speaker on behalf of Novo Nordisk. Dr. El Sayed, Dr. Halford, and Dr. Chambers had no relevant disclosures.
Although this proposition currently has formal backing from just the four authors of the article published in the Lancet, their recommendation to elevate substantial weight loss to the front line of management for many patients with type 2 diabetes drew quick support from leaders of several diabetes organizations, albeit with some caveats.
“Our main message is that treatment of obesity should be the future of diabetes treatment,” summed up Ildiko Lingvay, MD, lead author of the new review and proposal, at the annual meeting of the European Association for the Study of Diabetes.
“Right now, a relatively small percentage of clinicians [who treat patients with type 2 diabetes] address obesity and know how to treat it. That has to change. Every clinician who treats diabetes needs to know how to treat obesity,” said Dr. Lingvay, a professor in the division of endocrinology at the University of Texas Southwestern Medical Center, Dallas.
This requires a sea change in the way clinicians approach treating patients with type 2 diabetes, which until now has generally involved “exclusive focus on glycemic control,” the authors wrote. “Practice management should refocus to effectively incorporate weight management to treat patients with type 2 diabetes.”
Successfully implementing their new, proposed change in focus “will take fundamental change,” noted Dr. Lingvay, who expressed hope that international guidelines will soon endorse this approach, an action that would be “a huge step in the right direction.”
Target weight-loss drugs to the right patients.
Initial reactions from representatives of several diabetes and obesity groups suggested that official endorsements of this management strategy for at least a subset of patients with type 2 diabetes may be forthcoming.
“The American Diabetes Association’s standards of care is aligned with this approach in focusing on obesity as a target of management in people with type 2 diabetes,” commented Nuha A. El Sayed, MD, vice president for health care improvement for the ADA. An “area of discussion” is the specific weight-loss target of at least 15%, because patients benefit from more modest weight losses of 5%-7%, and a target loss of 15% may not be achievable for some patients, she noted in a statement.
The ADA’s leadership and its professional practice committee will “carefully consider” the new, published proposal, added Dr. El Sayed, a diabetologist at the Joslin Diabetes Center in Boston.
Similar caution over generalizability of the 15% loss target came from Stefano Del Prato, MD, president of the European Society for the Study of Diabetes.
“Not everyone responds to the same extent” to the newest pharmaceuticals for facilitating weight loss, such as the glucagonlike peptide-1 receptor agonists, so the ideal would be to try to “identify patients who respond better to weight loss and can lose at least 15% of their weight. We need to improve our ability to identify patients who respond better,” said Dr. Del Prato, a professor of endocrinology and metabolism at the University of Pisa (Italy).
Despite this, he agreed in an interview that “a significant reduction in body weight should be seen as a target for treatment of type 2 diabetes,”
“Appropriate training for obesity management is essential for those working on type 2 diabetes prevention or management,” commented Jason C.G. Halford, PhD, a professor of biological psychology at the University Of Leeds (England), and president of the European Association for the Study of Obesity.
For some patients with type 2 diabetes “losing 10%-15% of body weight can mean their diabetes goes into remission,” and “losing even a small amount of weight can be life changing, it can help people better manage their blood sugars and blood pressure, and reduce their risk for developing diabetes complications like heart disease and sight loss,” commented Lucy Chambers, PhD, head of research communications for Diabetes UK.
15% loss is a ‘reachable’ goal
Dr. Lingvay and coauthors acknowledged that weight loss of less than 15% can benefit many patients with type 2 diabetes, but they felt that a loss of at least 15% gives patients a realistic and potentially potent goal to strive for.
At least 15% loss “is a goal that is beneficial and reachable for many patients. Not everyone will get there, but the closer that patients get to this, or beyond, the bigger their benefit,” she explained. “There is no magic number” for exactly how much weight a patient needs to lose to improve their health. Dr. Lingvay also highlighted that weight loss is a better target for patients than remission of their diabetes because remission may no longer be possible in patients with longstanding type 2 diabetes.
The review divides patients with type 2 diabetes into three subgroups: those with adiposity-related disease, which includes about 40%-70% of patients with type 2 diabetes; patients with cardiovascular disease as their most prominent comorbidity, a subgroup that includes about a third of patients with type 2 diabetes; and the remaining patients with primarily beta-cell dysfunction with a principle morbidity of hyperglycemia, comprising about 10%-20% of patients with type 2 diabetes. Patients in the adiposity-related diabetes subgroup form the primary target group for interventions focused on weight loss.
Incretin-based weight-loss agents propel change.
The review also links the timing of the new recommendations to recent evidence that treatment with relatively new medications from classes such as the GLP-1 receptor agonists can produce weight loss of at least 15% in most patients with type 2 diabetes, especially those with the adiposity-related form of the disease.
“The number of patients who can achieve and maintain weight loss with lifestyle alone is limited, and while bariatric surgery is very effective [for producing substantial weight loss], only a minority of patients have access to it,” and the necessary scalability of surgery is doubtful, said Priya Sumithran, MBBS, PhD, an endocrinologist and leader of the obesity research group at the University of Melbourne, and a coauthor on the new review. Compelling evidence now exists that the gap between lifestyle interventions and bariatric surgery can now be filled by a new generation of incretin-based agents that can safely produce substantial weight loss.
New agents that work as GLP-1 receptor agonists and on related incretin pathways “have changed how we think about treating type 2 diabetes,” Dr. Lingvay declared.
Dr. Lingvay and Dr. Del Prato have each been consultants to numerous drug companies. Dr. Sumithran has been an adviser to and speaker on behalf of Novo Nordisk. Dr. El Sayed, Dr. Halford, and Dr. Chambers had no relevant disclosures.
FROM EASD 2021
TriMaster study shows precision medicine in diabetes is possible
A uniquely-designed three-drug study has demonstrated that individual clinical characteristics, including patient preference, can be used to guide medication choice in type 2 diabetes.
Results from the TriMaster trial using sitagliptin, pioglitazone, and canagliflozin as second- or third-line therapy in a total of 525 patients with type 2 diabetes were presented September 29 at the virtual European Association for the Study of Diabetes (EASD) 2021 Annual Meeting.
TriMaster is a phase 4, multicenter, randomized, double-blind, 12-month crossover trial examining the effects of all three drugs in subgroups of patients with type 2 diabetes who hadn’t achieved target glucose levels with metformin alone or combined with a sulfonylurea.
While all three drugs lowered glucose similarly overall, pioglitazone did so more effectively among patients with a body mass index (BMI) above 30 kg/m2, while sitagliptin worked better in those with a BMI less than 30 kg/m2. However, pioglitazone resulted in more weight gain.
In a second comparison, canagliflozin (a sodium-glucose cotransporter 2 [SGLT2] inhibitor) was more effective than sitagliptin (a dipeptidyl peptidase-4 [DPP-4] inhibitor) in lowering glucose among patients with an estimated glomerular filtration rate (eGFR) above 90 mL/min/1.73m2, while sitagliptin actually lowered glucose better among individuals with an eGFR 60-90 mL/min/1.73m2 than canagliflozin.
