News from the FDA/CDC
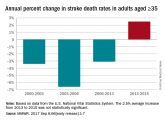
Recent upturn seen in stroke death rate
Long-term decline ended in 2013; reasons for the reversal “are not clear.”

AT ANA 2017
SAN DIEGO – Young adults who have suffered a stroke are at greater risk of a second stroke than other cardiovascular events, at least in the first year. That’s the conclusion drawn from a new analysis of 2013 data drawn from the Nationwide Readmissions Database.
The results suggest that younger adults who have a first-time stroke have a different risk profile than older adults and could require different management to improve long-term outcomes. The incidence of stroke has increased in recent years to the point that this population now accounts for about 10% of all strokes.
The analysis looked at all admissions for ischemic stroke in patients aged 18-45. The researchers found a cumulative risk of rehospitalization of 5.5% at 300 days, compared with 3.6% for cardiovascular disease.
When the researchers looked at risk factors, they discovered that blood sugar and dyslipidemia were tied to heightened risk, but there was no link to hypertension. “It was surprising. If you look at the older adult literature, there is a strong association between hypertension and these events,” said Peter Jin, MD, in an interview.The study can’t explain the association, nor can it prove causation. “Our thought was that the effects of hypertension might take longer to manifest in terms of cardiovascular outcomes as compared to hypercholesterolemia and diabetes,” said Dr. Jin, who is chief resident in the department of neurology at Icahn School of Medicine at Mount Sinai, New York. He presented the research at the annual meeting of the American Neurological Association.
The result sends a clear message for physicians caring for young adults who have experienced a first-time stroke. “They should be rigorously worked up and managed for any disorders in blood sugar and lipid disorders,” Dr. Jin said. Their care is vital because these younger adults have more time to accumulate second, third, or fourth strokes that could dramatically increase the burden of disease. “It’s just a matter of time. Optimizing their secondary prevention is crucial,” Dr. Jin said.
The study included data from 12,392 young adults in the Nationwide Readmissions Database who had suffered a first-time stroke. The researchers identified a higher readmission rate for stroke than cardiovascular events at 90 days (2,913.3 vs. 1,132.4 per 100,000 index hospitalizations). This pattern held when the analysis was restricted to patients who had no cardiovascular risk factors prior to the index hospitalization (2,534.9 vs. 676 per 100,000 index hospitalizations).
At 100 days, the cumulative risks were 3.2% for stroke and 2.5% for cardiovascular events. The risks were 4.3% and 3.2% at 200 days, and 5.5% and 3.6% at 300 days.
A multivariate analysis showed that patients with baseline diabetes were at a heightened risk of cardiovascular events (hazard ratio, 1.49; 95% confidence interval, 1.17-1.88), as were patients with hypercholesterolemia (HR, 1.43; 95% CI, 1.15-1.79) and those with atrial fibrillation or flutter (HR, 3.86; 95% CI, 2.74-5.43). Only diabetes was significantly associated with increased risk for hospitalization for recurrent stroke (HR, 1.5; 95% CI, 1.22-1.84).
Dr. Jin is eager to see if future research might establish a causative link between these risk factors and outcomes. The current work grew out of an administrative data set, but registry data or a prospective study could be more robust.
The study received no external funding. Dr. Jin reported having no financial disclosures.
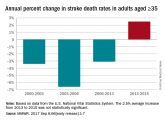
Long-term decline ended in 2013; reasons for the reversal “are not clear.”

Nearly 20% of patients 3-6 months after a stroke, in a Taiwanese database, were not using statins. Read the findings of a large retrospective...
