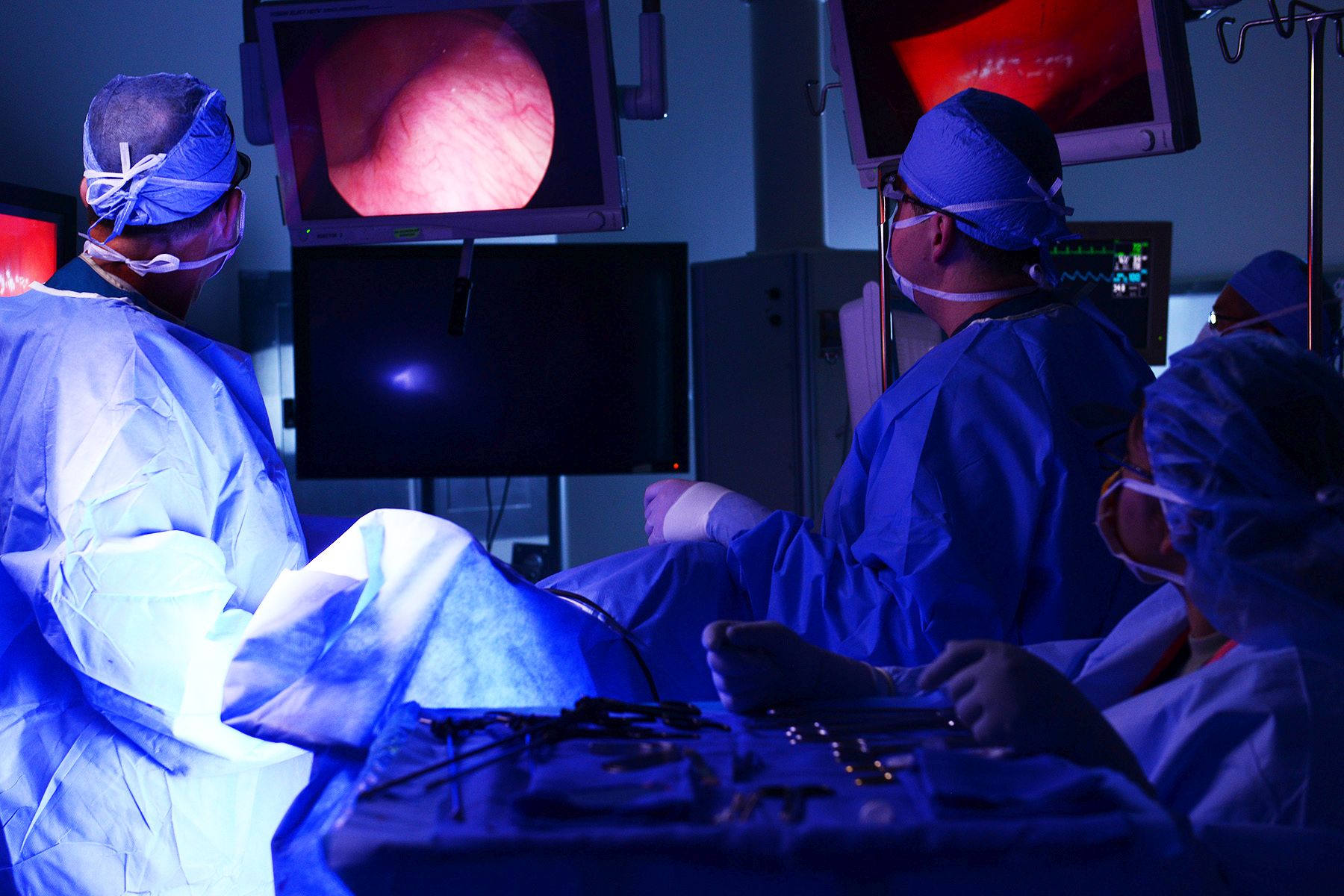
based on findings from the randomized, controlled phase 3 Laparoscopic Approach to Cervical Cancer (LACC) trial of more than 600 women.
The alarming findings, which led to early study termination, also were supported by results from a second population-based study. Both studies were published concurrently in the Oct. 31 issue of the New England Journal of Medicine.
The disease-free survival at 4.5 years among 319 patients who underwent minimally invasive surgery in the LACC trial was 86.0% vs. 96.5% in 312 patients who underwent open surgery, Pedro T. Ramirez, MD, of the University of Texas MD Anderson Cancer Center, Houston, and his colleagues reported (N Engl J Med. 2018 Oct 31. doi: 10.1056/NEJMoa1806395).
At 3 years, the disease-free survival rates were 91.2% in the minimally invasive surgery group and 97.1% in open surgery group (hazard ratio for disease recurrence or death from cervical cancer, 3.74).
The differences between the groups persisted after adjustment for age, body mass index, disease stage, lymphovascular invasion, and lymph-node involvement. In the minimally invasive surgery group, the findings were comparable for those who underwent laparoscopic vs. robot-assisted surgery, the investigators found.
Further, at 3 years, overall survival was 93.8% vs. 99.0% (HR for death from any cause, 6.00), death from cervical cancer was 4.4% vs. 0.6% (HR, 6.56), and the rate of locoregional recurrence-free survival was 94.3 vs. 98.3 (HR, 4.26) in the minimally invasive and open surgery groups, respectively.
Study participants were women with a mean age of 46 years with stage IA1, IA2, or IB1 cervical cancer, with most (91.9%) having IB1 disease, and either squamous-cell carcinoma, adenocarcinoma, or adenosquamous carcinoma. They were recruited from 33 centers worldwide between June 2008 and June 2017. Most of those assigned to minimally invasive surgery underwent laparoscopic surgery (84.4%), and the remaining patients underwent robot-assisted surgery.
The treatment groups were balanced with respect to baseline characteristics, they noted.
The minimally invasive approach is widely used given that guidelines from the National Comprehensive Cancer Network and European Society of Gynecological Oncology consider both surgical approaches acceptable, and since retrospective studies suggest laparoscopic radical hysterectomy is associated with lower complication rates and comparable outcomes. However, there are limited prospective data regarding survival outcomes in early stage disease with the two approaches, the researchers said.
“Our results call into question the findings in the literature suggesting that minimally invasive radical hysterectomy is associated with no difference in oncologic outcomes as compared with the open approach,” they wrote, noting that a number of factors may explain the differences, such as concurrent vs. sequential analyses in the current studies vs. prior studies (in sequential analyses, earlier procedures may have been performed under broader indications and less clearly defined radiotherapy guidelines), and the possibility that “routine use of a uterine manipulator might increase the propensity for tumor spillage” in minimally invasive surgery.
Strengths of the study include its prospective, randomized, international multicenter design and inclusion of a per-protocol analysis that was consistent with the intention-to-treat analysis, and limitations include the fact that intended enrollment wasn’t reached because of the “safety alert raised by the data and safety monitoring committee on the basis of the higher recurrence and death in the minimally invasive surgery groups,” as well as the inability to generalize the results to patients with low-risk disease as there was lack of power to evaluate outcomes in that context.