And when participants were asked which drug they preferred, the results were split nearly evenly among the three, correlating with how well the drug worked and the side effect profile for each individual.
“We proved a precision approach worked using predefined clinical criteria to define groups of patients where one drug is better than another. This is the first-ever proof of a precision medicine approach in type 2 diabetes,” chief investigator Andrew Hattersley, DM, professor of molecular medicine at the University of Exeter, U.K., told this news organization.
But, he stressed, “These results do not mean all patients with BMI above 30 should have pioglitazone or that all patients with an eGFR 60-90 should have a DPP-4 inhibitor.”
“Drug choice will need to consider other priorities than glycemia ... Patients with heart failure, cardiovascular disease, and chronic kidney disease should be prescribed SGLT2 inhibitors,” he noted. And “some patients will need to avoid specific drugs due to likely side effects.”
‘Modern era’ study used older drugs
Independent commentator Caroline M. Kistorp, MD, PhD, professor of endocrinology at University Hospital Copenhagen, congratulated the investigators for “moving precision medicine from the retrospective analysis of existing data into the modern era of evidence-based medicine with this randomized clinical trial in patients with type 2 diabetes ... Starting this trial back in 2015 was really ahead of their time.”
However, she questioned the use of a thiazolidinedione (TZD), pioglitazone, in the trial, as they are no longer used in many parts of the world in favor of more “modern” glucose-lowering drugs.
“I’m thinking of GLP-1 receptor agonists, especially if you want to treat type 2 diabetes patients who are obese with a BMI over 30 ... I acknowledge that there is a cost issue, but I still think we should try to give our patients the best treatments, so that’s why I’m not sure how much the [TZDs] will be used in the future, even with this trial,” she said.
Dr. Kistorp also noted the trial didn’t include cardiovascular disease outcomes, for which most SGLT2 inhibitors have shown benefit.
“We have to discuss and consider whether A1c is the most important parameter for these patients ... especially looking at their cardiovascular outcomes.”
Mr. Hattersley responded that the study was designed in 2015, prior to the landmark EMPA-REG OUTCOME trial that began the shift toward use of SGLT2 inhibitors for cardiovascular and kidney disease reduction in addition to glycemic control in the clinical management of type 2 diabetes.
“We will report the cardiovascular profiles, but it wasn’t a specific thing because at that time the evidence didn’t exist, so it wasn’t in our protocol,” he explained.
Regarding pioglitazone, he acknowledged that although it may be an alternative to insulin for some patients, “I think for most people you won’t be considering it in clinical practice,” but because it has a very different mechanism from the other two study drugs, “it did give the greater chance of differential effects ... Partly, what we’re really trying to do is test the question of whether precision medicine exists and can we do it.”
Unique study design had each patient act as their own control
Trial statistician Beverley Shields, PhD, of the University of Exeter, U.K., reported the results. The 525 participants with type 2 diabetes were aged 30-79 years and had A1c levels above 58 mmol/mol (7.5%) but not greater than 110 mmol/mol (12.2%) with metformin alone or combined with a sulfonylurea. Just over half (58%) had a BMI above 30 kg/m2 and 52% had an eGFR greater than 90 mL/min/1.73m2.
Each participant received each of the three medications as second- or third-line oral therapy in random order – in one of six possible sequences – for 16 weeks each, with no washout period in between (to prevent dropouts due to hyperglycemia). Thus, each participant acted as their own control.
A total of 458 participants completed all three study periods.
The drugs work differently in different patient groups
Without stratification by patient type, there was no overall difference in A1c reduction between the three therapies, with all achieving about 59-60 mmol/mol (7.5-7.6%) from a baseline average of 69 mmol/mol (8.9%).
But when stratified by BMI, A1c was 1.48 mmol/mol higher with pioglitazone versus sitagliptin in the group with BMI less than 30 kg/m2 and 1.44 mmol/mol lower with pioglitazone versus sitagliptin in the group with BMI greater than 30 kg/m2, giving a significant overall difference of 2.92 mmol/mol (P = .003).
By eGFR stratification, A1c was 1.74 mmol/mol lower with sitagliptin than canagliflozin in the 60-90 mL/min/1.73m2 group and 1.08 mmol/mol higher in the greater than 90 mL/min/1.73m2 group, giving a significant difference of 2.83 mmol/mol (P = .002).
“So, if we were to treat the patients with the drug that is optimal for their strata ... this would lead to a benefit of about 3 mmol/mol compared to if those patients were treated with the other drug,” Dr. Shields said.
By BMI, there were no significant differences by drug or strata for tolerability, defined as staying on drug for at least 12 weeks (P = .2), nor in the percentage of patients reporting at least one hypoglycemic episode (P = .6).
However, pioglitazone was associated with higher weight gain in both BMI groups, resulting in a 0.93 kg difference overall (P < .001), although it was higher in the higher BMI group (1.9 vs. 0.97 kg).
Similarly, by eGFR there were no differences in tolerability or hypoglycemic episodes between sitagliptin and canagliflozin (P = .09 and P = .6, respectively). And here, there were no differences in weight (P = .6).
Patients compared their own experiences with each drug
Patients were asked about their drug preferences after being reminded about their own changes in A1c and weight with each one. The result was a split: 25.8% picked pioglitazone, 34.8% sitagliptin, and 38.7% canagliflozin.
Looking at study outcomes by therapy, pioglitazone had the lowest rate of nontolerability but the highest weight gain, sitagliptin had the highest nontolerability but the lowest number of side effects, while canagliflozin had the highest number of reported side effects but the lowest weight gain.
Patients’ preferred drugs were associated with the lowest A1c and the fewest side effects for each group. Interestingly, pioglitazone was associated with the highest weight on therapy regardless of preference, so that even those who preferred pioglitazone had a higher weight than they did with the other two drugs.
In response to an audience question about durability of the results given the relatively short trial periods, Mr. Hattersley said: “We’re following up these patients who have chosen their drug, and on the whole, their primary care doctor agreed with them. So we’re following that up as a prospective cohort. We’re looking at tolerance and response and also to see if they’re still happy with that drug. That will be a future analysis.”
The TriMASTER data will be submitted for publication soon.
TriMASTER was funded by the UK Medical Research Council. Mr. Hattersley and Dr. Shields have reported no relevant financial relationships. Dr. Kistorp has reported receiving honoraria from and/or is on advisory boards for AstraZeneca, Novo Nordisk, Boehringer Ingelheim, MSD, Otsuka Pharma, and Chiesi.
A version of this article first appeared on Medscape.com.
A uniquely-designed three-drug study has demonstrated that individual clinical characteristics, including patient preference, can be used to guide medication choice in type 2 diabetes.
