JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
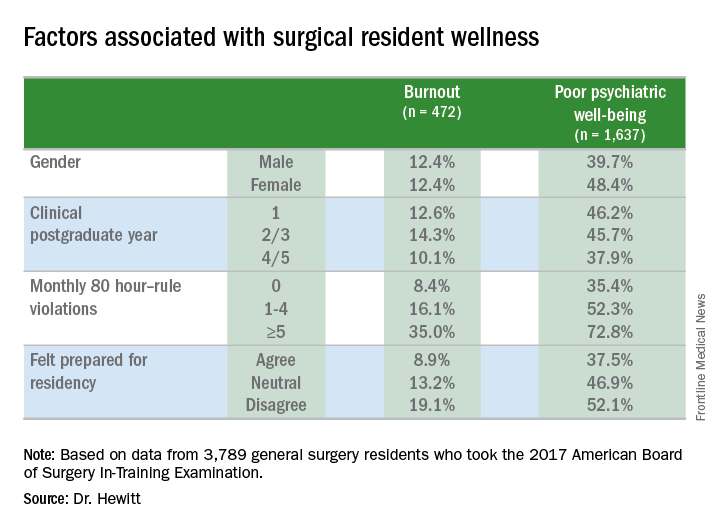
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
Likewise, rates of poor psychiatric well-being worsened with more duty-hour violations: 35.4% for those with no monthly violations, 52.3% for those with one to four a month, and 72.8% for those with five or more a month, Dr. Hewitt said.Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01