SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
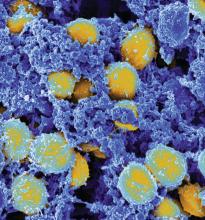
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.