Results from the TriMaster trial using sitagliptin, pioglitazone, and canagliflozin as second- or third-line therapy in a total of 525 patients with type 2 diabetes were presented September 29 at the virtual European Association for the Study of Diabetes (EASD) 2021 Annual Meeting.
TriMaster is a phase 4, multicenter, randomized, double-blind, 12-month crossover trial examining the effects of all three drugs in subgroups of patients with type 2 diabetes who hadn’t achieved target glucose levels with metformin alone or combined with a sulfonylurea.
While all three drugs lowered glucose similarly overall, pioglitazone did so more effectively among patients with a body mass index (BMI) above 30 kg/m2, while sitagliptin worked better in those with a BMI less than 30 kg/m2. However, pioglitazone resulted in more weight gain.
In a second comparison, canagliflozin (a sodium-glucose cotransporter 2 [SGLT2] inhibitor) was more effective than sitagliptin (a dipeptidyl peptidase-4 [DPP-4] inhibitor) in lowering glucose among patients with an estimated glomerular filtration rate (eGFR) above 90 mL/min/1.73m2, while sitagliptin actually lowered glucose better among individuals with an eGFR 60-90 mL/min/1.73m2 than canagliflozin.
And when participants were asked which drug they preferred, the results were split nearly evenly among the three, correlating with how well the drug worked and the side effect profile for each individual.
“We proved a precision approach worked using predefined clinical criteria to define groups of patients where one drug is better than another. This is the first-ever proof of a precision medicine approach in type 2 diabetes,” chief investigator Andrew Hattersley, DM, professor of molecular medicine at the University of Exeter, U.K., told this news organization.
But, he stressed, “These results do not mean all patients with BMI above 30 should have pioglitazone or that all patients with an eGFR 60-90 should have a DPP-4 inhibitor.”
“Drug choice will need to consider other priorities than glycemia ... Patients with heart failure, cardiovascular disease, and chronic kidney disease should be prescribed SGLT2 inhibitors,” he noted. And “some patients will need to avoid specific drugs due to likely side effects.”
‘Modern era’ study used older drugs
Independent commentator Caroline M. Kistorp, MD, PhD, professor of endocrinology at University Hospital Copenhagen, congratulated the investigators for “moving precision medicine from the retrospective analysis of existing data into the modern era of evidence-based medicine with this randomized clinical trial in patients with type 2 diabetes ... Starting this trial back in 2015 was really ahead of their time.”
However, she questioned the use of a thiazolidinedione (TZD), pioglitazone, in the trial, as they are no longer used in many parts of the world in favor of more “modern” glucose-lowering drugs.
“I’m thinking of GLP-1 receptor agonists, especially if you want to treat type 2 diabetes patients who are obese with a BMI over 30 ... I acknowledge that there is a cost issue, but I still think we should try to give our patients the best treatments, so that’s why I’m not sure how much the [TZDs] will be used in the future, even with this trial,” she said.
Dr. Kistorp also noted the trial didn’t include cardiovascular disease outcomes, for which most SGLT2 inhibitors have shown benefit.
“We have to discuss and consider whether A1c is the most important parameter for these patients ... especially looking at their cardiovascular outcomes.”
Mr. Hattersley responded that the study was designed in 2015, prior to the landmark EMPA-REG OUTCOME trial that began the shift toward use of SGLT2 inhibitors for cardiovascular and kidney disease reduction in addition to glycemic control in the clinical management of type 2 diabetes.
“We will report the cardiovascular profiles, but it wasn’t a specific thing because at that time the evidence didn’t exist, so it wasn’t in our protocol,” he explained.
Regarding pioglitazone, he acknowledged that although it may be an alternative to insulin for some patients, “I think for most people you won’t be considering it in clinical practice,” but because it has a very different mechanism from the other two study drugs, “it did give the greater chance of differential effects ... Partly, what we’re really trying to do is test the question of whether precision medicine exists and can we do it.”
Unique study design had each patient act as their own control
Trial statistician Beverley Shields, PhD, of the University of Exeter, U.K., reported the results. The 525 participants with type 2 diabetes were aged 30-79 years and had A1c levels above 58 mmol/mol (7.5%) but not greater than 110 mmol/mol (12.2%) with metformin alone or combined with a sulfonylurea. Just over half (58%) had a BMI above 30 kg/m2 and 52% had an eGFR greater than 90 mL/min/1.73m2.
Each participant received each of the three medications as second- or third-line oral therapy in random order – in one of six possible sequences – for 16 weeks each, with no washout period in between (to prevent dropouts due to hyperglycemia). Thus, each participant acted as their own control.
A total of 458 participants completed all three study periods.
The drugs work differently in different patient groups
Without stratification by patient type, there was no overall difference in A1c reduction between the three therapies, with all achieving about 59-60 mmol/mol (7.5-7.6%) from a baseline average of 69 mmol/mol (8.9%).
But when stratified by BMI, A1c was 1.48 mmol/mol higher with pioglitazone versus sitagliptin in the group with BMI less than 30 kg/m2 and 1.44 mmol/mol lower with pioglitazone versus sitagliptin in the group with BMI greater than 30 kg/m2, giving a significant overall difference of 2.92 mmol/mol (P = .003).
By eGFR stratification, A1c was 1.74 mmol/mol lower with sitagliptin than canagliflozin in the 60-90 mL/min/1.73m2 group and 1.08 mmol/mol higher in the greater than 90 mL/min/1.73m2 group, giving a significant difference of 2.83 mmol/mol (P = .002).
“So, if we were to treat the patients with the drug that is optimal for their strata ... this would lead to a benefit of about 3 mmol/mol compared to if those patients were treated with the other drug,” Dr. Shields said.
By BMI, there were no significant differences by drug or strata for tolerability, defined as staying on drug for at least 12 weeks (P = .2), nor in the percentage of patients reporting at least one hypoglycemic episode (P = .6).
However, pioglitazone was associated with higher weight gain in both BMI groups, resulting in a 0.93 kg difference overall (P < .001), although it was higher in the higher BMI group (1.9 vs. 0.97 kg).
Similarly, by eGFR there were no differences in tolerability or hypoglycemic episodes between sitagliptin and canagliflozin (P = .09 and P = .6, respectively). And here, there were no differences in weight (P = .6).
Patients compared their own experiences with each drug
Patients were asked about their drug preferences after being reminded about their own changes in A1c and weight with each one. The result was a split: 25.8% picked pioglitazone, 34.8% sitagliptin, and 38.7% canagliflozin.
Looking at study outcomes by therapy, pioglitazone had the lowest rate of nontolerability but the highest weight gain, sitagliptin had the highest nontolerability but the lowest number of side effects, while canagliflozin had the highest number of reported side effects but the lowest weight gain.
Patients’ preferred drugs were associated with the lowest A1c and the fewest side effects for each group. Interestingly, pioglitazone was associated with the highest weight on therapy regardless of preference, so that even those who preferred pioglitazone had a higher weight than they did with the other two drugs.
