CASE 1 Huge out-of-pocket cost makes patient forego treatment
Ms. M. is a 28-year-old patient who recently posted this on her Facebook page: “I went to the drugstore this morning to pick up a prescription, and as the pharmacist handed it to me she said, ‘That will be $180.00.’ And that’s after insurance coverage! Wow! I think I’ll pass!”
Our patients probably experience this type of situation more commonly than we know.
CASE 2 Catastrophic medical costs bankrupt family
A middle-class couple who had college degrees and full-time jobs with health insurance had twins at 24 weeks’ gestation. They accrued $450,000 in medical debt after exceeding the $2 million cap of their insurance policy. Having premature twins cost them everything. They liquidated their retirement and savings accounts, sold everything they had, and still ended up filing for bankruptcy.1
Costs indeed matter to patients, and we have a professional responsibility to help our patients navigate the murky waters of health care so that they can maintain financial as well as physical health.
Rising costs, lower yield,and opportunities for change
Rising health care costs are unsustainable for both our patients and our society. Although the United States spends more on health care than any other developed country, our health outcomes are actually worse—ranking at or near the bottom in both prevalence and mortality for multiple diseases, risk factors, and injuries.2
Of the 171 countries included in a study by the United Nations Maternal Mortality Estimation Inter-Agency Group, the United States was 1 of 13 countries that had an increasing maternal mortality and the only developed nation with an increasing maternal mortality rate.3 This tells us that, as our country spends more on health care, our patients’ health is not improving. For individuals, medical bills are now the leading cause of personal bankruptcy in the United States, even for those who are insured.4
ObGyns play an important leadership role in the practice of cost-conscious health care, as 25% of hospitalizations in the United States are pregnancy related.5,6 In addition, the wide scope of ObGyn practice reaches beyond pregnancy-related conditions and provides multiple opportunities to decrease the use of unnecessary tests and treatments.
The good news is that approximately 30% of health care costs are wasted on unnecessary care that could be eliminated without decreasing the quality of care.7
High-value change #1: Eliminate use of expensive products
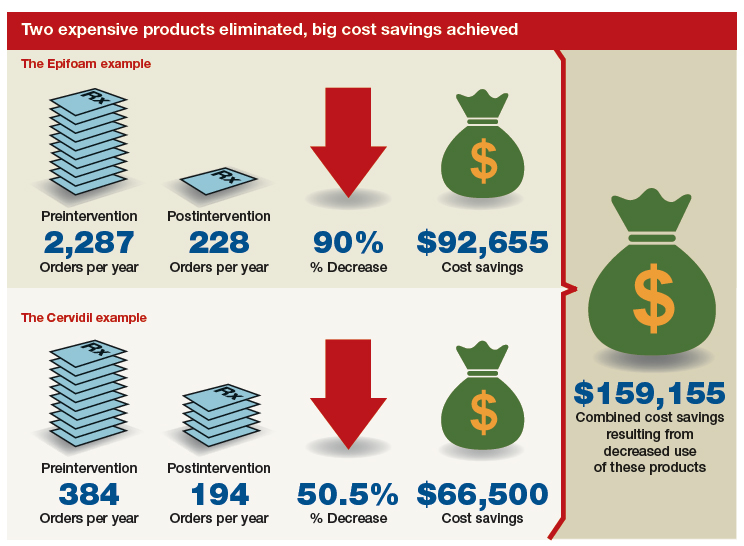
Embarking on a high-value care improvement project, experts at Greenville Health System examined the cost of different topical pain medications for perineal pain after a vaginal delivery. They found that Epifoam (hydrocortisone acetate/pramoxine hydrochloride) was ordered 2,287 times over the course of a year.
The study intervention consisted of an educational grand rounds and discussion of a Cochrane review, which concluded there was no difference in pain relief with topical anesthetics compared with placebo.8 Less expensive options for pain relief were discussed, and the department agreed to remove Epifoam as a standing order.
After the intervention, Epifoam was ordered 228 times, a 90% reduction. Over the period of a year, this translated to a cost savings of $92,655 for the hospital, with reduced charges passed on to patients.9 Thus, a seemingly small individual cost ($45.00 per can of Epifoam) can add up to a substantial sum in a large health care system.
Similarly, practitioners were educated about options for cervical ripening and were given information on the cost and efficacy of various cervical ripening agents. A Cochrane review found that oral misoprostol is as effective as vaginal misoprostol and results in fewer cesarean deliveries than vaginal dinoprostone (Cervidil).10 Practitioners were asked to consider making the transition to oral misoprostol. This action resulted in a 50.5% decrease in Cervidil use, from 384 to 194 cases, producing a cost savings of $66,500. The following year, the department removed Cervidil from the formulary as a high-value decision.9
Both of these examples illustrate what a value-minded department can accomplish by implementing performance improvement projects that focus on high-value care.
Continue to: High-value change #2: Stop ordering unnecessary lab work...