In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
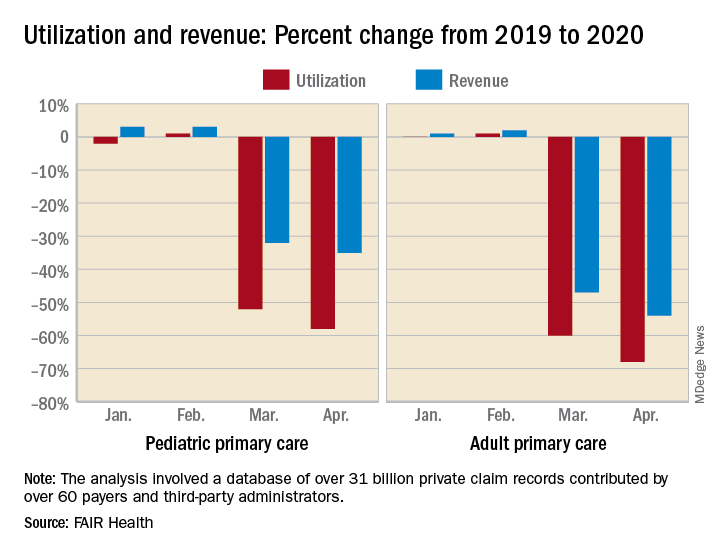
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”