Acne fulminans is an uncommon and debilitating disease that presents as an acute eruption of nodular and ulcerative acne lesions with associated systemic symptoms.1,2 Although its underlying pathophysiology is not well understood, it occurs commonly during treatment of severe acne (eg, acne conglobata) with isotretinoin in young adolescent males.3 Zaba et al4 indicated that an underlying genetic disorder, increase in serum androgen levels, or presence of autoimmune disorders may contribute to the development of acne fulminans.
Isotretinoin and doxycycline also can potentially induce development of neutrophilic dermatoses including Sweet syndrome and pyoderma gangrenosum in patients with severe acne lesions, which can be clinically similar to an acne fulminans eruption. The neutrophilic dermatosis is characterized by the acute appearance of painful ulcerative papulonodules accompanied by systemic symptoms including fever and leukocytosis.
Case Report
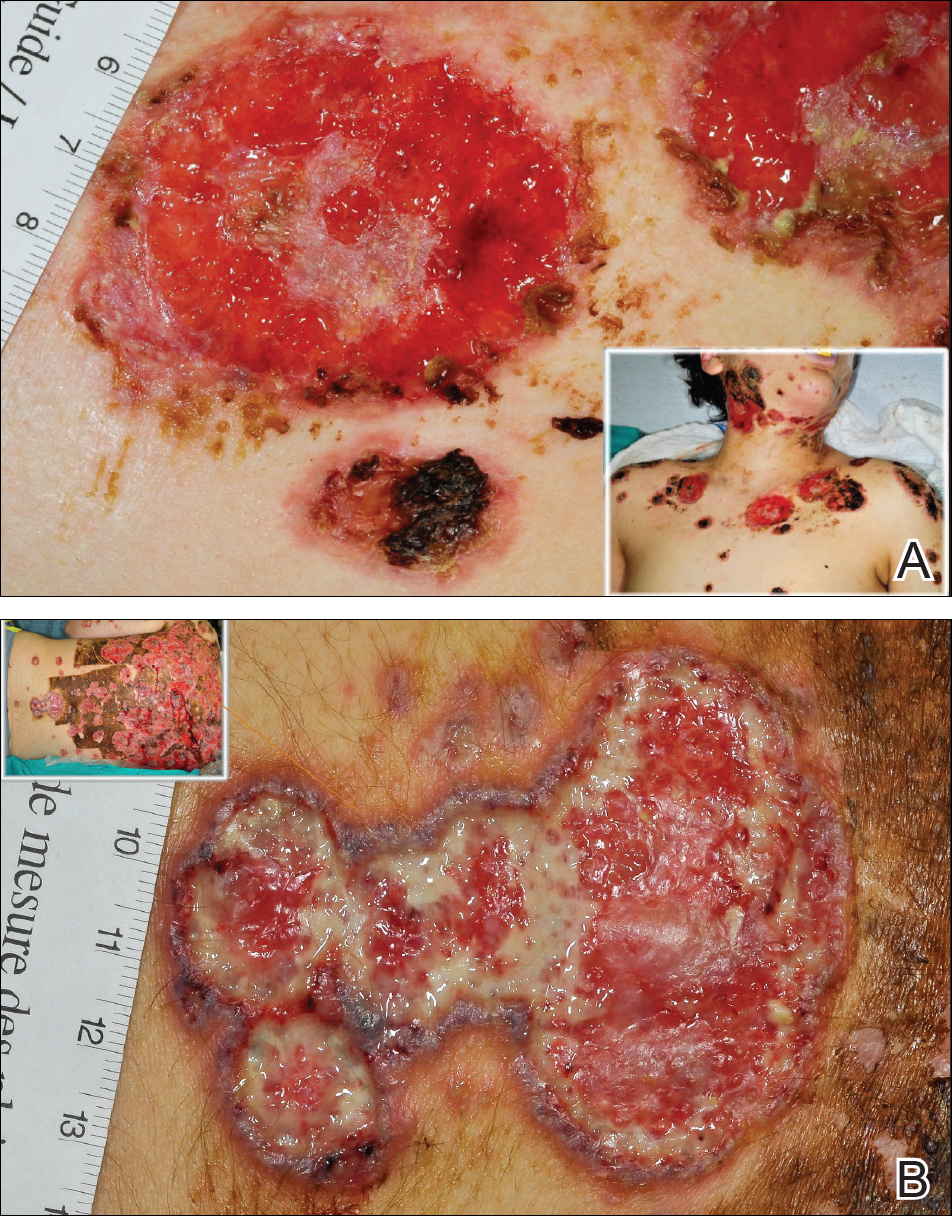
A 13-year-old adolescent boy was initially assessed by his family physician 2 months prior and started on oral doxycycline 100 mg twice daily for acne conglobata on the back. Unfortunately, the acne lesions, especially those on the upper back (Figure 1), started getting worse after 1 month of treatment with doxycycline; thus, he subsequently was switched to oral isotretinoin 0.5 mg/kg once daily. Less than 2 weeks later, the acne lesions worsened, and the patient also developed severe generalized arthralgia, myalgia, and fever (>38.3°C). He acutely developed hundreds of ulcerative plaques covering the entire trunk, upper extremities, face, and neck.
