Extended follow-up of the RESONATE-2 trial showed that first-line ibrutinib sustained efficacy in elderly patients with chronic lymphocytic leukemia (CLL).
Patients who received ibrutinib had a long-term progression-free survival benefit over those who received chlorambucil.
The depth of response to ibrutinib improved over time, which meant there was a substantial increase in the proportion of patients achieving complete response.
Additionally, rates of some serious adverse events associated with ibrutinib decreased over time.
Paul M. Barr, MD, of the University of Rochester in New York, and his colleagues reported these findings in Haematologica.
Previously reported results of the RESONATE-2 trial, which showed an 84% reduction in the risk of death for ibrutinib versus chlorambucil, led to the approval of ibrutinib for first-line CLL treatment, the authors said.
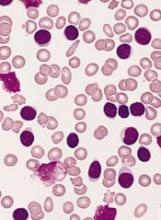
The study included 269 patients with untreated CLL or small lymphocytic lymphoma who had active disease and were at least 65 years of age. They were randomized to receive ibrutinib (n=136) or chlorambucil (n=133).
At a median follow-up of 29 months, 79% (107/136) of patients remained on ibrutinib.
There was an 88% reduction in the risk of progression or death for patients randomized to ibrutinib (P<0.0001).
The rate of complete response improved over time in ibrutinib-treated patients, from 7% at 12 months to 15% at 24 months and 18% at 36 months (maximum follow-up).
The overall response rate (ORR) with ibrutinib was 92%, with comparable findings in high-risk subgroups. The ORR was 100% in patients with del(11q) and 95% in those with unmutated IGHV.
Lymphadenopathy improved in most ibrutinib-treated patients, with complete resolution in 42%, compared to 7% of patients who received chlorambucil.
Splenomegaly improved by at least 50% in 95% of ibrutinib-treated patients and 52% in chlorambucil recipients, with complete resolution in 56% and 22%, respectively.
Adverse events of grade 3 or greater were generally seen more often in the first year of ibrutinib therapy and decreased over time.
The rate of grade 3 or higher neutropenia decreased from 8.1% in the first 12 months of treatment to 0% in the third year. The rate of grade 3 or higher anemia decreased from 5.9% to 1%. And the rate of grade 3 or higher thrombocytopenia decreased from 2.2% to 0%.
The rate of atrial fibrillation increased from 6% in the primary analysis to 10% in extended follow-up. However, investigators said ibrutinib dose reductions and discontinuations because of this adverse event were uncommon and less frequent with extended treatment.
“Atrial fibrillation therefore appears manageable and does not frequently necessitate ibrutinib discontinuation,” they concluded.
This study was supported by Pharmacyclics, an AbbVie company, and by grants from the National Institutes of Health and the MD Anderson Moon Shot Program in CLL. Pharmacyclics designed the study and performed analysis of the data. Several study authors reported funding from various companies, including Pharmacyclics.