The United States has allocated more than 641,000 monoclonal antibody treatments for outpatients to ease pressure on strained hospitals, but officials from Operation Warp Speed report that more than half of that reserve sits unused as clinicians grapple with best practices.
There are space and personnel limitations in hospitals right now, Janet Woodcock, MD, therapeutics lead on Operation Warp Speed, acknowledges in an interview with this news organization. “Special areas and procedures must be set up.” And the operation is in the process of broadening availability beyond hospitals, she points out.
But for frontline clinicians, questions about treatment efficacy and the logistics of administering intravenous drugs to infectious outpatients loom large.
More than 50 monoclonal antibody products that target SARS-CoV-2 are now in development. The U.S. Food and Drug Administration has already issued Emergency Use Authorization (EUA) for two such drugs on the basis of phase 2 trial data – bamlanivimab, made by Eli Lilly, and a cocktail of casirivimab plus imdevimab, made by Regeneron – and another two-antibody cocktail from AstraZeneca, AZD7442, has started phase 3 clinical trials. The Regeneron combination was used to treat President Donald Trump when he contracted COVID-19 in October.
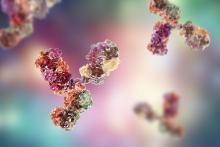
Monoclonal antibody drugs are based on the natural antibodies that the body uses to fight infections. They work by binding to a specific target and then blocking its action or flagging it for destruction by other parts of the immune system. Both bamlanivimab and the casirivimab plus imdevimab combination target the spike protein of the virus and stop it from attaching to and entering human cells.
Targeting the spike protein out of the hospital
The antibody drugs covered by EUAs do not cure COVID-19, but they have been shown to reduce hospitalizations and visits to the emergency department for patients at high risk for disease progression. They are approved to treat patients older than 12 years with mild to moderate COVID-19 who are at high risk of progressing to severe disease or hospitalization. They are not authorized for use in patients who have been hospitalized or who are on ventilators. The hope is that antibody drugs will reduce the number of severe cases of COVID-19 and ease pressure on overstretched hospitals.
Most COVID-19 patients are outpatients, so we need something to keep them from getting worse.
This is important because it targets the greatest need in COVID-19 therapeutics, says Rajesh Gandhi, MD, an infectious disease physician at Harvard Medical School in Boston, who is a member of two panels evaluating COVID-19 treatments: one for the Infectious Disease Society of America and the other for the National Institutes of Health. “Up to now, most of the focus has been on hospitalized patients,” he says, but “most COVID-19 patients are outpatients, so we need something to keep them from getting worse.”
Both panels have said that, despite the EUAs, more evidence is needed to be sure of the efficacy of the drugs and to determine which patients will benefit the most from them.
These aren’t the mature data from drug development that guideline groups are accustomed to working with, Dr. Woodcock points out. “But this is an emergency and the data taken as a whole are pretty convincing,” she says. “As I look at the totality of the evidence, monoclonal antibodies will have a big effect in keeping people out of the hospital and helping them recover faster.”
High-risk patients are eligible for treatment, especially those older than 65 years and those with comorbidities who are younger. Access to the drugs is increasing for clinicians who are able to infuse safely or work with a site that will.
In the Boston area, several hospitals, including Massachusetts General where Dr. Gandhi works, have set up infusion centers where newly diagnosed patients can get the antibody treatment if their doctor thinks it will benefit them. And Coram, a provider of at-home infusion therapy owned by the CVS pharmacy chain, is running a pilot program offering the Eli Lilly drug to people in seven cities – including Boston, Chicago, Los Angeles, and Tampa – and their surrounding communities with a physician referral.
Getting that referral could be tricky, however, for patients without a primary care physician or for those whose doctor isn’t already connected to one of the institutions providing the infusions. The hospitals are sending out communications on how patients and physicians can get the therapy, but Dr. Gandhi says that making information about access available should be a priority. The window for the effective treatment is small – the drugs appear to work best before patients begin to make their own antibodies, says Dr. Gandhi – so it’s vital that doctors act quickly if they have a patient who is eligible.
And rolling out the new therapies to patients around the world will be a major logistical undertaking.
The first hurdle will be making enough of them to go around. Case numbers are skyrocketing around the globe, and producing the drugs is a complex time- and labor-intensive process that requires specialized facilities. Antibodies are produced by cell lines in bioreactors, so a plant that churns out generic aspirin tablets can’t simply be converted into an antibody factory.
“These types of drugs are manufactured in a sterile injectables plant, which is different from a plant where oral solids are made,” says Kim Crabtree, senior director of pharma portfolio management for Henry Schein Medical, a medical supplies distributor. “Those are not as plentiful as a standard pill factory.”
The doses required are also relatively high – 1.2 g of each antibody in Regeneron’s cocktail – which will further strain production capacity. Leah Lipsich, PhD, vice president of strategic program direction at Regeneron, says the company is prepared for high demand and has been able to respond, thanks to its rapid development and manufacturing technology, known as VelociSuite, which allows it to rapidly scale-up from discovery to productions in weeks instead of months.
“We knew supply would be a huge problem for COVID-19, but because we had such confidence in our technology, we went immediately from research-scale to our largest-scale manufacturing,” she says. “We’ve been manufacturing our cocktail for months now.”
The company has also partnered with Roche, the biggest manufacturer and vendor of monoclonal antibodies in the world, to manufacture and supply the drugs. Once full manufacturing capacity is reached in 2021, the companies expect to produce at least 2 million doses a year.
Then there is the issue of getting the drugs from the factories to the places they will be used.
Antibodies are temperature sensitive and need to be refrigerated during transport and storage, so a cold-chain-compliant supply chain is required. Fortunately, they can be kept at standard refrigerator temperatures, ranging from 2° C to 8° C, rather than the ultra-low temperatures required by some COVID-19 vaccines.