He was admitted to the Stollery Children’s Hospital (Edmonton, Alberta, Canada) and was assessed by the dermatology, rheumatology, and general pediatric teams (Figure 2). He initially was investigated for the potential presence of autoinflammatory disorders, such as PAPA syndrome (pyogenic arthritis, pyoderma gangrenosum, acne) and SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, osteitis). A laboratory workup showed an elevated erythrocyte sedimentation rate (43 mm/h [reference range, <20 mm/h]) and C-reactive protein level (50 mg/L [reference range, <10 mg/L]), leukocytosis (14×109/L [reference range, 4.5–11.0×109/L]), and transaminitis (alanine aminotransferase, 72 U/L [reference range, 10–40 U/L]). A radiograph of the clavicle did not reveal any osteitis. Rheumatology assessment ruled out the presence of any synovitis. Based on the patient’s history and physical presentation, a differential diagnosis of acne fulminans, pyoderma gangrenosum, and Sweet syndrome was entertained. Histologic findings were consistent with a diagnosis of ulcerative neutrophilic dermatosis. The patient required prolonged hospitalization (>3 months) for treatment, dressing changes, and pain control.
 Photography courtesy of the Strollery Children's Hospital (Edmonton, Alberta, Canada) professional photography team.
Photography courtesy of the Strollery Children's Hospital (Edmonton, Alberta, Canada) professional photography team.
Figure 2. Clinical presentation at the time of admission to the hospital. Diffuse, well-demarcated, discrete and confluent ulcers with violaceous overhanging borders were mostly consistent with pyoderma gangrenosum (A). Well-demarcated, discrete, annular, edematous, pseudovesicular papules with hemorrhagic crust in the center which were consistent with Sweet syndrome (B).
