Photo by Bill Branson
Investigators conducting a phase 1 trial failed to follow requirements for reporting serious adverse events (AEs), including deaths, according to officials from the National Cancer Institute (NCI) and the National Institutes of Health (NIH).
The trial was an NCI-sponsored study of ibrutinib in combination with dose-adjusted temozolomide, etoposide, liposomal doxorubicin, dexamethasone, and rituximab (DA-TEDDi-R) in patients with primary CNS lymphoma.
Four patients in this trial developed invasive aspergillosis, 3 others had unconfirmed Aspergillus infections, and 2 patients died of aspergillosis in 2015.
Trial investigators did not report these events to the NCI or the institutional review board (IRB) as quickly as required by the study protocol.
In addition, the suspected relationship between Aspergillus infections and the study treatment wasn’t reported to the US Food and Drug Administration (FDA) until May 2016, several months after the second patient died of aspergillosis.
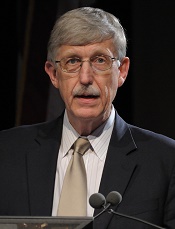
Francis S. Collins, MD, PhD, director of the NIH, and Douglas R. Lowy, MD, acting director of the NCI, discussed this delay in reporting during a meeting of the Clinical Center Hospital Board last Friday.
About the trial
The trial (NCT02203526) enrolled 18 patients with primary CNS lymphoma—13 relapsed/refractory and 5 previously untreated—between August 2014 and March 2016.
Patients received 14 days of ibrutinib (with corticosteroids to prevent cerebral edema), followed by six 21-day cycles of DA-TEDDi-R.
Twelve patients achieved a complete response following treatment, 5 had a partial response, and 1 patient progressed without responding. Eight patients remain in complete response, 2 have progressed, and 8 have died.
Four patients developed invasive aspergillosis, and 3 had possible Aspergillus infections. Two deaths, which occurred in May and December of 2015, were attributed to aspergillosis.
Some patients developed aspergillosis while they were receiving only steroids and ibrutinib, which led the investigators to believe there was a causative relationship between Aspergillus infections and treatment with ibrutinib/steroids.
The investigators stopped trial accrual in April 2016 due to the Aspergillus infections. The suspected relationship between the infections and ibrutinib/steroids was reported to the FDA in late May 2016.
Delayed reporting
On October 3, 2016, the FDA issued a 483 report to the trial’s principal investigator, Kieron Dunleavy, MD, of the NCI. The report cited “delays and deficient reporting” of serious AEs/unanticipated problems to the trial’s sponsor and IRB.
The trial’s protocol required that grade 3-5 AEs be reported to the NCI within 24 hours of occurrence and unanticipated problems be reported to the IRB within 7 days.
The median time of delayed reporting to the NCI was 40 days (range, 4 to 456), and the median time of delayed reporting to the IRB was 18 days (range, 8 to 56).
As a result of the delayed reporting, Dr Dunleavy has been suspended from conducting clinical research in the NIH Clinical Center, and holds have been placed on trials conducted by the NCI lymphoma team.
The accrual of current studies and the opening of planned studies by the lymphoma team have been stopped. The team will be allowed to resume/begin studies after they undergo training and once the NCI and an outside contractor complete an audit of all NCI lymphoma trials that have been open over the last 3 years.
Patients involved in the trial of DA-TEDDi-R (and their families) have been informed of the delayed AE reporting.
Various parties involved in NIH/NCI trials have been reminded about the importance of timely reporting of safety and regulatory information.
The NCI and NIH are taking steps to ensure that AEs are reported promptly in the future. And the Office of Research Support and Compliance has been tasked with investigating past reporting of AEs in NIH trials, particularly those conducted at the Clinical Center.


