User login
Studies link TMAO to microbiome, reveal new heart disease target
MIAMI – Researchers are one step closer to developing “drugs for bugs” – agents that target the gut microbiome to prevent and treat cardiometabolic diseases, Stanley L. Hazen, MD, PhD, said at the 2019 Gut Microbiota for Health World Summit.
“Each person experiences a meal differently through the filter of their gut microbiome, which helps explain individual differences in susceptibility to disease,” said Dr. Hazen of Cleveland Clinic. “In the future, our medicine cabinets will have drugs in them that not only affect us, but also target the microbial enzymes that affect levels of metabolites like TMAO.”
Trimethylamine N-oxide (TMAO) is produced by gut bacteria. High levels (in one study, approximately 6.2 micromolar) significantly increase the risk of major adverse cardiovascular events even after controlling for traditional demographic and clinical risk factors. Studies indicate that TMAO alters cholesterol and bile acid metabolism, upregulates inflammatory pathways, and promotes foam cell formation, all of which worsen atherosclerosis. In addition, TMAO increases clotting risk by enhancing platelet reactivity.
“Reducing the amount of animal products in one’s diet helps reduce TMAO levels,” said Dr. Hazen. Certain fish – mainly those found in deep, cold water, such as cod – are high in TMAO. However, a bigger culprit in the United States is red meat, which contains two major TMAO precursors – choline and carnitine. In a recent study, Dr. Hazen and his associates gave 113 healthy volunteers three isocaloric diets in random order based on red meat, white meat, or plant-based protein. After 4 weeks, eating the daily equivalent of 8 ounces of steak or two quarter-pound beef patties nearly tripled plasma TMAO levels (P less than .05) from baseline. The white meat and vegetarian diets showed no such effect.
Crucially, the effect of red meat was reversible – TMAO levels fell significantly within 4 weeks after participants stopped consuming red meat. Eating red meat low in saturated fat did not prevent TMAO levels from rising, Dr. Hazen noted at the meeting at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
In a second study, Dr. Hazen and his associates identified a two-step process by which gut bacteria metabolize carnitine to TMAO. The second step was greatly enhanced in individuals who eat red meat, suggesting a possible therapeutic target. In a third study, they found that high TMAO levels in mice fell significantly with a single oral dose of a second-generation inhibitor of trimethylamine lyase, the enzyme used by gut bacteria to convert choline to TMAO. The inhibitory effect was irreversible, did not reduce the viability of commensal microorganisms, and significantly lowered platelet hyperreactivity and clot formation.
Such results are exciting, but “drugs for bugs” will exhibit varying effects depending on which gut species are present at baseline, Dr. Hazen explained. Investigators will need to understand and account for these differences before therapies for the microbiome can enter the clinic. For now, a blood test for TMAO is available and can help clinicians tailor their suggestions on what to eat.
Dr. Hazen disclosed a consulting relationship with Proctor & Gamble, royalties for patents from Proctor & Gamble, Cleveland Heart Lab, and Quest Diagnostics, and research support from AstraZeneca, Pfizer, Roche Diagnostics, and Proctor & Gamble.
MIAMI – Researchers are one step closer to developing “drugs for bugs” – agents that target the gut microbiome to prevent and treat cardiometabolic diseases, Stanley L. Hazen, MD, PhD, said at the 2019 Gut Microbiota for Health World Summit.
“Each person experiences a meal differently through the filter of their gut microbiome, which helps explain individual differences in susceptibility to disease,” said Dr. Hazen of Cleveland Clinic. “In the future, our medicine cabinets will have drugs in them that not only affect us, but also target the microbial enzymes that affect levels of metabolites like TMAO.”
Trimethylamine N-oxide (TMAO) is produced by gut bacteria. High levels (in one study, approximately 6.2 micromolar) significantly increase the risk of major adverse cardiovascular events even after controlling for traditional demographic and clinical risk factors. Studies indicate that TMAO alters cholesterol and bile acid metabolism, upregulates inflammatory pathways, and promotes foam cell formation, all of which worsen atherosclerosis. In addition, TMAO increases clotting risk by enhancing platelet reactivity.
“Reducing the amount of animal products in one’s diet helps reduce TMAO levels,” said Dr. Hazen. Certain fish – mainly those found in deep, cold water, such as cod – are high in TMAO. However, a bigger culprit in the United States is red meat, which contains two major TMAO precursors – choline and carnitine. In a recent study, Dr. Hazen and his associates gave 113 healthy volunteers three isocaloric diets in random order based on red meat, white meat, or plant-based protein. After 4 weeks, eating the daily equivalent of 8 ounces of steak or two quarter-pound beef patties nearly tripled plasma TMAO levels (P less than .05) from baseline. The white meat and vegetarian diets showed no such effect.
Crucially, the effect of red meat was reversible – TMAO levels fell significantly within 4 weeks after participants stopped consuming red meat. Eating red meat low in saturated fat did not prevent TMAO levels from rising, Dr. Hazen noted at the meeting at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
In a second study, Dr. Hazen and his associates identified a two-step process by which gut bacteria metabolize carnitine to TMAO. The second step was greatly enhanced in individuals who eat red meat, suggesting a possible therapeutic target. In a third study, they found that high TMAO levels in mice fell significantly with a single oral dose of a second-generation inhibitor of trimethylamine lyase, the enzyme used by gut bacteria to convert choline to TMAO. The inhibitory effect was irreversible, did not reduce the viability of commensal microorganisms, and significantly lowered platelet hyperreactivity and clot formation.
Such results are exciting, but “drugs for bugs” will exhibit varying effects depending on which gut species are present at baseline, Dr. Hazen explained. Investigators will need to understand and account for these differences before therapies for the microbiome can enter the clinic. For now, a blood test for TMAO is available and can help clinicians tailor their suggestions on what to eat.
Dr. Hazen disclosed a consulting relationship with Proctor & Gamble, royalties for patents from Proctor & Gamble, Cleveland Heart Lab, and Quest Diagnostics, and research support from AstraZeneca, Pfizer, Roche Diagnostics, and Proctor & Gamble.
MIAMI – Researchers are one step closer to developing “drugs for bugs” – agents that target the gut microbiome to prevent and treat cardiometabolic diseases, Stanley L. Hazen, MD, PhD, said at the 2019 Gut Microbiota for Health World Summit.
“Each person experiences a meal differently through the filter of their gut microbiome, which helps explain individual differences in susceptibility to disease,” said Dr. Hazen of Cleveland Clinic. “In the future, our medicine cabinets will have drugs in them that not only affect us, but also target the microbial enzymes that affect levels of metabolites like TMAO.”
