In a phase 2 trial, an investigational drug conferred a significant improvement in survival when used as salvage therapy in poor-risk patients with acute myeloid leukemia (AML).
On the other hand, the drug did not provide any significant improvements over control treatment (investigator’s choice) in the entire population of AML patients in first relapse.
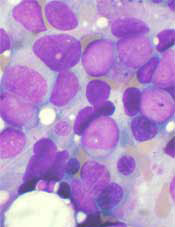
The drug, CPX-351, is a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle.
Researchers reported these results with CPX-351 in Cancer. The study was funded by Celator Pharmaceuticals, the company developing CPX-351, and the Leukemia and Lymphoma Society.
“Patients with first-relapse AML have generally a poor prognosis, with a limited likelihood of response following salvage treatment,” said study author Jorge Cortes, MD, of the MD Anderson Cancer Center in Houston, Texas.
“This is particularly true for patients classified by the EPI [European Prognostic Index] as poor-risk upon entering the trial.”
For this trial, Dr Cortes and his colleagues evaluated 125 patients, ages 18 to 65, from 35 centers in the US, Canada, and Europe. Patients had AML in first relapse after an initial complete remission lasting a month or longer.
They were stratified per the EPI into favorable-, intermediate-, and poor-risk groups based on the duration of their first complete remission, cytogenetics, age, and transplant history. Most patients (68%) were in the poor-risk group.
Patients were randomized 2:1 to receive CPX-351 (100 units/m2 on days 1, 3, and 5 by 90-minute infusion) or the investigators’ choice of first salvage chemotherapy. The control treatment was usually based on cytarabine and an anthracycline, often with one or more additional agents.
Patient characteristics were largely well-balanced between the treatment arms. However, the CPX-351 group had a younger median age (52 years vs 56 years), more patients with secondary AML (12.3% vs 6.8%), and a higher rate of prior transplant (27.2% vs 15.9%).
Response and survival
Response rates were higher in the CPX-351 arm than in the control arm. The rates of complete response were 37% and 31.8%, respectively. And the rates of complete response with incomplete count recovery were 12.3% and 9.1%, respectively.
However, there was no significant difference in event-free survival (EFS) or overall survival (OS) between the treatment arms.
The median EFS was 4 months in the CPX-351 arm and 1.4 months in the control arm (hazard ratio[HR]=0.66, P=0.08). And the median OS was 8.5 months and 6.3 months, respectively (HR=0.75, P=0.19).
In the poor-risk population, there was no significant improvement in EFS with CPX-351, but there was a significant improvement in OS.
The median EFS was 1.8 months in the CPX-351 arm and 1.2 months in the control arm (HR=0.63, P=0.08). And the median OS was 6.5 months and 4.2 months, respectively (HR=0.55, P=0.02).
Safety and early mortality
The early mortality rate was similar between the treatment arms at 30 days—7.4% in the CPX-351 arm and 4.5% in the control arm—and at 60 days—14.8% and 15.9%, respectively. However, at 90 days, deaths were more frequent in the control arm—21.4% and 37.9%.
Patients in the CPX-351 arm had slower neutrophil recovery than those in the control arm—42 days and 34 days, respectively. The same was true for platelet recovery—45 days and 35 days, respectively.
Delayed hematologic recovery was associated with more infection-related events, such as febrile neutropenia, bacteremia, pneumonia, sepsis, urinary tract infection, pyrexia, and cellulitis.
The researchers believe these results, along with the previously published results from a phase 2 trial of CPX-351 in patients newly diagnosed with AML, support the phase 3 study of CPX-351 as a first-line therapy in older patients with high-risk (secondary) AML.
“We were very pleased to see promising response rates in this difficult-to-treat population,” Dr Cortes said. “And we eagerly await results from Celator’s pivotal phase 3 study of CPX-351, which could fulfill a considerable unmet need in AML.”