In response to an audience question about durability of the results given the relatively short trial periods, Mr. Hattersley said: “We’re following up these patients who have chosen their drug, and on the whole, their primary care doctor agreed with them. So we’re following that up as a prospective cohort. We’re looking at tolerance and response and also to see if they’re still happy with that drug. That will be a future analysis.”
The TriMASTER data will be submitted for publication soon.
TriMASTER was funded by the UK Medical Research Council. Mr. Hattersley and Dr. Shields have reported no relevant financial relationships. Dr. Kistorp has reported receiving honoraria from and/or is on advisory boards for AstraZeneca, Novo Nordisk, Boehringer Ingelheim, MSD, Otsuka Pharma, and Chiesi.
A version of this article first appeared on Medscape.com.
A uniquely-designed three-drug study has demonstrated that individual clinical characteristics, including patient preference, can be used to guide medication choice in type 2 diabetes.
Results from the TriMaster trial using sitagliptin, pioglitazone, and canagliflozin as second- or third-line therapy in a total of 525 patients with type 2 diabetes were presented September 29 at the virtual European Association for the Study of Diabetes (EASD) 2021 Annual Meeting.
TriMaster is a phase 4, multicenter, randomized, double-blind, 12-month crossover trial examining the effects of all three drugs in subgroups of patients with type 2 diabetes who hadn’t achieved target glucose levels with metformin alone or combined with a sulfonylurea.
While all three drugs lowered glucose similarly overall, pioglitazone did so more effectively among patients with a body mass index (BMI) above 30 kg/m2, while sitagliptin worked better in those with a BMI less than 30 kg/m2. However, pioglitazone resulted in more weight gain.
In a second comparison, canagliflozin (a sodium-glucose cotransporter 2 [SGLT2] inhibitor) was more effective than sitagliptin (a dipeptidyl peptidase-4 [DPP-4] inhibitor) in lowering glucose among patients with an estimated glomerular filtration rate (eGFR) above 90 mL/min/1.73m2, while sitagliptin actually lowered glucose better among individuals with an eGFR 60-90 mL/min/1.73m2 than canagliflozin.
And when participants were asked which drug they preferred, the results were split nearly evenly among the three, correlating with how well the drug worked and the side effect profile for each individual.
“We proved a precision approach worked using predefined clinical criteria to define groups of patients where one drug is better than another. This is the first-ever proof of a precision medicine approach in type 2 diabetes,” chief investigator Andrew Hattersley, DM, professor of molecular medicine at the University of Exeter, U.K., told this news organization.
But, he stressed, “These results do not mean all patients with BMI above 30 should have pioglitazone or that all patients with an eGFR 60-90 should have a DPP-4 inhibitor.”
“Drug choice will need to consider other priorities than glycemia ... Patients with heart failure, cardiovascular disease, and chronic kidney disease should be prescribed SGLT2 inhibitors,” he noted. And “some patients will need to avoid specific drugs due to likely side effects.”
‘Modern era’ study used older drugs
Independent commentator Caroline M. Kistorp, MD, PhD, professor of endocrinology at University Hospital Copenhagen, congratulated the investigators for “moving precision medicine from the retrospective analysis of existing data into the modern era of evidence-based medicine with this randomized clinical trial in patients with type 2 diabetes ... Starting this trial back in 2015 was really ahead of their time.”
However, she questioned the use of a thiazolidinedione (TZD), pioglitazone, in the trial, as they are no longer used in many parts of the world in favor of more “modern” glucose-lowering drugs.
“I’m thinking of GLP-1 receptor agonists, especially if you want to treat type 2 diabetes patients who are obese with a BMI over 30 ... I acknowledge that there is a cost issue, but I still think we should try to give our patients the best treatments, so that’s why I’m not sure how much the [TZDs] will be used in the future, even with this trial,” she said.
Dr. Kistorp also noted the trial didn’t include cardiovascular disease outcomes, for which most SGLT2 inhibitors have shown benefit.
“We have to discuss and consider whether A1c is the most important parameter for these patients ... especially looking at their cardiovascular outcomes.”
Mr. Hattersley responded that the study was designed in 2015, prior to the landmark EMPA-REG OUTCOME trial that began the shift toward use of SGLT2 inhibitors for cardiovascular and kidney disease reduction in addition to glycemic control in the clinical management of type 2 diabetes.
“We will report the cardiovascular profiles, but it wasn’t a specific thing because at that time the evidence didn’t exist, so it wasn’t in our protocol,” he explained.
Regarding pioglitazone, he acknowledged that although it may be an alternative to insulin for some patients, “I think for most people you won’t be considering it in clinical practice,” but because it has a very different mechanism from the other two study drugs, “it did give the greater chance of differential effects ... Partly, what we’re really trying to do is test the question of whether precision medicine exists and can we do it.”
Unique study design had each patient act as their own control
Trial statistician Beverley Shields, PhD, of the University of Exeter, U.K., reported the results. The 525 participants with type 2 diabetes were aged 30-79 years and had A1c levels above 58 mmol/mol (7.5%) but not greater than 110 mmol/mol (12.2%) with metformin alone or combined with a sulfonylurea. Just over half (58%) had a BMI above 30 kg/m2 and 52% had an eGFR greater than 90 mL/min/1.73m2.
Each participant received each of the three medications as second- or third-line oral therapy in random order – in one of six possible sequences – for 16 weeks each, with no washout period in between (to prevent dropouts due to hyperglycemia). Thus, each participant acted as their own control.
A total of 458 participants completed all three study periods.
The drugs work differently in different patient groups
Without stratification by patient type, there was no overall difference in A1c reduction between the three therapies, with all achieving about 59-60 mmol/mol (7.5-7.6%) from a baseline average of 69 mmol/mol (8.9%).
But when stratified by BMI, A1c was 1.48 mmol/mol higher with pioglitazone versus sitagliptin in the group with BMI less than 30 kg/m2 and 1.44 mmol/mol lower with pioglitazone versus sitagliptin in the group with BMI greater than 30 kg/m2, giving a significant overall difference of 2.92 mmol/mol (P = .003).
By eGFR stratification, A1c was 1.74 mmol/mol lower with sitagliptin than canagliflozin in the 60-90 mL/min/1.73m2 group and 1.08 mmol/mol higher in the greater than 90 mL/min/1.73m2 group, giving a significant difference of 2.83 mmol/mol (P = .002).
“So, if we were to treat the patients with the drug that is optimal for their strata ... this would lead to a benefit of about 3 mmol/mol compared to if those patients were treated with the other drug,” Dr. Shields said.
By BMI, there were no significant differences by drug or strata for tolerability, defined as staying on drug for at least 12 weeks (P = .2), nor in the percentage of patients reporting at least one hypoglycemic episode (P = .6).