Trimethylamine N-oxide (TMAO) is produced by gut bacteria. High levels (in one study, approximately 6.2 micromolar) significantly increase the risk of major adverse cardiovascular events even after controlling for traditional demographic and clinical risk factors. Studies indicate that TMAO alters cholesterol and bile acid metabolism, upregulates inflammatory pathways, and promotes foam cell formation, all of which worsen atherosclerosis. In addition, TMAO increases clotting risk by enhancing platelet reactivity.
“Reducing the amount of animal products in one’s diet helps reduce TMAO levels,” said Dr. Hazen. Certain fish – mainly those found in deep, cold water, such as cod – are high in TMAO. However, a bigger culprit in the United States is red meat, which contains two major TMAO precursors – choline and carnitine. In a recent study, Dr. Hazen and his associates gave 113 healthy volunteers three isocaloric diets in random order based on red meat, white meat, or plant-based protein. After 4 weeks, eating the daily equivalent of 8 ounces of steak or two quarter-pound beef patties nearly tripled plasma TMAO levels (P less than .05) from baseline. The white meat and vegetarian diets showed no such effect.
Crucially, the effect of red meat was reversible – TMAO levels fell significantly within 4 weeks after participants stopped consuming red meat. Eating red meat low in saturated fat did not prevent TMAO levels from rising, Dr. Hazen noted at the meeting at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
In a second study, Dr. Hazen and his associates identified a two-step process by which gut bacteria metabolize carnitine to TMAO. The second step was greatly enhanced in individuals who eat red meat, suggesting a possible therapeutic target. In a third study, they found that high TMAO levels in mice fell significantly with a single oral dose of a second-generation inhibitor of trimethylamine lyase, the enzyme used by gut bacteria to convert choline to TMAO. The inhibitory effect was irreversible, did not reduce the viability of commensal microorganisms, and significantly lowered platelet hyperreactivity and clot formation.
Such results are exciting, but “drugs for bugs” will exhibit varying effects depending on which gut species are present at baseline, Dr. Hazen explained. Investigators will need to understand and account for these differences before therapies for the microbiome can enter the clinic. For now, a blood test for TMAO is available and can help clinicians tailor their suggestions on what to eat.
Dr. Hazen disclosed a consulting relationship with Proctor & Gamble, royalties for patents from Proctor & Gamble, Cleveland Heart Lab, and Quest Diagnostics, and research support from AstraZeneca, Pfizer, Roche Diagnostics, and Proctor & Gamble.
REPORTING FROM GMFH 2019
Western diet linked to lower microbiome diversity
MIAMI – Eating a Western diet correlated with significantly lower gut microbiome diversity in an observational study of 1,000 healthy men and women.
The chief culprits were fried foods, sodas, fatty sweets, processed meats, ready-cooked meals, and desserts, reported Valentin Partula, a PhD student at the Université Paris 13 Nord and his associates. The more often individuals reported consuming these, the fewer bacterial species were identified in their stool (P less than .05 for each association), the investigators wrote in a poster presented at the annual Gut Microbiota for Health World Summit.
Studies have linked decreased microbiota diversity with health conditions ranging from inflammatory bowel disease and colorectal cancer to diabetes mellitus. Obesity also is characterized by a less diverse microbiome and is linked to many of the same diseases, but the diversity (richness) of the gut microbiome appears to have more to do with diet than body mass index. However, interventional studies linking diet to microbiome shifts often have been small, narrow in scope, and short in duration, the researchers noted at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
To help fill these gaps, they administered a 19-item food-frequency questionnaire to 1,000 healthy men and women in France who were 20-69 years old. Each food question had six possible responses, ranging from “at least twice a day” to “never.” For 862 of these men and women, the researchers also analyzed stool samples using 16S rRNA sequencing – a standard test for microbiome diversity. These sequencing results were analyzed in terms of both alpha diversity (the number of species within a sample, and the relative abundance of each) and beta diversity (the degree of dissimilarity among different individuals).
The most significant correlate of low alpha diversity (that is, a less diverse gut microbiome) was frequent consumption of fried foods, followed by sodas or sugary drinks, fatty sweet products, processed meats, ready-cooked meals, and desserts (P less than .05 for each). Conversely, raw fruits and fish each correlated with having a richer microbiome (P less than .05). Consuming eggs and raw and cooked vegetables also correlated with greater diversity, but these associations did not reach statistical significance.
In terms of beta diversity (uniqueness of the microbiome signature), the strongest correlates were fresh fruit, fried products, ready-cooked meals, and cheese. The finding for fresh fruit might be an effect of weighting but needs further study, the researchers said. Taken together, however, the findings “extend and support mechanistic arguments linking Western diet to altered microbiota composition,” they said.
Next, they looked at how specific foods correlated with specific bacterial taxa. Consuming more dairy correlated with a greater abundance of Streptococcus salivarius, which disrupts S. pyogenes biofilms in the pharynx and thus might help prevent bacterial pharyngitis. Eating raw fruits was tied to increases in Eubacterium eligens, a nonpathogenic bacterium whose role in the gut remains unclear. Finally, frequent cheese consumption was linked to lower abundance of Akkermansia muciniphila, a bacterium that is thought to benefit metabolic pathways and immune signaling.
For the same 846 individuals, the researchers performed 1hydrogen nuclear magnetic resonance metabolomic tests on plasma Carr-Purcell-Meiboom-Gill (CPMG)–pulse sequence and nuclear Overhauser enhancement spectroscopy (NOESY). Increased creatinine was associated with the highest number of bacterial taxa and might reflect effects on kidney function or trimethylamine N-oxide, they wrote. Greater microbiome diversity correlated with higher plasma levels of amino acids, proteins, creatinine, choline, glucose, and citrate. Lower diversity was tied to the presence of lipid-based metabolites, including ketones and esters.
The next step is to confirm the findings in a separate population and establish which of these associations are probably causal, the researchers wrote. “Mechanistic studies elucidating the metabolic capability of the organisms [also] are needed.”
No external funding sources or conflicts of interest were reported.
MIAMI – Eating a Western diet correlated with significantly lower gut microbiome diversity in an observational study of 1,000 healthy men and women.
The chief culprits were fried foods, sodas, fatty sweets, processed meats, ready-cooked meals, and desserts, reported Valentin Partula, a PhD student at the Université Paris 13 Nord and his associates. The more often individuals reported consuming these, the fewer bacterial species were identified in their stool (P less than .05 for each association), the investigators wrote in a poster presented at the annual Gut Microbiota for Health World Summit.
