Mr. C, age 34, presented to the emergency department with his wife because of increasingly bizarre behavior. He reported auditory and visual hallucinations, and believed that the “mob had ordered a hit” against him. He had threatened to shoot his wife and children, which led to his arrest and being briefly jailed. In jail, he was agitated, defecated on the floor, and disrobed. His wife reported that Mr. C had a long history of bipolar disorder and had experienced his first manic episode and hospitalization at age 17. Since then, he had been treated with many different antidepressants, antipsychotics, and mood stabilizers.
Mr. C was admitted to the hospital, where he developed a catatonic syndrome that was treated with a course of electroconvulsive therapy. He was eventually stabilized with olanzapine, 20 mg by mouth nightly, with moderate improvement in his symptoms, although he never fully returned to baseline.
Over the next 8 years, Mr. C was often noncompliant with medication and frequently was hospitalized for mania. His symptoms included poor sleep, grandiosity, pressured speech, racing and disorganized thoughts, increased risk-taking behavior (ie, driving at excessive speeds), and hyperreligiosity (ie, speaking with God). Mr. C also occasionally used methamphetamine, cannabis, and cocaine. Although he had responded well to treatment early in the course of his illness, as he entered his late 30s, his response was less complete, and by his 40s, Mr. C was no longer able to function independently. He eventually was prescribed a long-acting injectable antipsychotic, paliperidone palmitate, 156 mg monthly. Eventually, his family was no longer able to care for him at home, so he was admitted to a residential care facility.
In this facility, based on the long-standing nature of Mr. C’s psychotic disorder and frequency with which he presented with mania, his clinicians changed his diagnosis to schizoaffective disorder, bipolar type. It had become clear that mood symptoms comprised >50% of the total duration of his illness.
Schizoaffective disorder (SAD) often has been used as a diagnosis for patients who have an admixture of mood and psychotic symptoms whose diagnosis is uncertain. Its hallmark is the presence of symptoms of a major mood episode (either a depressive or manic episode) concurrent with symptoms characteristic of schizophrenia, such as delusions, hallucinations, or disorganized speech.1
SAD is a controversial diagnosis. There has been inadequate research regarding the epidemiology, course, etiologic factors, and treatment of this disorder. Debate continues to swirl around its conceptualization; some experts view SAD as an independent disorder, while others see SAD as either a form of schizophrenia or a mood disorder.1 In this review, we describe the classification of SAD and its features, diagnosis, and treatment.
An evolving diagnosis
The term schizoaffective was first used by Jacob Kasanin, MD, in 1933.2 He described 9 patients with “acute schizoaffective psychoses,” each of whom had an abrupt onset. The term was used in the first edition of the DSM as a subtype of schizophrenia.3 In DSM-I, the “schizo-affective type” was defined as a diagnosis for patients with a “significant admixture of schizophrenic and affective reactions.”3 Diagnostic criteria for SAD were developed for DSM-III-R, published in 1987.4 These criteria continued to evolve with subsequent editions of the DSM.
Continue to: DSM-5 provides...
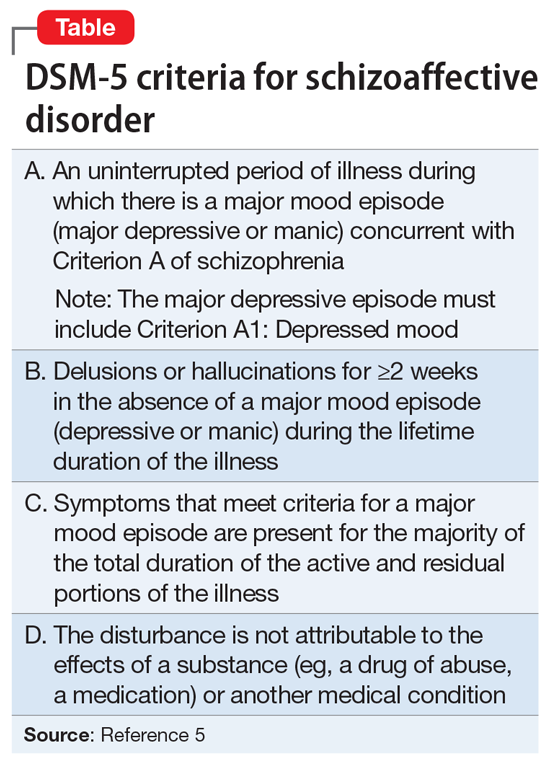
DSM-5 provides a clearer separation between schizophrenia with mood symptoms, bipolar disorder, and SAD (Table5). In addition, DSM-5 shifts away from the DSM-IV diagnosis of SAD as an episode, and instead focuses more on the longitudinal course of the illness. It has been suggested that this change will likely lead to reduced rates of diagnosis of SAD.6 Despite improvements in classification, the diagnosis remains controversial (Box7-11).