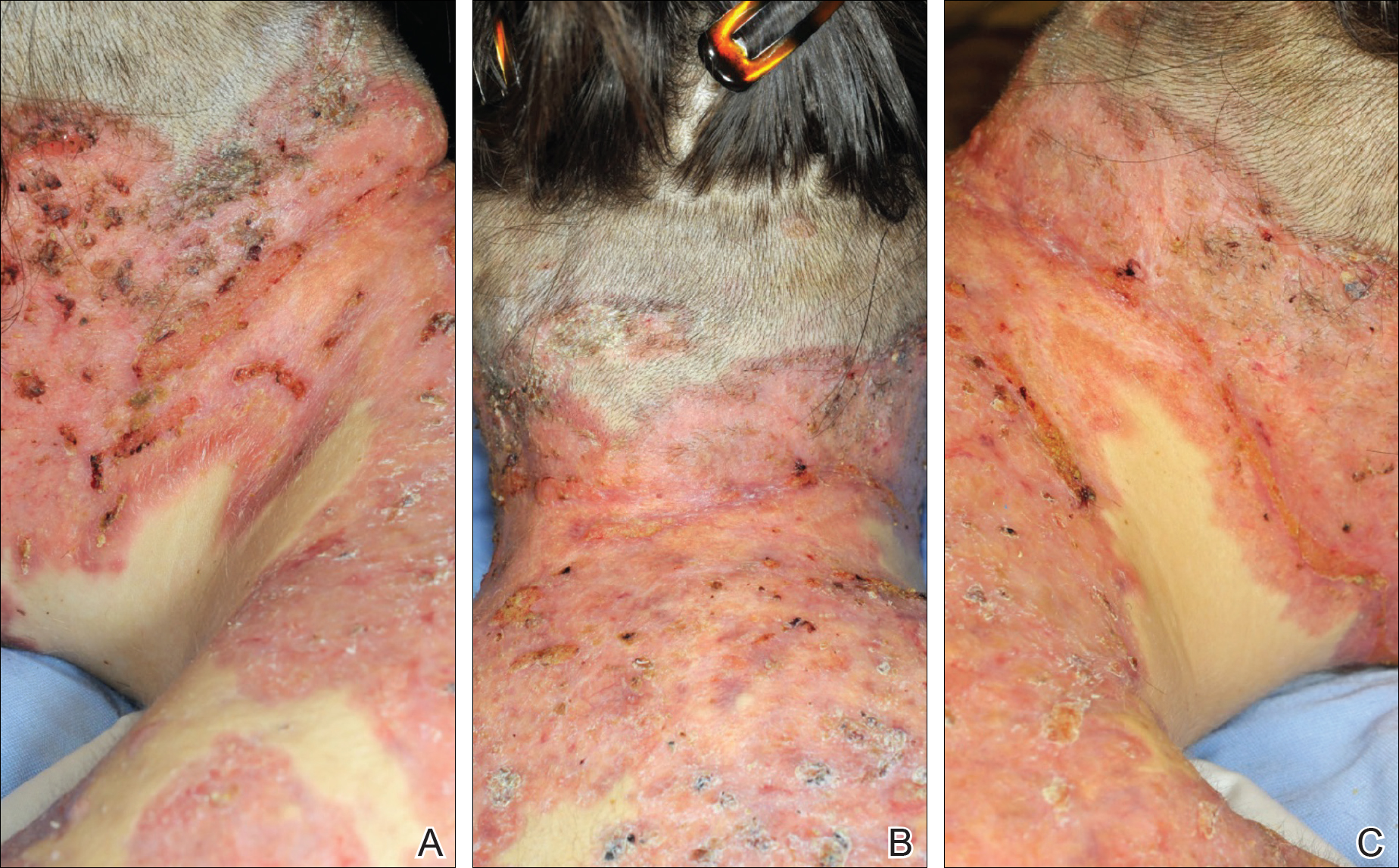
The patient initially was treated with prednisone 30 mg once daily for 3 weeks; dapsone 50 mg once daily and colchicine 0.6 mg twice daily were added while attempting to slowly wean off the prednisone (starting at 30 mg daily and reducing by 5 mg every other week). An attempt to discontinue the prednisone after 2 months was followed by immediate recurrence of the lesions (Figure 3), and the prednisone was restarted for another month. He was subsequently switched to oral cyclosporine 5 mg/kg once daily and achieved considerable improvement in his skin condition (Figure 4).
 Photography courtesy of the Strollery Children's Hospital (Edmonton, Alberta, Canada) professional photography team.
Photography courtesy of the Strollery Children's Hospital (Edmonton, Alberta, Canada) professional photography team.
Figure 3. The lesions flared up after attempting to wean off prednisone for the first time. The presence of well-demarcated superficial ulcers that were morphologically consistent with worsening pyoderma gangrenosum were noted (A and B).
 Photography courtesy of the Strollery Children's Hospital (Edmonton, Alberta, Canada) professional photography team.
Photography courtesy of the Strollery Children's Hospital (Edmonton, Alberta, Canada) professional photography team.
Figure 4. Notable improvement of the lesions was appreciated during cyclosporine treatment (A–C). The presence of considerable cushingoid changes was noted due to months of prednisone use.