Studies have linked decreased microbiota diversity with health conditions ranging from inflammatory bowel disease and colorectal cancer to diabetes mellitus. Obesity also is characterized by a less diverse microbiome and is linked to many of the same diseases, but the diversity (richness) of the gut microbiome appears to have more to do with diet than body mass index. However, interventional studies linking diet to microbiome shifts often have been small, narrow in scope, and short in duration, the researchers noted at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
To help fill these gaps, they administered a 19-item food-frequency questionnaire to 1,000 healthy men and women in France who were 20-69 years old. Each food question had six possible responses, ranging from “at least twice a day” to “never.” For 862 of these men and women, the researchers also analyzed stool samples using 16S rRNA sequencing – a standard test for microbiome diversity. These sequencing results were analyzed in terms of both alpha diversity (the number of species within a sample, and the relative abundance of each) and beta diversity (the degree of dissimilarity among different individuals).
The most significant correlate of low alpha diversity (that is, a less diverse gut microbiome) was frequent consumption of fried foods, followed by sodas or sugary drinks, fatty sweet products, processed meats, ready-cooked meals, and desserts (P less than .05 for each). Conversely, raw fruits and fish each correlated with having a richer microbiome (P less than .05). Consuming eggs and raw and cooked vegetables also correlated with greater diversity, but these associations did not reach statistical significance.
In terms of beta diversity (uniqueness of the microbiome signature), the strongest correlates were fresh fruit, fried products, ready-cooked meals, and cheese. The finding for fresh fruit might be an effect of weighting but needs further study, the researchers said. Taken together, however, the findings “extend and support mechanistic arguments linking Western diet to altered microbiota composition,” they said.
Next, they looked at how specific foods correlated with specific bacterial taxa. Consuming more dairy correlated with a greater abundance of Streptococcus salivarius, which disrupts S. pyogenes biofilms in the pharynx and thus might help prevent bacterial pharyngitis. Eating raw fruits was tied to increases in Eubacterium eligens, a nonpathogenic bacterium whose role in the gut remains unclear. Finally, frequent cheese consumption was linked to lower abundance of Akkermansia muciniphila, a bacterium that is thought to benefit metabolic pathways and immune signaling.
For the same 846 individuals, the researchers performed 1hydrogen nuclear magnetic resonance metabolomic tests on plasma Carr-Purcell-Meiboom-Gill (CPMG)–pulse sequence and nuclear Overhauser enhancement spectroscopy (NOESY). Increased creatinine was associated with the highest number of bacterial taxa and might reflect effects on kidney function or trimethylamine N-oxide, they wrote. Greater microbiome diversity correlated with higher plasma levels of amino acids, proteins, creatinine, choline, glucose, and citrate. Lower diversity was tied to the presence of lipid-based metabolites, including ketones and esters.
The next step is to confirm the findings in a separate population and establish which of these associations are probably causal, the researchers wrote. “Mechanistic studies elucidating the metabolic capability of the organisms [also] are needed.”
No external funding sources or conflicts of interest were reported.
MIAMI – Eating a Western diet correlated with significantly lower gut microbiome diversity in an observational study of 1,000 healthy men and women.
The chief culprits were fried foods, sodas, fatty sweets, processed meats, ready-cooked meals, and desserts, reported Valentin Partula, a PhD student at the Université Paris 13 Nord and his associates. The more often individuals reported consuming these, the fewer bacterial species were identified in their stool (P less than .05 for each association), the investigators wrote in a poster presented at the annual Gut Microbiota for Health World Summit.
Studies have linked decreased microbiota diversity with health conditions ranging from inflammatory bowel disease and colorectal cancer to diabetes mellitus. Obesity also is characterized by a less diverse microbiome and is linked to many of the same diseases, but the diversity (richness) of the gut microbiome appears to have more to do with diet than body mass index. However, interventional studies linking diet to microbiome shifts often have been small, narrow in scope, and short in duration, the researchers noted at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
To help fill these gaps, they administered a 19-item food-frequency questionnaire to 1,000 healthy men and women in France who were 20-69 years old. Each food question had six possible responses, ranging from “at least twice a day” to “never.” For 862 of these men and women, the researchers also analyzed stool samples using 16S rRNA sequencing – a standard test for microbiome diversity. These sequencing results were analyzed in terms of both alpha diversity (the number of species within a sample, and the relative abundance of each) and beta diversity (the degree of dissimilarity among different individuals).
The most significant correlate of low alpha diversity (that is, a less diverse gut microbiome) was frequent consumption of fried foods, followed by sodas or sugary drinks, fatty sweet products, processed meats, ready-cooked meals, and desserts (P less than .05 for each). Conversely, raw fruits and fish each correlated with having a richer microbiome (P less than .05). Consuming eggs and raw and cooked vegetables also correlated with greater diversity, but these associations did not reach statistical significance.
In terms of beta diversity (uniqueness of the microbiome signature), the strongest correlates were fresh fruit, fried products, ready-cooked meals, and cheese. The finding for fresh fruit might be an effect of weighting but needs further study, the researchers said. Taken together, however, the findings “extend and support mechanistic arguments linking Western diet to altered microbiota composition,” they said.
Next, they looked at how specific foods correlated with specific bacterial taxa. Consuming more dairy correlated with a greater abundance of Streptococcus salivarius, which disrupts S. pyogenes biofilms in the pharynx and thus might help prevent bacterial pharyngitis. Eating raw fruits was tied to increases in Eubacterium eligens, a nonpathogenic bacterium whose role in the gut remains unclear. Finally, frequent cheese consumption was linked to lower abundance of Akkermansia muciniphila, a bacterium that is thought to benefit metabolic pathways and immune signaling.
For the same 846 individuals, the researchers performed 1hydrogen nuclear magnetic resonance metabolomic tests on plasma Carr-Purcell-Meiboom-Gill (CPMG)–pulse sequence and nuclear Overhauser enhancement spectroscopy (NOESY). Increased creatinine was associated with the highest number of bacterial taxa and might reflect effects on kidney function or trimethylamine N-oxide, they wrote. Greater microbiome diversity correlated with higher plasma levels of amino acids, proteins, creatinine, choline, glucose, and citrate. Lower diversity was tied to the presence of lipid-based metabolites, including ketones and esters.
The next step is to confirm the findings in a separate population and establish which of these associations are probably causal, the researchers wrote. “Mechanistic studies elucidating the metabolic capability of the organisms [also] are needed.”
No external funding sources or conflicts of interest were reported.
REPORTING FROM GMFH 2019
Hyperglycemia drives leaky gut syndrome, inflammation
MIAMI – Hyperglycemia increases intestinal permeability, which facilitates enteric infections and systemic inflammation, reported Christoph Thaiss, PhD.