Box 1
Despite improvements in classification, controversy continues to swirl around the question of whether schizoaffective disorder (SAD) represents an independent disorder that stands apart from schizophrenia and bipolar disorder, whether it is a form of schizophrenia, or whether it is a form of bipolar disorder or a depressive disorder.7,8 Other possibilities are that SAD is heterogeneous or that it represents a middle point on a spectrum that bridges mood and psychotic disorders. While the merits of each possibility are beyond the scope of this review, it is safe to say that each possibility has its proponents. For these reasons, some argue that the concept itself lacks validity and shows the pitfalls of our classification system.7
Poor diagnostic reliability is one reason for concerns about validity. Most recently, a field trial using DSM-5 criteria produced a kappa of 0.50, which is moderate,9 but earlier definitions produced relatively poor results. Wilson et al10 point out that Criterion C, which concerns duration of mood symptoms, produces a particularly low kappa. Another reason is diagnostic switching, whereby patients initially diagnosed with 1 disorder receive a different diagnosis at followup. Diagnostic switching is especially problematic for SAD. In a large meta-analysis by Santelmann et al,11 36% of patients initially diagnosed with SAD had their diagnosis changed when reassessed. This diagnostic shift tended more toward schizophrenia than bipolar disorder. In addition, more than one-half of all patients initially diagnosed with schizophrenia, bipolar disorder, or major depressive disorder were re-diagnosed with SAD when reassessed.
DSM-5 subtypes and specifiers
In DSM-5,SAD has 2 subtypes5:
- Bipolar type. The bipolar type is marked by the presence of a manic episode (major depressive episodes may also occur)
- Depressive type. The depressive type is marked by the presence of only major depressive episodes.
SAD also includes several specifiers, with the express purpose of giving clinicians greater descriptive ability. The course of SAD can be described as either “first episode,” defined as the first manifestation of the disorder, or as having “multiple episodes,” defined as a minimum of 2 episodes with 1 relapse. In addition, SAD can be described as an acute episode, in partial remission, or in full remission. The course can be described as “continuous” if it is clear that symptoms have been present for the majority of the illness with very brief subthreshold periods. The course is designated as “unspecified” when information is unavailable or lacking. The 5-point Clinician-Rated Dimensions of Psychosis Symptoms was introduced to enable clinicians to make a quantitative assessment of the psychotic symptoms, although its use is not required.
Epidemiology and gender ratio
The epidemiology of SAD has not been well studied. DSM-5 estimates that SAD is approximately one-third as common as schizophrenia, which has a lifetime prevalence of 0.5% to 0.8%.5 This is similar to an estimate by Perälä et al12 of a 0.32% lifetime prevalence based on a nationally representative sample of persons in Finland age ≥30. Scully et al13 calculated a prevalence estimate of 1.1% in a representative sample of adults in rural Ireland. Based on pooled clinical data, Keck et al14 estimated the prevalence in clinical settings at 16%, similar to the figure of 19% reported by Levinson et al15 based on data from New York State psychiatric hospitals. In clinical practice, the diagnosis of SAD is used frequently when there is diagnostic uncertainty, which potentially inflates estimates of lifetime prevalence.
The prevalence of SAD is higher in women than men, with a sex ratio of about 2:1, similar to that seen in mood disorders.13,16-19 There are an equal number of men and women with the bipolar subtype, but a female preponderance with the depressive subtype.5 The bipolar subtype is more common in younger patients, while the depressive subtype is more common in older patients. SAD is a rare diagnosis in children.20
Continue to: Course and outcome
Course and outcome
The onset of SAD typically occurs in early adulthood, but can range from childhood to senescence. Approximately one-third of patients are diagnosed before age 25, one-third between age 25 and 35, and one-third after age 35.21-23 Based on a literature review, Cheniaux et al7 concluded that that age at onset for patients with SAD is between those with schizophrenia and those with mood disorders.
