While single-center studies have supported the advantages of multiple arterial grafts over venous grafts in coronary artery bypass surgery, an analysis of patients in the international and multicenter SYNTAX trial has shown that, on propensity matching, rates of cardiac events and death are actually similar between the two groups.
These findings of the SYNTAX investigators, led by Dr. Catalina Parasca of Erasmus University in Rotterdam, the Netherlands, were published online in the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j.jtcvs.2015.05.010).
The SYNTAX trial compared percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) in patients with left main or three-vessel coronary artery disease (Lancet. 2013;381[9867]:629-38).
In the latest report, the SYNTAX investigators found that patients in unmatched groups who received arterial grafts in addition to an arterial graft of the left anterior descending artery (LAD) had noticeably lower rates of death and a composite endpoint of death-stroke-MI than did those who received a second venous graft. However, when the researchers applied propensity matching, the outcomes between the two groups were similar.
 Coutresy of JTCVS/American Association for Thoracic Surgery
Coutresy of JTCVS/American Association for Thoracic Surgery
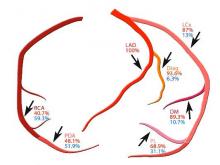
Percentage arterial (red), venous (blue) grafts shown in relation to distal anastomoses; LAD, left anterior descending; Diag, diagonal; LCx, left circumflex; OM, obtuse marginal; PL, postero-lateral; RCA, right coronary; PDA, Posterior descending artery.
Because large randomized trials have yet to prove the superiority of multiarterial grafts, the adoption rate has been low, Dr. Parasca and colleagues said. “The objective of this study was to assess the effect of using a second arterial graft on 5-year outcomes in patients who underwent CABG in the SYNTAX trial and registry,” they said.
They looked at 1,322 SYNTAX trial patients who had CABG with 5-year follow-up. In unmatched groups, the safety endpoint of the death-stroke-MI composite was 13.3% in the multiarterial group vs. 18.7% in the vein graft group. Although the incidence of stroke, MI, and graft occlusion was similar between the unmatched groups, the second-graft arterial group had a higher revascularization rate at 5 years, 12.6% vs. 9.6%, mainly due to repeat PCI. The element of the composite where the two unmatched groups deviated was the all-cause death rate at 5 years: 8.9% in the second-graft arterial group and 13.1% in the venous group.
However, when the investigators applied propensity matching, the differences between the two groups were insignificant.
“The results of the present study must be seen in the light of a multicenter CABG cohort with complex coronary disease, where revascularization was performed according to surgeon’s personal experience and local practices,” Dr. Parasca and coauthors noted. “The result was a high heterogeneity of CABG techniques, which shows different understanding of the best ‘graft-target match’ across centers.”
While the SYNTAX analysis demonstrates the variation in patient selection and operator technique with regard to arterial revascularization typical of a multicenter study, “extended follow-up beyond 5 years is required to estimate its impact on long-term outcomes,” Dr. Parasca and colleagues said.
Boston Scientific supported the trial. Coauthor Keith Dawkins is employed by Boston Scientific and coauthor Ted Feldman has received consulting fees from the company. The other authors reported no disclosures.