The findings upend the old idea that intestinal barrier dysfunction leads to diabetes, Dr. Thaiss said during a plenary session at the annual Gut Microbiota for Health World Summit. Multiple mouse models link hyperglycemia to intestinal barrier dysfunction, and hemoglobin A1C (HbA1c) levels in humans “highly correlate with the influx of microbial molecules into the intestinal epithelium.”
Researchers often struggle to decide if apparent causes are really confounders or even downstream results (reverse causation). In the metabolic syndrome, patients are known to have increased intestinal permeability – so-called leaky gut – and microbes crossing the gastrointestinal epithelium have been found to cause both gut mucosal infections and chronic systemic inflammation. But because these mechanisms were poorly understood, some experts posited that intestinal barrier dysfunction induced pancreatic beta cell inflammation, insulin resistance, and diabetes.
To take a deeper dive, Dr. Thaiss and his associates at the University of Pennsylvania, Philadelphia started with a mouse model of morbid obesity. The mice had multiple systemic sites with microbial pattern recognition ligands, signifying microbial influx from the gut. They also had genetic signatures indicating a marked disruption of junctions between epithelial cells, compared with healthy controls.
The obese mice also were much more susceptible to enteric infections with Citrobacter rodentium (a Salmonella analog), but obesity itself did not drive this risk, Dr. Thaiss explained. In fact, two different murine models of nonobese type 1 diabetes mellitus showed “leaky” intestinal epithelial adherence junctions, heightened susceptibility to C. rodentium infection, and showed systemic pathogen spread. Ribosomal DNA sequencing showed that these hyperglycemic (diabetic) mice had shifts in their gut microbiomes; however, translocating the altered microbiota to normal mice did not make them more susceptible to enteric infections or systemic inflammation.
Based on these findings, the researchers hypothesized that hyperglycemia itself drove susceptibility to enteric infections. They confirmed this by administering insulin to the mice with type 1 diabetes, which restored intestinal epithelial adherence junctions and stopped the systemic spread of pathogens. In vitro, exposing intestinal epithelial cells to glucose-induced barrier dysfunctions that increased over time and with higher glucose concentrations. RNA sequencing demonstrated that hyperglycemia markedly changed expression of genes that encode proteins that regulate intestinal barrier function. Moreover, hyperglycemic mice lacking the bidirectional glucose transporter GLUT2 showed no intestinal barrier dysfunction and were not susceptible to C. rodentium infection and systemic spread.
Finally, the investigators studied more than 30 clinical measures and microbial products in the systemic circulation of 27 healthy human volunteers. “Of all the variables we measured, HbA1c showed the strongest correlation with the influx of microbial molecules,” said Dr. Thaiss. Serum HbA1c correlated highly (P = .008) with levels of toll-like receptor 4, an indicator of systemic pathogens, but not with body mass index (P = .76).
The findings in humans confirm those in mice and indicate that hyperglycemia is a direct cause of intestinal barrier dysfunction and susceptibility to enteric infection, Dr. Thaiss said, adding that the systemic influx of microbial products might explain the wide range of otherwise unrelated inflammatory conditions seen in patients with metabolic syndrome. Future studies of therapies for enteric infection and systemic inflammation might focus on glucose as a modifier of intestinal barrier function.
These findings, reported at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, were also published in Science.
The work was supported by a Boehringer Ingelheim Funds PhD fellowship, the Leona M. and Harry B. Helmsley Charitable Trust, the Adelis Foundation, the Gurwin Family Fund for Scientific Research, the Crown Endowment Fund for Immunological Research, and others. Dr. Thaiss and his coinvestigators reported having no conflicts of interest.
SOURCE: Thaiss CA et al. Science. 2018;359(6382):1376-83.
MIAMI – Hyperglycemia increases intestinal permeability, which facilitates enteric infections and systemic inflammation, reported Christoph Thaiss, PhD.
The findings upend the old idea that intestinal barrier dysfunction leads to diabetes, Dr. Thaiss said during a plenary session at the annual Gut Microbiota for Health World Summit. Multiple mouse models link hyperglycemia to intestinal barrier dysfunction, and hemoglobin A1C (HbA1c) levels in humans “highly correlate with the influx of microbial molecules into the intestinal epithelium.”
Researchers often struggle to decide if apparent causes are really confounders or even downstream results (reverse causation). In the metabolic syndrome, patients are known to have increased intestinal permeability – so-called leaky gut – and microbes crossing the gastrointestinal epithelium have been found to cause both gut mucosal infections and chronic systemic inflammation. But because these mechanisms were poorly understood, some experts posited that intestinal barrier dysfunction induced pancreatic beta cell inflammation, insulin resistance, and diabetes.
To take a deeper dive, Dr. Thaiss and his associates at the University of Pennsylvania, Philadelphia started with a mouse model of morbid obesity. The mice had multiple systemic sites with microbial pattern recognition ligands, signifying microbial influx from the gut. They also had genetic signatures indicating a marked disruption of junctions between epithelial cells, compared with healthy controls.
The obese mice also were much more susceptible to enteric infections with Citrobacter rodentium (a Salmonella analog), but obesity itself did not drive this risk, Dr. Thaiss explained. In fact, two different murine models of nonobese type 1 diabetes mellitus showed “leaky” intestinal epithelial adherence junctions, heightened susceptibility to C. rodentium infection, and showed systemic pathogen spread. Ribosomal DNA sequencing showed that these hyperglycemic (diabetic) mice had shifts in their gut microbiomes; however, translocating the altered microbiota to normal mice did not make them more susceptible to enteric infections or systemic inflammation.
Based on these findings, the researchers hypothesized that hyperglycemia itself drove susceptibility to enteric infections. They confirmed this by administering insulin to the mice with type 1 diabetes, which restored intestinal epithelial adherence junctions and stopped the systemic spread of pathogens. In vitro, exposing intestinal epithelial cells to glucose-induced barrier dysfunctions that increased over time and with higher glucose concentrations. RNA sequencing demonstrated that hyperglycemia markedly changed expression of genes that encode proteins that regulate intestinal barrier function. Moreover, hyperglycemic mice lacking the bidirectional glucose transporter GLUT2 showed no intestinal barrier dysfunction and were not susceptible to C. rodentium infection and systemic spread.
Finally, the investigators studied more than 30 clinical measures and microbial products in the systemic circulation of 27 healthy human volunteers. “Of all the variables we measured, HbA1c showed the strongest correlation with the influx of microbial molecules,” said Dr. Thaiss. Serum HbA1c correlated highly (P = .008) with levels of toll-like receptor 4, an indicator of systemic pathogens, but not with body mass index (P = .76).
The findings in humans confirm those in mice and indicate that hyperglycemia is a direct cause of intestinal barrier dysfunction and susceptibility to enteric infection, Dr. Thaiss said, adding that the systemic influx of microbial products might explain the wide range of otherwise unrelated inflammatory conditions seen in patients with metabolic syndrome. Future studies of therapies for enteric infection and systemic inflammation might focus on glucose as a modifier of intestinal barrier function.