The course of SAD is variable but represents a middle ground between that of schizophrenia and the mood disorders. In a 4- to 5-year follow-up,24 patients with SAD had a better overall course than patients with schizophrenia but had poorer functioning than those with bipolar mania, and much poorer than those with unipolar depression. Mood-incongruent psychotic features predict a particularly worse outcome. These findings were reaffirmed at a 10-year follow-up.25 Mood symptoms portend a better outcome than do symptoms of schizophrenia.
The lifetime suicide risk for patients with SAD is estimated at 5%, with a higher risk associated with the presence of depressive symptoms.26 One study found that women with SAD had a 17.5-year reduced life expectancy (64.1 years) compared with a reduction of 8.0 years for men (69.4 years).27
Comorbidity
Patients with SAD are commonly diagnosed with other psychiatric disorders, including anxiety disorders, obsessive-compulsive disorder, posttraumatic stress disorder, and substance use disorders.21,28,29 When compared with the general population, patients with SAD are at higher risk for coronary heart disease, stroke, obesity, and smoking, likely contributing to their decreased life expectancy.27,30 Because second-generation antipsychotics (SGAs) are often used to treat SAD, patients with SAD are at risk for metabolic syndrome and diabetes mellitus.30
Clinical assessment
Because there are no diagnostic, laboratory, or neuroimaging tests for SAD, the most important basis for making the diagnosis is the patient’s history, supplemented by collateral history from family members or friends, and medical records. Determining the percentage of time spent in a mood episode (DSM-5 Criterion C) is especially important.31 This requires the clinician to pay close attention to the temporal relationship of psychotic and mood symptoms.
Continue to: Differential diagnosis
Differential diagnosis
The differential diagnosis for SAD is broad because it includes all of the possibilities usually considered for major mood disorders and for psychotic disorders5:
- schizophrenia
- bipolar disorder with psychotic features
- major depressive disorder with psychotic features
- depressive or bipolar disorders with catatonic features
- personality disorders (especially the schizotypal, paranoid, and borderline types)
- major neurocognitive disorders in which there are mood and psychotic symptoms
- substance/medication-induced psychotic disorder
- disorders induced by medical conditions.
With schizophrenia, the duration of all episodes of a mood syndrome is brief (<50% of the total duration of the illness) relative to the duration of the psychotic symptoms. Although psychotic symptoms may occur in persons with mood disorders, they are generally not present in the absence of depression or mania, helping to set the boundary between SAD and psychotic mania or depression. As for personality disorders, the individual will not have a true psychosis, although some symptoms, such as feelings of unreality, paranoia, or magical thinking, may cause diagnostic confusion.
Medical conditions also can present with psychotic and mood symptoms and need to be ruled out. These include psychotic disorder due to another medical condition, and delirium. A thorough medical workup should be performed to rule out any possible medical causes for the symptoms.
Substance use should also be ruled out as the cause of the symptoms because many substances are associated with mood and psychotic symptoms. It is usually clear from the history, physical examination, or laboratory tests when a medication/illicit substance has initiated and maintained the disorder.
Neurologic conditions. If a neurologic condition is suspected, a neurologic evaluation may be warranted, including laboratory tests, brain imaging to identify specific anatomical abnormalities, lumbar puncture with cerebrospinal fluid analysis, and an electroencephalogram to rule out a convulsive disorder.
Continue to: Clinical symptoms
Clinical symptoms
The signs and symptoms of SAD include those typically seen in schizophrenia and the mood disorders. Thus, the patient may exhibit elated mood and/or grandiosity, or severe depression, combined with mood-incongruent psychotic features such as paranoid delusions. The symptoms may present together or in an alternating fashion, and psychotic symptoms may be mood-congruent or mood-incongruent. Mr. C’s case illustrates some of the symptoms of the disorder.