However, pioglitazone was associated with higher weight gain in both BMI groups, resulting in a 0.93 kg difference overall (P < .001), although it was higher in the higher BMI group (1.9 vs. 0.97 kg).
Similarly, by eGFR there were no differences in tolerability or hypoglycemic episodes between sitagliptin and canagliflozin (P = .09 and P = .6, respectively). And here, there were no differences in weight (P = .6).
Patients compared their own experiences with each drug
Patients were asked about their drug preferences after being reminded about their own changes in A1c and weight with each one. The result was a split: 25.8% picked pioglitazone, 34.8% sitagliptin, and 38.7% canagliflozin.
Looking at study outcomes by therapy, pioglitazone had the lowest rate of nontolerability but the highest weight gain, sitagliptin had the highest nontolerability but the lowest number of side effects, while canagliflozin had the highest number of reported side effects but the lowest weight gain.
Patients’ preferred drugs were associated with the lowest A1c and the fewest side effects for each group. Interestingly, pioglitazone was associated with the highest weight on therapy regardless of preference, so that even those who preferred pioglitazone had a higher weight than they did with the other two drugs.
In response to an audience question about durability of the results given the relatively short trial periods, Mr. Hattersley said: “We’re following up these patients who have chosen their drug, and on the whole, their primary care doctor agreed with them. So we’re following that up as a prospective cohort. We’re looking at tolerance and response and also to see if they’re still happy with that drug. That will be a future analysis.”
The TriMASTER data will be submitted for publication soon.
TriMASTER was funded by the UK Medical Research Council. Mr. Hattersley and Dr. Shields have reported no relevant financial relationships. Dr. Kistorp has reported receiving honoraria from and/or is on advisory boards for AstraZeneca, Novo Nordisk, Boehringer Ingelheim, MSD, Otsuka Pharma, and Chiesi.
A version of this article first appeared on Medscape.com.
Cell therapy promising as long-term limb-saving treatment in diabetes
Bone marrow derived autologous cell therapy (ACT) has been shown to significantly reduce the rate of major amputation at 5 years in people with diabetes who developed critical limb-threatening ischemia (CLTI).
In a study of 130 patients, 64% of 42 patients who were treated conservatively needed a major amputation at 5 years versus just 30% of 45 patients who had been treated with ACT (P = .011).
This compared favorably to the results seen with repeated percutaneous angioplasty (re-PTA), where just 20.9% of 43 patients underwent limb salvage (P = .002 vs. conservative therapy).
Furthermore, amputation-free survival was significantly longer in both active groups, Michal Dubský, MD, PhD, FRSPH, reported at the annual meeting of the European Association for the Study of Diabetes.
Dr. Dubský, of the Institute for Clinical and Experimental Medicine and Charles University in Prague, also reported that fewer patients who had undergone re-PTA or ACT than conservative treatment had died by 5 years (25.8% and 35.6%, respectively, vs. 61.9%), but that the difference was significant only for the revascularization procedure (P = .012).
Based on these findings, “we believe that autologous cell therapy seems to be an appropriate alternative to repeated PTA even for patients with no-option chronic limb-threatening ischemia,” he said.
“This is a very important area,” said Andrew J.M. Boulton, MBBS, MD, FRCP, who chaired the oral abstract presentation session during which the findings were presented.
“It is very difficult to get an evidence base from randomized studies in this area, because of the nature of the patients: They’re very sick and we all deal with them in our clinics very regularly,” added Dr. Boulton, professor of medicine within the division of diabetes, endocrinology and gastroenterology at the University of Manchester (England).
Dr. Boulton called the findings a “very important addition to what we know.”
New option for no-option CLTI
CLTI is associated with persistent pain at rest, ulcers, and gangrene, and can be the end result of longstanding peripheral arterial disease. Within the first year of presentation, there’s a 30% chance of having a major amputation and a 25% chance of dying.
Importantly, said Dr. Dubský, “there is a big difference in this diagnosis” between patients with diabetes and those without. For instance, CLTI is more diffuse in patients with diabetes than in those without, different arteries are affected and the sclerosis seen can be more rigid and “full of calcium.”
While surgery to improve blood flow is the standard of care, not everyone is suitable. Bypass surgery or endovascular procedures can be performed in only 40%-50% of patients, and even then a therapeutic effect may be seen in only a quarter of patients.
“We need some new therapeutic modalities for this diagnosis, and one of them could be autologous cell therapy,” said Dr. Dubský.
Study details
Dr. Dubský and coinvestigators consecutively recruited 130 patients with diabetic foot and CLTI who had been seen at their clinic over a 5-year period. Of these, 87 had not been eligible for standard revascularization and underwent ACT or were treated conservatively.
Of the patients who were not eligible for standard revascularization (‘no-option CLTI), 45 had undergone ACT and 42 had been treated conservatively. Dr. Dubský acknowledged that “his study was not prospective and randomized.”
All patients in the study had at least one unsuccessful revascularization procedure and diabetic foot ulcers, and low tissue oxygenation. The latter was defined as transcutaneous oxygen pressure (TcPO2) of below 30 mm Hg.
There were little differences in demographic characteristics between the treatment groups, the average age ranged from 62 to 67 years, there were more men (70%-80%) than women; most patients (90%) had type 2 diabetes for at least 20 years. There were similar rates of ischemic heart disease, hypertension, dialysis, and immunosuppressive therapy.
There were no differences in baseline values of TcPO2 between the groups, and similar improvements were seen in both the ACT and re-PTA groups versus conservative group.
ACT in practice
With such promising results, what about the practicalities of harvesting a patient’s bone marrow to make the ACT?
“Bone marrow harvesting usually takes about 20 minutes,” Dr. Dubský said. It then takes another 45 minutes to separate the cells and make the cell suspension, and then maybe another 10 minutes or so to administer this to the patient, which is done by injecting into the calf muscles and small muscles of the foot, aided by computed tomography. The whole process may take up to 2 hours, he said.
“Patients are under local or general anesthesia, so there is no pain during the procedure,” Dr. Dubský reassured. “Afterwards we sometimes see small hematoma[s], with low-intensity pain that responds well to usual analgesic therapy.”
Computed tomography was used to help guide the injections, which was advantageous, Dr. Boulton pointed out, because it was “less invasive than angioplasty in these very sick people with very distal lesions, many of whom already have renal problems.”
“It is surprising though, that everybody had re-PTA and not one had vascular surgery,” he suggested. Dr. Boulton added, however: “These are very important observations; they help us a lot in an area where there’s unlikely to be a full RCT.”
The next step in this research is to see if combining ACT and re-PTA could lead to even better results.
The study was funded by the Czech Republic Ministry of Health. Dr. Dubský had nothing to disclose. Dr. Boulton made no statement about his conflicts of interest.
Bone marrow derived autologous cell therapy (ACT) has been shown to significantly reduce the rate of major amputation at 5 years in people with diabetes who developed critical limb-threatening ischemia (CLTI).