These findings, reported at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, were also published in Science.
The work was supported by a Boehringer Ingelheim Funds PhD fellowship, the Leona M. and Harry B. Helmsley Charitable Trust, the Adelis Foundation, the Gurwin Family Fund for Scientific Research, the Crown Endowment Fund for Immunological Research, and others. Dr. Thaiss and his coinvestigators reported having no conflicts of interest.
SOURCE: Thaiss CA et al. Science. 2018;359(6382):1376-83.
MIAMI – Hyperglycemia increases intestinal permeability, which facilitates enteric infections and systemic inflammation, reported Christoph Thaiss, PhD.
The findings upend the old idea that intestinal barrier dysfunction leads to diabetes, Dr. Thaiss said during a plenary session at the annual Gut Microbiota for Health World Summit. Multiple mouse models link hyperglycemia to intestinal barrier dysfunction, and hemoglobin A1C (HbA1c) levels in humans “highly correlate with the influx of microbial molecules into the intestinal epithelium.”
Researchers often struggle to decide if apparent causes are really confounders or even downstream results (reverse causation). In the metabolic syndrome, patients are known to have increased intestinal permeability – so-called leaky gut – and microbes crossing the gastrointestinal epithelium have been found to cause both gut mucosal infections and chronic systemic inflammation. But because these mechanisms were poorly understood, some experts posited that intestinal barrier dysfunction induced pancreatic beta cell inflammation, insulin resistance, and diabetes.
To take a deeper dive, Dr. Thaiss and his associates at the University of Pennsylvania, Philadelphia started with a mouse model of morbid obesity. The mice had multiple systemic sites with microbial pattern recognition ligands, signifying microbial influx from the gut. They also had genetic signatures indicating a marked disruption of junctions between epithelial cells, compared with healthy controls.
The obese mice also were much more susceptible to enteric infections with Citrobacter rodentium (a Salmonella analog), but obesity itself did not drive this risk, Dr. Thaiss explained. In fact, two different murine models of nonobese type 1 diabetes mellitus showed “leaky” intestinal epithelial adherence junctions, heightened susceptibility to C. rodentium infection, and showed systemic pathogen spread. Ribosomal DNA sequencing showed that these hyperglycemic (diabetic) mice had shifts in their gut microbiomes; however, translocating the altered microbiota to normal mice did not make them more susceptible to enteric infections or systemic inflammation.
Based on these findings, the researchers hypothesized that hyperglycemia itself drove susceptibility to enteric infections. They confirmed this by administering insulin to the mice with type 1 diabetes, which restored intestinal epithelial adherence junctions and stopped the systemic spread of pathogens. In vitro, exposing intestinal epithelial cells to glucose-induced barrier dysfunctions that increased over time and with higher glucose concentrations. RNA sequencing demonstrated that hyperglycemia markedly changed expression of genes that encode proteins that regulate intestinal barrier function. Moreover, hyperglycemic mice lacking the bidirectional glucose transporter GLUT2 showed no intestinal barrier dysfunction and were not susceptible to C. rodentium infection and systemic spread.
Finally, the investigators studied more than 30 clinical measures and microbial products in the systemic circulation of 27 healthy human volunteers. “Of all the variables we measured, HbA1c showed the strongest correlation with the influx of microbial molecules,” said Dr. Thaiss. Serum HbA1c correlated highly (P = .008) with levels of toll-like receptor 4, an indicator of systemic pathogens, but not with body mass index (P = .76).
The findings in humans confirm those in mice and indicate that hyperglycemia is a direct cause of intestinal barrier dysfunction and susceptibility to enteric infection, Dr. Thaiss said, adding that the systemic influx of microbial products might explain the wide range of otherwise unrelated inflammatory conditions seen in patients with metabolic syndrome. Future studies of therapies for enteric infection and systemic inflammation might focus on glucose as a modifier of intestinal barrier function.
These findings, reported at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, were also published in Science.
The work was supported by a Boehringer Ingelheim Funds PhD fellowship, the Leona M. and Harry B. Helmsley Charitable Trust, the Adelis Foundation, the Gurwin Family Fund for Scientific Research, the Crown Endowment Fund for Immunological Research, and others. Dr. Thaiss and his coinvestigators reported having no conflicts of interest.
SOURCE: Thaiss CA et al. Science. 2018;359(6382):1376-83.
REPORTING FROM GMFH 2019
More fiber looks safe, might benefit ICU patients
MIAMI –
“Higher fiber intake was associated with greater preservation of short-chain fatty acid–producing bacteria, even after we adjusted for antibiotics and acute severity of illness,” said Yichun Fu, a fourth-year medical student at Columbia University, New York, at the annual Gut Microbiota for Health World Summit.
She explained that, after 72 hours on the high-fiber diet, only 11% of patients had abdominal distension noted in their EMRs, compared with 36% of patients who received no dietary fiber (P less than .01). Fiber was not associated with bowel obstruction, high gastric residuals, enteric infections, edema, or diarrhea. She and her associates presented the findings in a poster at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
Dietary fiber is a prebiotic that increases the abundance of short-chain fatty acid (SCFA)–producing bacteria in the gut. Growing evidence links these bacteria and their metabolites – such as acetate, propionate, and butyrate – to immunomodulatory benefits and suggests that they help maintain gut barrier function, glucose homeostasis, adipose tissue lipolysis, and normal blood pressure. Thus, fiber for ICU patients might make sense, but relevant dietary guidelines rarely address the topic. In practice, fiber is often withheld in the ICU because of concerns that it might cause bloating or diarrhea, Ms. Fu said.
For the study, the researchers performed 16s ribosomal RNA sequencing on baseline and 72-hour rectal swabs collected from 129 consecutive adults newly admitted to the ICU. Patients were eligible for the study regardless of whether they received nothing by mouth, enteral feeding, or food by mouth. They were grouped in tertiles based on fiber intake over 72 hours, corrected by caloric intake. The resulting groups were dubbed “no fiber” (median and interquartile range, 0 grams), “low fiber” (median, 11.2 g; IQR, 3.8-18.2 g), and “high fiber” (median, 39.3 g; IQR, 4.7-50.2 g).
Patients in these three groups had a similar relative abundance of SCFA-producing bacteria at baseline. At 72 hours, the high-fiber group had a significantly greater relative abundance of SCFA producers than the no fiber group (P = .01). Compared with no fiber, high-fiber intake also correlated with significantly increased gut bacterial diversity (P = .04) and a lower relative abundance of Enterococcus bacteria (P less than .01). None of these measures differed significantly between the no-fiber and low-fiber groups.
