FORT LAUDERDALE, FLA. – An evaluation of 222 pain-related smartphone apps showed that many were developed without the input of a health professional, some had inaccurate information, and some of their features weren’t as robust as they could be.
"Many of them were giving advice and offering coping strategies, but we don’t know if they’re effective," said Lorraine S. Wallace, Ph.D., who led the study. In addition, the apps could potentially be dangerous for users if the coping strategy – for instance, exercise – isn’t right for them, she said.
Experts have begun studying the safety and efficacy of health-related smartphone apps, many of which are aimed at patients for managing various diseases and conditions.
Dr. Wallace said that, ideally, app developers, physicians, and patients should collaborate to create the apps. "And there needs to be a list of good apps. I always get asked ‘show us a good app,’ so there are definitely some features that we should look at, and that should be driven by health care professionals to determine what a pain app should look like," she said. She advised physicians to be aware of the apps that are currently available to patients.
Dr. Wallace said her study was modeled after a 2011 British study of 111 pain-related apps. The authors of that study also concluded, "Pain apps appear to be able to promise pain relief without any concern for the effectiveness of the product, or for possible adverse effects of product use. In a population often desperate for a solution to distressing and debilitating pain conditions, there is considerable risk of individuals being misled" (J. Telemed. Telecare. 2011;17:308-12).
Dr. Wallace of the department of family medicine and director of research at the Ohio State University in Columbus said that in her evaluation, she didn’t find an ideal pain-related app. "There were certain ones that had better features such as pain diaries or other characteristics, but most of them were not that comprehensive."
Dr. Wallace and her colleagues searched Apple, Android, and Blackberry app stores for the word "pain." They chose 222 apps, and evaluated certain information such as cost, purpose, and key features and documentation of medical professional involvement in design and/or content.
The apps were released between June 2009 and July 2012, with an average cost of $4.99 or less (only seven apps cost more than $9.99). Researchers didn’t purchase any of the apps.
Pain diaries, exercises, and coping strategies were the most common app features. Many apps focused on general pain (93), 57 addressed back and/or neck pain, and 21 dealt with migraine/headache pain. Researchers found one app for muscle pain and one for pain from each of the following conditions: fibromyalgia, menstruation, injury, patellar tendonitis, rheumatism, and sciatica.
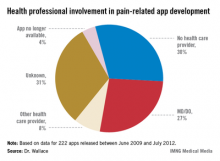
But, "the key finding was that in 30% of the apps, there was no evidence of a health provider input," said Dr. Wallace, who presented her findings in a poster at the annual meeting of the American Academy of Pain Medicine. In another 30%, the developer was unknown, and researchers couldn’t determine whether a health provider was involved in developing the app. In only 27% of the apps was there a clear involvement of an MD or DO.
Dr. Wallace and her team are working to get the study published and are planning to do a more extensive review of the apps this year. "We’re also planning on connecting some of the studies and looking at what percentages of physicians are recommending these apps and under what circumstances."
Dr. Wallace said she had no relevant financial disclosures.
On Twitter @NaseemSMiller