In a study of 130 patients, 64% of 42 patients who were treated conservatively needed a major amputation at 5 years versus just 30% of 45 patients who had been treated with ACT (P = .011).
This compared favorably to the results seen with repeated percutaneous angioplasty (re-PTA), where just 20.9% of 43 patients underwent limb salvage (P = .002 vs. conservative therapy).
Furthermore, amputation-free survival was significantly longer in both active groups, Michal Dubský, MD, PhD, FRSPH, reported at the annual meeting of the European Association for the Study of Diabetes.
Dr. Dubský, of the Institute for Clinical and Experimental Medicine and Charles University in Prague, also reported that fewer patients who had undergone re-PTA or ACT than conservative treatment had died by 5 years (25.8% and 35.6%, respectively, vs. 61.9%), but that the difference was significant only for the revascularization procedure (P = .012).
Based on these findings, “we believe that autologous cell therapy seems to be an appropriate alternative to repeated PTA even for patients with no-option chronic limb-threatening ischemia,” he said.
“This is a very important area,” said Andrew J.M. Boulton, MBBS, MD, FRCP, who chaired the oral abstract presentation session during which the findings were presented.
“It is very difficult to get an evidence base from randomized studies in this area, because of the nature of the patients: They’re very sick and we all deal with them in our clinics very regularly,” added Dr. Boulton, professor of medicine within the division of diabetes, endocrinology and gastroenterology at the University of Manchester (England).
Dr. Boulton called the findings a “very important addition to what we know.”
New option for no-option CLTI
CLTI is associated with persistent pain at rest, ulcers, and gangrene, and can be the end result of longstanding peripheral arterial disease. Within the first year of presentation, there’s a 30% chance of having a major amputation and a 25% chance of dying.
Importantly, said Dr. Dubský, “there is a big difference in this diagnosis” between patients with diabetes and those without. For instance, CLTI is more diffuse in patients with diabetes than in those without, different arteries are affected and the sclerosis seen can be more rigid and “full of calcium.”
While surgery to improve blood flow is the standard of care, not everyone is suitable. Bypass surgery or endovascular procedures can be performed in only 40%-50% of patients, and even then a therapeutic effect may be seen in only a quarter of patients.
“We need some new therapeutic modalities for this diagnosis, and one of them could be autologous cell therapy,” said Dr. Dubský.
Study details
Dr. Dubský and coinvestigators consecutively recruited 130 patients with diabetic foot and CLTI who had been seen at their clinic over a 5-year period. Of these, 87 had not been eligible for standard revascularization and underwent ACT or were treated conservatively.
Of the patients who were not eligible for standard revascularization (‘no-option CLTI), 45 had undergone ACT and 42 had been treated conservatively. Dr. Dubský acknowledged that “his study was not prospective and randomized.”
All patients in the study had at least one unsuccessful revascularization procedure and diabetic foot ulcers, and low tissue oxygenation. The latter was defined as transcutaneous oxygen pressure (TcPO2) of below 30 mm Hg.
There were little differences in demographic characteristics between the treatment groups, the average age ranged from 62 to 67 years, there were more men (70%-80%) than women; most patients (90%) had type 2 diabetes for at least 20 years. There were similar rates of ischemic heart disease, hypertension, dialysis, and immunosuppressive therapy.
There were no differences in baseline values of TcPO2 between the groups, and similar improvements were seen in both the ACT and re-PTA groups versus conservative group.
ACT in practice
With such promising results, what about the practicalities of harvesting a patient’s bone marrow to make the ACT?
“Bone marrow harvesting usually takes about 20 minutes,” Dr. Dubský said. It then takes another 45 minutes to separate the cells and make the cell suspension, and then maybe another 10 minutes or so to administer this to the patient, which is done by injecting into the calf muscles and small muscles of the foot, aided by computed tomography. The whole process may take up to 2 hours, he said.
“Patients are under local or general anesthesia, so there is no pain during the procedure,” Dr. Dubský reassured. “Afterwards we sometimes see small hematoma[s], with low-intensity pain that responds well to usual analgesic therapy.”
Computed tomography was used to help guide the injections, which was advantageous, Dr. Boulton pointed out, because it was “less invasive than angioplasty in these very sick people with very distal lesions, many of whom already have renal problems.”
“It is surprising though, that everybody had re-PTA and not one had vascular surgery,” he suggested. Dr. Boulton added, however: “These are very important observations; they help us a lot in an area where there’s unlikely to be a full RCT.”
The next step in this research is to see if combining ACT and re-PTA could lead to even better results.
The study was funded by the Czech Republic Ministry of Health. Dr. Dubský had nothing to disclose. Dr. Boulton made no statement about his conflicts of interest.
Bone marrow derived autologous cell therapy (ACT) has been shown to significantly reduce the rate of major amputation at 5 years in people with diabetes who developed critical limb-threatening ischemia (CLTI).
In a study of 130 patients, 64% of 42 patients who were treated conservatively needed a major amputation at 5 years versus just 30% of 45 patients who had been treated with ACT (P = .011).
This compared favorably to the results seen with repeated percutaneous angioplasty (re-PTA), where just 20.9% of 43 patients underwent limb salvage (P = .002 vs. conservative therapy).
Furthermore, amputation-free survival was significantly longer in both active groups, Michal Dubský, MD, PhD, FRSPH, reported at the annual meeting of the European Association for the Study of Diabetes.
Dr. Dubský, of the Institute for Clinical and Experimental Medicine and Charles University in Prague, also reported that fewer patients who had undergone re-PTA or ACT than conservative treatment had died by 5 years (25.8% and 35.6%, respectively, vs. 61.9%), but that the difference was significant only for the revascularization procedure (P = .012).
Based on these findings, “we believe that autologous cell therapy seems to be an appropriate alternative to repeated PTA even for patients with no-option chronic limb-threatening ischemia,” he said.
“This is a very important area,” said Andrew J.M. Boulton, MBBS, MD, FRCP, who chaired the oral abstract presentation session during which the findings were presented.
“It is very difficult to get an evidence base from randomized studies in this area, because of the nature of the patients: They’re very sick and we all deal with them in our clinics very regularly,” added Dr. Boulton, professor of medicine within the division of diabetes, endocrinology and gastroenterology at the University of Manchester (England).
Dr. Boulton called the findings a “very important addition to what we know.”
New option for no-option CLTI
CLTI is associated with persistent pain at rest, ulcers, and gangrene, and can be the end result of longstanding peripheral arterial disease. Within the first year of presentation, there’s a 30% chance of having a major amputation and a 25% chance of dying.
Importantly, said Dr. Dubský, “there is a big difference in this diagnosis” between patients with diabetes and those without. For instance, CLTI is more diffuse in patients with diabetes than in those without, different arteries are affected and the sclerosis seen can be more rigid and “full of calcium.”
