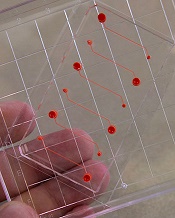
Photo courtesy of the
Wyss Institute at Harvard
A novel microfluidic device can be used to monitor thrombus formation and platelet function in patients receiving antiplatelet therapy, according to research published in Biomedical Microdevices.
The device is designed to mimic cellular and vascular flow conditions inside the human body.
Investigators say it demonstrates how endothelial cells contribute to hemostasis, even though it does not contain living endothelial cells.
The device contains microfluidic channels lined with chemically fixed human endothelial cells.
“It’s a bioinspired device that contains the endothelial function of a diseased patient without having actual living cells, and this greatly increases the robustness of the device,” explained study author Abhishek Jain, PhD, of Texas A&M University in College Station, Texas.
D Jain and his colleagues said their device retains the ability to modulate hemostasis under continuous flow in vitro, even after a few days of storage.
And the team successfully used the device to measure thrombus formation and platelet function in small amounts of whole blood from patients receiving antiplatelet therapy.
“Abnormal blood coagulation and platelet activation are major medical problems, and the ways we study them now are overly simplified,” said study author Donald Ingber, MD, PhD, of the Wyss Institute for Biologically Inspired Engineering at Harvard University in Boston, Massachusetts.
“Clinicians currently do not have tools to monitor hemostasis that take into account physiologically important interactions between endothelial cells and flowing blood.”
In a previous study, Dr Ingber and his colleagues showed that recreating the physicality and blood flow of vasculature within microfluidic channels allowed them to predict precise times that blood might clot, with potential applications in real-time monitoring of patients receiving anticoagulants.
The group’s new device adds another layer of complexity by embedding the functionality of the vascular endothelium within a tool that might be manufactured, stored, and shipped for clinical use.
“This is one of the first examples of how a microfluidic cell culture system could have added value in clinical diagnostics,” said study author Andries van der Meer, PhD, of University of Twente in Enschede, Netherlands.
“Using chemically fixed tissue that is no longer alive offers a clear, low-risk path toward further testing and product development.”