Brain imaging
Significant changes have been reported to occur in the brain structure and function in persons with SAD. Neuroimaging studies using voxel-based morphometry have shown significant reductions in gray matter volume in several areas of the brain, including the medial prefrontal cortex, insula, Rolandic operculum, parts of the temporal lobe, and the hippocampus.32-35 Amann et al32 found that patients with SAD and schizophrenia had widespread and overlapping areas of significant volume reduction, but patients with bipolar disorder did not. These studies suggest that at least from a neuroimaging standpoint, SAD is more closely related to schizophrenia than bipolar disorder, and could represent a variant of schizophrenia.
Treatment of SAD
The pharmacotherapy of SAD is mostly empirical because of the lack of randomized controlled trials. Clinicians have traditionally prescribed an antipsychotic agent along with either a mood stabilizer (eg, lithium, valproate) or an antidepressant, depending on the patient’s SAD subtype. Jäger et al36 reviewed 33 treatment studies published up to 2007 that employed widely accepted diagnostic criteria and reported results for SAD patients. They concluded that mood stabilizers and antipsychotics appeared to be effective, but that it was not possible to provide treatment guidelines.
Since that exhaustive review, aripiprazole was compared with placebo in 2 separate trials that include patients with schizophrenia and patients with SAD.37 In a pooled sub-analysis of SAD, aripiprazole was found to be more effective on some but not all measures, suggesting efficacy. Based on 2 randomized controlled trials, the FDA approved the use of paliperidone, an SGA, as monotherapy in the acute treatment of SAD and in combination with mood stabilizers and/or antidepressants.38,39 It is likely that other SGAs are also effective.
Patients with SAD will require maintenance treatment for ongoing symptom control. Medication that is effective for treatment of an acute episode should be considered for maintenance treatment. Both the extended-release and long-acting injectable (LAI) formulations of paliperidone have been shown to be efficacious in the maintenance treatment of patients with SAD.40 The LAI form of paliperidone significantly delayed psychotic, depressive, and manic relapses, improved clinical rating scale scores, and increased medication adherence.41,42 In an open-label study, olanzapine LAI was effective in long-term maintenance treatment, although approximately 40% of patients experienced significant weight gain.43 One concern with olanzapine is the possible occurrence of a post-injection delirium/sedation syndrome. For that reason, patients receiving olanzapine must be monitored for at least 3 hours post-injection. The paliperidone LAI does not require monitoring after injection.
Continue to: There is a single clinical trial...
There is a single clinical trial showing that patients with SAD can be successfully switched from other antipsychotics to lurasidone, although this study had no long-term follow-up.44
Other approaches
Electroconvulsive therapy (ECT) should be considered for patients with SAD who are acutely ill and have failed to respond adequately to medication. ECT is especially relevant in the setting of acute mood symptoms (ie, depressive or manic symptoms co-occurring with psychosis or in the absence of psychosis).45
As currently conceptualized, the diagnosis of SAD is made in persons having an admixture of mood and psychotic symptoms, although by definition mood symptoms must take up the majority (≥50%) of the total duration of the illness. Unfortunately, SAD has been inadequately researched due to the unreliability of its definition and concerns about its validity. The long-term course of SAD is midway between mood and psychotic disorders, and the disorder can cause significant disability.
Bottom Line
Schizoaffective disorder (SAD) is characterized by the presence of symptoms of a major mood episode (a depressive or manic episode) concurrent with symptoms of schizophrenia. The most important basis for establishing the diagnosis is the patient’s history. Determining the percentage of time spent in a mood episode is especially important. Treatment usually consists of an antipsychotic plus a mood stabilizer or antidepressant. Electroconvulsive therapy is an option for patients with SAD who do not respond well to medication.
Related Resources
- Wy TJP, Saadabadi A. Schizoaffective disorder. NCBI Bookshelf: StatPearls Publishing. Published January 2020. https://www.ncbi.nlm.nih.gov/books/NBK541012/. Updated April 15, 2020.
- Parker G. How well does the DSM-5 capture schizoaffective disorder? Can J Psychiatry. 2019;64(9):607-610.
Drug Brand Names
Aripiprazole • Abilify
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Olanzapine • Zyprexa
Olanzapine long-acting injectable • Zyprexa Relprevv
Paliperidone • Invega
Paliperidone palmitate • Invega sustenna
Valproate • Depacon