according to the Agency for Healthcare Research and Quality.
That year, there were 27.4 million inpatient visits by adults with a total cost of $380.1 billion, although obstetric stays were not included in the analysis. Of those inpatient admissions, 3.5 million (12.9%) were deemed to be “avoidable, in part, through timely and quality primary and preventive care,” Kimberly W. McDermott, PhD, and H. Joanna Jiang, PhD, said in a recent AHRQ statistical brief.
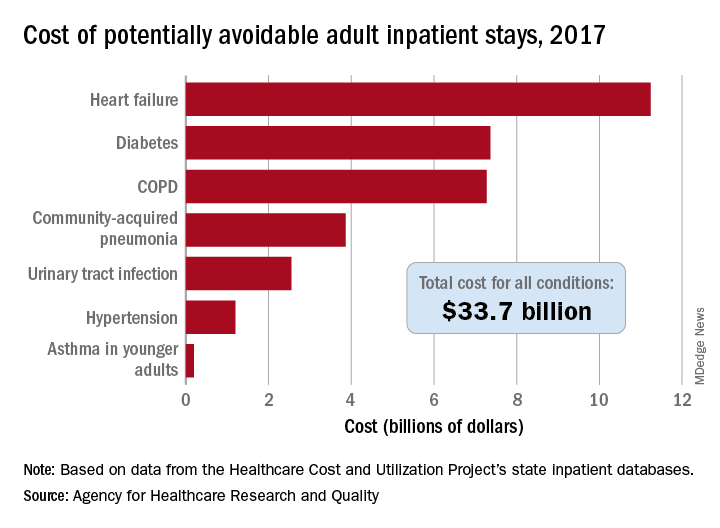
The charges for those 3.5 million visits came to $33.7 billion, or 8.9% of aggregate hospital costs in 2017, based on data from the AHRQ Healthcare Cost and Utilization Project’s state inpatient databases.
“Determining the volume and costs of potentially preventable inpatient stays can identify where potential cost savings might be found associated with reducing these hospitalizations overall and among specific subpopulations,” the investigators pointed out.
Of the seven conditions that are potentially avoidable, heart failure was the most expensive, producing more than 1.1 million inpatient admissions at a cost of $11.2 billion. Diabetes was next with a cost of almost $7.4 billion, followed by chronic obstructive pulmonary disease (COPD) at nearly $7.3 billion, they said.
Those three conditions, along with hypertension and asthma in younger adults, brought the total cost of the preventable-stay equation’s chronic side to $27.3 billion in 2017, versus $6.4 billion for the two acute conditions, community-acquired pneumonia and urinary tract infections, said Dr. McDermott of IBM Watson Health and Dr. Jiang of the AHRQ.
The rate of potentially avoidable stays for chronic conditions was higher for men (1,112/100,000 population) than for women (954/100,000), but women had a higher rate for acute conditions, 346 vs. 257, which made the overall rates similar (1,369 for men and 1,300 for women), they reported.
Differences by race/ethnicity were more striking. The rate of potentially avoidable stays for blacks was 2,573/100,000 in 2017, compared with 1,315 for Hispanics, 1,173 for whites, and 581 for Asians/Pacific Islanders. The considerable margins between those figures, however, were far eclipsed by the “other” category, which had 4,911 stays per 100,000, the researchers said.
Large disparities also can be seen when looking at community-level income. Communities with income in the lowest quartile had a preventable-hospitalization rate of 2,013/100,000, and the rate dropped with each successive quartile until it reached 878/100,000 for the highest-income communities, according to the report.
“High hospital admission rates for these conditions may indicate areas where changes to the healthcare delivery system could be implemented to improve patient outcomes and lower costs,” Dr. McDermott and Dr. Jiang wrote.
SOURCE: McDermott KW and Jiang HJ. HCUP Statistical Brief #259. June 2020.