The groups were demographically and clinically similar at baseline, except that the high-fiber group had lower Acute Physiology and Chronic Health Evaluation IV scores (P = .02) and was less likely to receive antibiotics, mechanical ventilation, hemodialysis, or vasopressors (P less than .01). After correcting for these differences, each 10-g increase in fiber intake over 72 hours correlated with a 0.3% median increase in the relative abundance of SCFA-producing bacteria (estimated IQR, 0.10%-0.46%; P less than .01).
“Fiber may be a simple candidate therapy for ICU patients,” the researchers concluded. The team is now designing a prospective, interventional study to further test whether fiber can modify the gut microbiome to benefit ICU patients, Ms. Fu explained.
Funders included the American Gastroenterological Association, the National Institutes of Health, and the Feldstein Medical Foundation. Ms. Fu reported no competing interests.
MIAMI –
“Higher fiber intake was associated with greater preservation of short-chain fatty acid–producing bacteria, even after we adjusted for antibiotics and acute severity of illness,” said Yichun Fu, a fourth-year medical student at Columbia University, New York, at the annual Gut Microbiota for Health World Summit.
She explained that, after 72 hours on the high-fiber diet, only 11% of patients had abdominal distension noted in their EMRs, compared with 36% of patients who received no dietary fiber (P less than .01). Fiber was not associated with bowel obstruction, high gastric residuals, enteric infections, edema, or diarrhea. She and her associates presented the findings in a poster at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
Dietary fiber is a prebiotic that increases the abundance of short-chain fatty acid (SCFA)–producing bacteria in the gut. Growing evidence links these bacteria and their metabolites – such as acetate, propionate, and butyrate – to immunomodulatory benefits and suggests that they help maintain gut barrier function, glucose homeostasis, adipose tissue lipolysis, and normal blood pressure. Thus, fiber for ICU patients might make sense, but relevant dietary guidelines rarely address the topic. In practice, fiber is often withheld in the ICU because of concerns that it might cause bloating or diarrhea, Ms. Fu said.
For the study, the researchers performed 16s ribosomal RNA sequencing on baseline and 72-hour rectal swabs collected from 129 consecutive adults newly admitted to the ICU. Patients were eligible for the study regardless of whether they received nothing by mouth, enteral feeding, or food by mouth. They were grouped in tertiles based on fiber intake over 72 hours, corrected by caloric intake. The resulting groups were dubbed “no fiber” (median and interquartile range, 0 grams), “low fiber” (median, 11.2 g; IQR, 3.8-18.2 g), and “high fiber” (median, 39.3 g; IQR, 4.7-50.2 g).
Patients in these three groups had a similar relative abundance of SCFA-producing bacteria at baseline. At 72 hours, the high-fiber group had a significantly greater relative abundance of SCFA producers than the no fiber group (P = .01). Compared with no fiber, high-fiber intake also correlated with significantly increased gut bacterial diversity (P = .04) and a lower relative abundance of Enterococcus bacteria (P less than .01). None of these measures differed significantly between the no-fiber and low-fiber groups.
The groups were demographically and clinically similar at baseline, except that the high-fiber group had lower Acute Physiology and Chronic Health Evaluation IV scores (P = .02) and was less likely to receive antibiotics, mechanical ventilation, hemodialysis, or vasopressors (P less than .01). After correcting for these differences, each 10-g increase in fiber intake over 72 hours correlated with a 0.3% median increase in the relative abundance of SCFA-producing bacteria (estimated IQR, 0.10%-0.46%; P less than .01).
“Fiber may be a simple candidate therapy for ICU patients,” the researchers concluded. The team is now designing a prospective, interventional study to further test whether fiber can modify the gut microbiome to benefit ICU patients, Ms. Fu explained.
Funders included the American Gastroenterological Association, the National Institutes of Health, and the Feldstein Medical Foundation. Ms. Fu reported no competing interests.
MIAMI –
“Higher fiber intake was associated with greater preservation of short-chain fatty acid–producing bacteria, even after we adjusted for antibiotics and acute severity of illness,” said Yichun Fu, a fourth-year medical student at Columbia University, New York, at the annual Gut Microbiota for Health World Summit.
She explained that, after 72 hours on the high-fiber diet, only 11% of patients had abdominal distension noted in their EMRs, compared with 36% of patients who received no dietary fiber (P less than .01). Fiber was not associated with bowel obstruction, high gastric residuals, enteric infections, edema, or diarrhea. She and her associates presented the findings in a poster at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility.
Dietary fiber is a prebiotic that increases the abundance of short-chain fatty acid (SCFA)–producing bacteria in the gut. Growing evidence links these bacteria and their metabolites – such as acetate, propionate, and butyrate – to immunomodulatory benefits and suggests that they help maintain gut barrier function, glucose homeostasis, adipose tissue lipolysis, and normal blood pressure. Thus, fiber for ICU patients might make sense, but relevant dietary guidelines rarely address the topic. In practice, fiber is often withheld in the ICU because of concerns that it might cause bloating or diarrhea, Ms. Fu said.
For the study, the researchers performed 16s ribosomal RNA sequencing on baseline and 72-hour rectal swabs collected from 129 consecutive adults newly admitted to the ICU. Patients were eligible for the study regardless of whether they received nothing by mouth, enteral feeding, or food by mouth. They were grouped in tertiles based on fiber intake over 72 hours, corrected by caloric intake. The resulting groups were dubbed “no fiber” (median and interquartile range, 0 grams), “low fiber” (median, 11.2 g; IQR, 3.8-18.2 g), and “high fiber” (median, 39.3 g; IQR, 4.7-50.2 g).
Patients in these three groups had a similar relative abundance of SCFA-producing bacteria at baseline. At 72 hours, the high-fiber group had a significantly greater relative abundance of SCFA producers than the no fiber group (P = .01). Compared with no fiber, high-fiber intake also correlated with significantly increased gut bacterial diversity (P = .04) and a lower relative abundance of Enterococcus bacteria (P less than .01). None of these measures differed significantly between the no-fiber and low-fiber groups.
The groups were demographically and clinically similar at baseline, except that the high-fiber group had lower Acute Physiology and Chronic Health Evaluation IV scores (P = .02) and was less likely to receive antibiotics, mechanical ventilation, hemodialysis, or vasopressors (P less than .01). After correcting for these differences, each 10-g increase in fiber intake over 72 hours correlated with a 0.3% median increase in the relative abundance of SCFA-producing bacteria (estimated IQR, 0.10%-0.46%; P less than .01).