While surgery to improve blood flow is the standard of care, not everyone is suitable. Bypass surgery or endovascular procedures can be performed in only 40%-50% of patients, and even then a therapeutic effect may be seen in only a quarter of patients.
“We need some new therapeutic modalities for this diagnosis, and one of them could be autologous cell therapy,” said Dr. Dubský.
Study details
Dr. Dubský and coinvestigators consecutively recruited 130 patients with diabetic foot and CLTI who had been seen at their clinic over a 5-year period. Of these, 87 had not been eligible for standard revascularization and underwent ACT or were treated conservatively.
Of the patients who were not eligible for standard revascularization (‘no-option CLTI), 45 had undergone ACT and 42 had been treated conservatively. Dr. Dubský acknowledged that “his study was not prospective and randomized.”
All patients in the study had at least one unsuccessful revascularization procedure and diabetic foot ulcers, and low tissue oxygenation. The latter was defined as transcutaneous oxygen pressure (TcPO2) of below 30 mm Hg.
There were little differences in demographic characteristics between the treatment groups, the average age ranged from 62 to 67 years, there were more men (70%-80%) than women; most patients (90%) had type 2 diabetes for at least 20 years. There were similar rates of ischemic heart disease, hypertension, dialysis, and immunosuppressive therapy.
There were no differences in baseline values of TcPO2 between the groups, and similar improvements were seen in both the ACT and re-PTA groups versus conservative group.
ACT in practice
With such promising results, what about the practicalities of harvesting a patient’s bone marrow to make the ACT?
“Bone marrow harvesting usually takes about 20 minutes,” Dr. Dubský said. It then takes another 45 minutes to separate the cells and make the cell suspension, and then maybe another 10 minutes or so to administer this to the patient, which is done by injecting into the calf muscles and small muscles of the foot, aided by computed tomography. The whole process may take up to 2 hours, he said.
“Patients are under local or general anesthesia, so there is no pain during the procedure,” Dr. Dubský reassured. “Afterwards we sometimes see small hematoma[s], with low-intensity pain that responds well to usual analgesic therapy.”
Computed tomography was used to help guide the injections, which was advantageous, Dr. Boulton pointed out, because it was “less invasive than angioplasty in these very sick people with very distal lesions, many of whom already have renal problems.”
“It is surprising though, that everybody had re-PTA and not one had vascular surgery,” he suggested. Dr. Boulton added, however: “These are very important observations; they help us a lot in an area where there’s unlikely to be a full RCT.”
The next step in this research is to see if combining ACT and re-PTA could lead to even better results.
The study was funded by the Czech Republic Ministry of Health. Dr. Dubský had nothing to disclose. Dr. Boulton made no statement about his conflicts of interest.
FROM EASD 2021
Retinopathy risk higher in young-onset T2D, more so in men
Men diagnosed with type 2 diabetes (T2D) by the age of 40 years appear significantly more likely to develop retinopathy than men who are diagnosed at an older age, Norwegian researchers report.
In a cross-sectional study of about 10,000 people, men with young-onset T2D were 72% more likely than men aged 50 years or older to have retinopathy.
While an increased retinopathy risk was also seen in women with young-onset T2D versus older women at first, this difference was not significant after adjusting for various confounding factors.
The effect of young-onset diabetes on retinopathy seems to be gender specific, Katrina Tibballs, MD, of the department of general practice at the University of Oslo, reported at the annual meeting of the European Association for the Study of Diabetes.
“In the unadjusted analysis, the odds ratio for retinopathy was substantially higher in both [young-onset] men [odds ratio, 3.0] and women [OR, 2.46], compared with those 50 or older at diabetes diagnosis,” Dr. Tibballs said.
That relationship was not substantially altered after adjustment for variables such as level of education, country background, gender, and body mass index, with adjusted ORs of 2.56 and 2.55 for men and women, respectively.
However, further adjustment to include current age, duration of diabetes, and blood lipids and glycated hemoglobin levels, led to the difference no longer holding for women (OR, 1.34; 95% confidence interval, 0.95-1.89) as it did for men (OR 1.72; 95% CI, 1.29-2.29).
First data in Norwegian population
Cross-sectional data on more than 10,000 people with T2D were used for the analysis. These came from the ROSA4 study, a general practice study conducted across Norway in 2014.
Just over 10% of the study population used in the analysis was under the age of 40 years at diagnosis of T2D; 21% were aged between 40 and 49 years, and 69% were at least 50 years old.
The mean age of those with young-onset T2D, defined as a diagnosis before the age of 40 years, was 33 years. These individuals had a longer disease duration than those in the other age groups (11.4 vs. 10.0 vs. 7.8 years).
“Looking at clinical characteristics, we say that individuals [with young-onset T2D] have a higher level of hemoglobin A1c than those with diabetes onset later in life,” Dr. Tibballs said.
“This is despite a substantially higher proportion [being] treated with insulin and fewer on lifestyle interventions alone.”
Gender differences were seen in A1c levels, with men with young-onset T2D having consistently higher levels than women, with levels increasing with diabetes duration.
Rise in retinopathy faster in men than in women
Dr. Tibballs reported that, not only did the prevalence of retinopathy rise faster in those of a younger age, but it also rose more quickly in men with young-onset T2D than it in their female counterparts.
“Comparing that [young-onset diabetes] and later-onset diabetes in men and women separately, we see a clearly higher prevalence of retinopathy with increasing diabetes duration for [young-onset] men,” she said.
In women, on the other hand, there was “no clear indication of a higher retinopathy prevalence in [young-onset diabetes], except in those with the longest diabetes duration.”
So, what do the results mean for practice? First, they confirm prior work showing that there is a strong association between retinopathy and age at diagnosis of T2D. Second, they suggest that this is despite intensive glucose-lowering treatment.
She speculated that men with young-onset T2D may have had a delayed diagnosis when compared with women and individuals with later onset diabetes, Dr. Tibballs said.
“This may in turn lead to delayed onset of glucose-lowering treatment, allowing for more time with high glycemic exposure and increased risk of acquiring complications, such as retinopathy at the time of diagnosis, or in the first years after,” said Dr. Tibballs.
These are cross-sectional data, “so we can’t say anything about whether this treatment is sufficient, but it is obviously not reducing HbA1c levels as much as we would like” added Dr. Tibballs, who is a primary care physician and PhD student.
The study was supported by The Norwegian Research Fund for General Practice. Dr. Tibballs had no conflicts of interest to disclose.
Men diagnosed with type 2 diabetes (T2D) by the age of 40 years appear significantly more likely to develop retinopathy than men who are diagnosed at an older age, Norwegian researchers report.
In a cross-sectional study of about 10,000 people, men with young-onset T2D were 72% more likely than men aged 50 years or older to have retinopathy.
While an increased retinopathy risk was also seen in women with young-onset T2D versus older women at first, this difference was not significant after adjusting for various confounding factors.