“Fiber may be a simple candidate therapy for ICU patients,” the researchers concluded. The team is now designing a prospective, interventional study to further test whether fiber can modify the gut microbiome to benefit ICU patients, Ms. Fu explained.
Funders included the American Gastroenterological Association, the National Institutes of Health, and the Feldstein Medical Foundation. Ms. Fu reported no competing interests.
REPORTING FROM GMFM 2019
Proinflammatory microbiome tied to colorectal adenoma
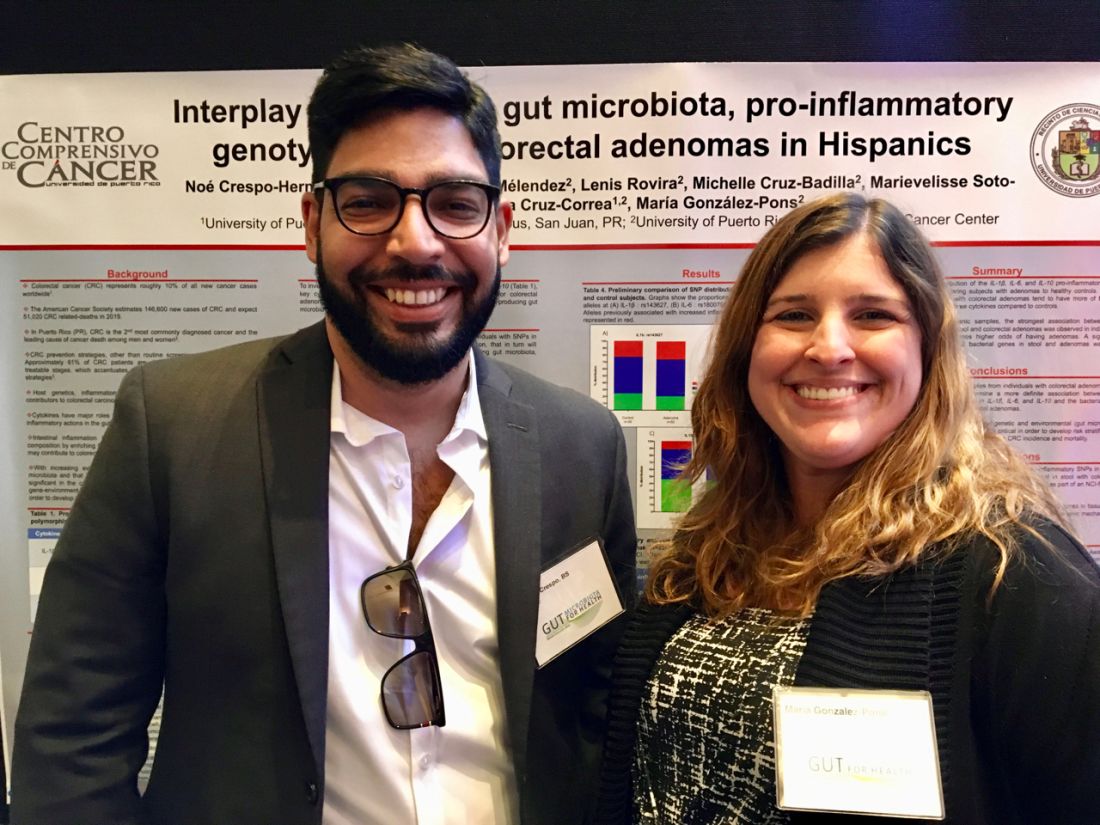
MIAMI – The fecal presence of least two genes harbored by toxin-producing or proinflammatory bacteria conferred a nearly 200% rise in the odds of colorectal adenoma, investigators reported.
Moreover, the fecal presence of usp (uropathogenic-specific protein), a bacterial gene encoding a genotoxin that damages DNA, correlated with nearly 1,200% greater odds of colorectal adenoma (P =.08), said senior investigator María González-Pons, PhD, of the University of Puerto Rico Comprehensive Cancer Center in San Juan.
“We are continuing to enlarge this study. We need more power to assess statistical significance and look at associations for individual combinations of bacterial genes,” Dr. Pons said in an interview. “Our ultimate goal is to risk-stratify patients so that we know whom to target for [colorectal cancer] prevention.”
Dr. Pons and the study’s lead author, Noe Crespo-Hernandez, of the University of Puerto Rico, presented the findings with their associates in a poster at the the annual Gut Microbiota for Health World Summit.
Colorectal cancer is the most lethal cancer and the second-most common malignancy in Puerto Rico. Despite recommendations for screening colonoscopy, many patients are diagnosed in late-stage disease, when treatment options are limited. Intestinal inflammation is itself key to colorectal carcinogenesis and also promotes the enteric proliferation of gram-negative bacteria that produce potentially carcinogenic toxins. Thus, gut inflammation and the microbiome are of great interest to researchers who are working to develop reliable, minimally invasive tests that assess future colorectal cancer risk.
For their study presented at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Pons and her coinvestigators compared stool samples from 67 adults with colonoscopically confirmed colorectal adenomas and 39 controls with negative screening colonoscopies. Both groups were captured in the Puerto Rico Familial Colorectal Cancer Registry. The researchers used TaqMan SNP Genotyping to look for single-nucleotide polymorphisms (SNPs) from promoter regions of genes encoding interleukin-1 beta, IL-6, and IL-10, cytokines that regulate gut inflammation. They found nonsignificant associations between colorectal adenoma and two of the three SNPs: rs143627 (encoding IL-1B) and rs1800795 (IL-6).
The real-time polymerase chain reaction results were even more striking. Using SYBR Green, the researchers tested stool for six genotoxic or proinflammatory bacterial genes and identified five, each of which correlated with colorectal adenoma. Colorectal adenoma also was linked with the fecal presence of a nonpathogenic housekeeping gene that is a surrogate for a mucolytic bacterium abundant in the stool of colorectal cancer patients.
Odds ratios for these associations ranged from 1.17 (for cnf, or cytotoxic necrotizing factor) to 12.83 (for usp), the researchers reported. Dr. Pons commented that Hurricane Maria greatly delayed this study and thus the cohort was underpowered to test for statistical significance. Nonetheless, P values approached significance for the usp gene (OR, 12.83; 95% confidence interval, 0.73-226.8; P = .08) and the fecal presence of at least two genes in combination (OR, 2.84; 95% CI, 1.01-8.90; P = .05).
Next, Dr. Pons and her team will expand the study to assess links between colorectal adenoma and these pathogenic bacterial genes, individually and in various combinations. They also plan to compare genes in normal and adenomatous colon tissue and to use enteroid (small intestinal organoid) models to tease out the carcinogenic mechanisms of these bacterial toxins.
The National Institutes of Health provided funding. The researchers disclosed no competing interests.
MIAMI – The fecal presence of least two genes harbored by toxin-producing or proinflammatory bacteria conferred a nearly 200% rise in the odds of colorectal adenoma, investigators reported.
Moreover, the fecal presence of usp (uropathogenic-specific protein), a bacterial gene encoding a genotoxin that damages DNA, correlated with nearly 1,200% greater odds of colorectal adenoma (P =.08), said senior investigator María González-Pons, PhD, of the University of Puerto Rico Comprehensive Cancer Center in San Juan.
“We are continuing to enlarge this study. We need more power to assess statistical significance and look at associations for individual combinations of bacterial genes,” Dr. Pons said in an interview. “Our ultimate goal is to risk-stratify patients so that we know whom to target for [colorectal cancer] prevention.”
Dr. Pons and the study’s lead author, Noe Crespo-Hernandez, of the University of Puerto Rico, presented the findings with their associates in a poster at the the annual Gut Microbiota for Health World Summit.
Colorectal cancer is the most lethal cancer and the second-most common malignancy in Puerto Rico. Despite recommendations for screening colonoscopy, many patients are diagnosed in late-stage disease, when treatment options are limited. Intestinal inflammation is itself key to colorectal carcinogenesis and also promotes the enteric proliferation of gram-negative bacteria that produce potentially carcinogenic toxins. Thus, gut inflammation and the microbiome are of great interest to researchers who are working to develop reliable, minimally invasive tests that assess future colorectal cancer risk.
For their study presented at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Pons and her coinvestigators compared stool samples from 67 adults with colonoscopically confirmed colorectal adenomas and 39 controls with negative screening colonoscopies. Both groups were captured in the Puerto Rico Familial Colorectal Cancer Registry. The researchers used TaqMan SNP Genotyping to look for single-nucleotide polymorphisms (SNPs) from promoter regions of genes encoding interleukin-1 beta, IL-6, and IL-10, cytokines that regulate gut inflammation. They found nonsignificant associations between colorectal adenoma and two of the three SNPs: rs143627 (encoding IL-1B) and rs1800795 (IL-6).
The real-time polymerase chain reaction results were even more striking. Using SYBR Green, the researchers tested stool for six genotoxic or proinflammatory bacterial genes and identified five, each of which correlated with colorectal adenoma. Colorectal adenoma also was linked with the fecal presence of a nonpathogenic housekeeping gene that is a surrogate for a mucolytic bacterium abundant in the stool of colorectal cancer patients.
Odds ratios for these associations ranged from 1.17 (for cnf, or cytotoxic necrotizing factor) to 12.83 (for usp), the researchers reported. Dr. Pons commented that Hurricane Maria greatly delayed this study and thus the cohort was underpowered to test for statistical significance. Nonetheless, P values approached significance for the usp gene (OR, 12.83; 95% confidence interval, 0.73-226.8; P = .08) and the fecal presence of at least two genes in combination (OR, 2.84; 95% CI, 1.01-8.90; P = .05).
Next, Dr. Pons and her team will expand the study to assess links between colorectal adenoma and these pathogenic bacterial genes, individually and in various combinations. They also plan to compare genes in normal and adenomatous colon tissue and to use enteroid (small intestinal organoid) models to tease out the carcinogenic mechanisms of these bacterial toxins.
The National Institutes of Health provided funding. The researchers disclosed no competing interests.
MIAMI – The fecal presence of least two genes harbored by toxin-producing or proinflammatory bacteria conferred a nearly 200% rise in the odds of colorectal adenoma, investigators reported.
Moreover, the fecal presence of usp (uropathogenic-specific protein), a bacterial gene encoding a genotoxin that damages DNA, correlated with nearly 1,200% greater odds of colorectal adenoma (P =.08), said senior investigator María González-Pons, PhD, of the University of Puerto Rico Comprehensive Cancer Center in San Juan.
“We are continuing to enlarge this study. We need more power to assess statistical significance and look at associations for individual combinations of bacterial genes,” Dr. Pons said in an interview. “Our ultimate goal is to risk-stratify patients so that we know whom to target for [colorectal cancer] prevention.”
Dr. Pons and the study’s lead author, Noe Crespo-Hernandez, of the University of Puerto Rico, presented the findings with their associates in a poster at the the annual Gut Microbiota for Health World Summit.
Colorectal cancer is the most lethal cancer and the second-most common malignancy in Puerto Rico. Despite recommendations for screening colonoscopy, many patients are diagnosed in late-stage disease, when treatment options are limited. Intestinal inflammation is itself key to colorectal carcinogenesis and also promotes the enteric proliferation of gram-negative bacteria that produce potentially carcinogenic toxins. Thus, gut inflammation and the microbiome are of great interest to researchers who are working to develop reliable, minimally invasive tests that assess future colorectal cancer risk.
For their study presented at the meeting sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Pons and her coinvestigators compared stool samples from 67 adults with colonoscopically confirmed colorectal adenomas and 39 controls with negative screening colonoscopies. Both groups were captured in the Puerto Rico Familial Colorectal Cancer Registry. The researchers used TaqMan SNP Genotyping to look for single-nucleotide polymorphisms (SNPs) from promoter regions of genes encoding interleukin-1 beta, IL-6, and IL-10, cytokines that regulate gut inflammation. They found nonsignificant associations between colorectal adenoma and two of the three SNPs: rs143627 (encoding IL-1B) and rs1800795 (IL-6).
The real-time polymerase chain reaction results were even more striking. Using SYBR Green, the researchers tested stool for six genotoxic or proinflammatory bacterial genes and identified five, each of which correlated with colorectal adenoma. Colorectal adenoma also was linked with the fecal presence of a nonpathogenic housekeeping gene that is a surrogate for a mucolytic bacterium abundant in the stool of colorectal cancer patients.
Odds ratios for these associations ranged from 1.17 (for cnf, or cytotoxic necrotizing factor) to 12.83 (for usp), the researchers reported. Dr. Pons commented that Hurricane Maria greatly delayed this study and thus the cohort was underpowered to test for statistical significance. Nonetheless, P values approached significance for the usp gene (OR, 12.83; 95% confidence interval, 0.73-226.8; P = .08) and the fecal presence of at least two genes in combination (OR, 2.84; 95% CI, 1.01-8.90; P = .05).
Next, Dr. Pons and her team will expand the study to assess links between colorectal adenoma and these pathogenic bacterial genes, individually and in various combinations. They also plan to compare genes in normal and adenomatous colon tissue and to use enteroid (small intestinal organoid) models to tease out the carcinogenic mechanisms of these bacterial toxins.
The National Institutes of Health provided funding. The researchers disclosed no competing interests.
REPORTING FROM GUT 2019