The effect of young-onset diabetes on retinopathy seems to be gender specific, Katrina Tibballs, MD, of the department of general practice at the University of Oslo, reported at the annual meeting of the European Association for the Study of Diabetes.
“In the unadjusted analysis, the odds ratio for retinopathy was substantially higher in both [young-onset] men [odds ratio, 3.0] and women [OR, 2.46], compared with those 50 or older at diabetes diagnosis,” Dr. Tibballs said.
That relationship was not substantially altered after adjustment for variables such as level of education, country background, gender, and body mass index, with adjusted ORs of 2.56 and 2.55 for men and women, respectively.
However, further adjustment to include current age, duration of diabetes, and blood lipids and glycated hemoglobin levels, led to the difference no longer holding for women (OR, 1.34; 95% confidence interval, 0.95-1.89) as it did for men (OR 1.72; 95% CI, 1.29-2.29).
First data in Norwegian population
Cross-sectional data on more than 10,000 people with T2D were used for the analysis. These came from the ROSA4 study, a general practice study conducted across Norway in 2014.
Just over 10% of the study population used in the analysis was under the age of 40 years at diagnosis of T2D; 21% were aged between 40 and 49 years, and 69% were at least 50 years old.
The mean age of those with young-onset T2D, defined as a diagnosis before the age of 40 years, was 33 years. These individuals had a longer disease duration than those in the other age groups (11.4 vs. 10.0 vs. 7.8 years).
“Looking at clinical characteristics, we say that individuals [with young-onset T2D] have a higher level of hemoglobin A1c than those with diabetes onset later in life,” Dr. Tibballs said.
“This is despite a substantially higher proportion [being] treated with insulin and fewer on lifestyle interventions alone.”
Gender differences were seen in A1c levels, with men with young-onset T2D having consistently higher levels than women, with levels increasing with diabetes duration.
Rise in retinopathy faster in men than in women
Dr. Tibballs reported that, not only did the prevalence of retinopathy rise faster in those of a younger age, but it also rose more quickly in men with young-onset T2D than it in their female counterparts.
“Comparing that [young-onset diabetes] and later-onset diabetes in men and women separately, we see a clearly higher prevalence of retinopathy with increasing diabetes duration for [young-onset] men,” she said.
In women, on the other hand, there was “no clear indication of a higher retinopathy prevalence in [young-onset diabetes], except in those with the longest diabetes duration.”
So, what do the results mean for practice? First, they confirm prior work showing that there is a strong association between retinopathy and age at diagnosis of T2D. Second, they suggest that this is despite intensive glucose-lowering treatment.
She speculated that men with young-onset T2D may have had a delayed diagnosis when compared with women and individuals with later onset diabetes, Dr. Tibballs said.
“This may in turn lead to delayed onset of glucose-lowering treatment, allowing for more time with high glycemic exposure and increased risk of acquiring complications, such as retinopathy at the time of diagnosis, or in the first years after,” said Dr. Tibballs.
These are cross-sectional data, “so we can’t say anything about whether this treatment is sufficient, but it is obviously not reducing HbA1c levels as much as we would like” added Dr. Tibballs, who is a primary care physician and PhD student.
The study was supported by The Norwegian Research Fund for General Practice. Dr. Tibballs had no conflicts of interest to disclose.
Men diagnosed with type 2 diabetes (T2D) by the age of 40 years appear significantly more likely to develop retinopathy than men who are diagnosed at an older age, Norwegian researchers report.
In a cross-sectional study of about 10,000 people, men with young-onset T2D were 72% more likely than men aged 50 years or older to have retinopathy.
While an increased retinopathy risk was also seen in women with young-onset T2D versus older women at first, this difference was not significant after adjusting for various confounding factors.
The effect of young-onset diabetes on retinopathy seems to be gender specific, Katrina Tibballs, MD, of the department of general practice at the University of Oslo, reported at the annual meeting of the European Association for the Study of Diabetes.
“In the unadjusted analysis, the odds ratio for retinopathy was substantially higher in both [young-onset] men [odds ratio, 3.0] and women [OR, 2.46], compared with those 50 or older at diabetes diagnosis,” Dr. Tibballs said.
That relationship was not substantially altered after adjustment for variables such as level of education, country background, gender, and body mass index, with adjusted ORs of 2.56 and 2.55 for men and women, respectively.
However, further adjustment to include current age, duration of diabetes, and blood lipids and glycated hemoglobin levels, led to the difference no longer holding for women (OR, 1.34; 95% confidence interval, 0.95-1.89) as it did for men (OR 1.72; 95% CI, 1.29-2.29).
First data in Norwegian population
Cross-sectional data on more than 10,000 people with T2D were used for the analysis. These came from the ROSA4 study, a general practice study conducted across Norway in 2014.
Just over 10% of the study population used in the analysis was under the age of 40 years at diagnosis of T2D; 21% were aged between 40 and 49 years, and 69% were at least 50 years old.
The mean age of those with young-onset T2D, defined as a diagnosis before the age of 40 years, was 33 years. These individuals had a longer disease duration than those in the other age groups (11.4 vs. 10.0 vs. 7.8 years).
“Looking at clinical characteristics, we say that individuals [with young-onset T2D] have a higher level of hemoglobin A1c than those with diabetes onset later in life,” Dr. Tibballs said.
“This is despite a substantially higher proportion [being] treated with insulin and fewer on lifestyle interventions alone.”
Gender differences were seen in A1c levels, with men with young-onset T2D having consistently higher levels than women, with levels increasing with diabetes duration.
Rise in retinopathy faster in men than in women
Dr. Tibballs reported that, not only did the prevalence of retinopathy rise faster in those of a younger age, but it also rose more quickly in men with young-onset T2D than it in their female counterparts.
“Comparing that [young-onset diabetes] and later-onset diabetes in men and women separately, we see a clearly higher prevalence of retinopathy with increasing diabetes duration for [young-onset] men,” she said.
In women, on the other hand, there was “no clear indication of a higher retinopathy prevalence in [young-onset diabetes], except in those with the longest diabetes duration.”
So, what do the results mean for practice? First, they confirm prior work showing that there is a strong association between retinopathy and age at diagnosis of T2D. Second, they suggest that this is despite intensive glucose-lowering treatment.
She speculated that men with young-onset T2D may have had a delayed diagnosis when compared with women and individuals with later onset diabetes, Dr. Tibballs said.
“This may in turn lead to delayed onset of glucose-lowering treatment, allowing for more time with high glycemic exposure and increased risk of acquiring complications, such as retinopathy at the time of diagnosis, or in the first years after,” said Dr. Tibballs.
These are cross-sectional data, “so we can’t say anything about whether this treatment is sufficient, but it is obviously not reducing HbA1c levels as much as we would like” added Dr. Tibballs, who is a primary care physician and PhD student.
The study was supported by The Norwegian Research Fund for General Practice. Dr. Tibballs had no conflicts of interest to disclose.
FROM EASD 2021