CHICAGO – With reimbursements declining, finding the money to sustain trauma centers is becoming even more crucial for hospitals and the trauma surgeons who staff them, but a Mississippi "play or pay" policy for trauma centers could be a model for other states, according to a recent study.
"The ‘play or pay’ policy in Mississippi was associated with an increase in trauma system participation, and it created increased access for Mississippians, particularly in the southern part of the state," Dr. Ben L. Zarzaur said at the annual meeting of the American Association for the Surgery of Trauma.
Dr. Zarzaur presented an analysis of the state’s "play or pay" program based on 2,815 trauma admissions to the Presley Memorial Trauma Center in Memphis, a level I trauma center that covers southwestern Tennessee and northern Mississippi. Although Mississippi has had a fund for trauma centers for most of the last decade, the Mississippi Trauma Care System Fund underwent a major change in 2008 when the state implemented a "play or pay" policy.
He noted that readiness costs for level I trauma centers were about $2.7 million a year in 2004 (Am. J. Surg. 2004;187:7-13). Under "play or pay," hospitals now either establish a trauma center at a level that the state deems sufficient, or they pay into the fund.
"Fundamentally, 'play or pay' is a social contract with citizens and patients of the most important type."
For example, a hospital with a level III center that the state says should be a level II facility would pay $423,500, and fees can range up to $1.5 million, according to Dr. Zarzaur, a surgeon at the University of Tennessee Health Science Center, Memphis, and the Presley Memorial Trauma Center. Out-of-state trauma centers may participate if an independent review team determines that they comply with Mississippi regulations.
About 15% of the Trauma Care System Fund comes from these hospital fees, said Dr. John Porter of Jackson, Miss., an attendee at the paper presentation and a policy author and trauma surgeon at the University of Mississippi, Oxford, which has the only in-state level I center. The fund had accumulated more than $24 million through 2010, Dr. Zarzaur said. Funding also comes from motor vehicle fees and fines.
Before the policy was enacted in July 2008, 70 of 107 hospitals had trauma centers and two level I centers served the state, Dr. Zarzaur said. Today, 85 of 106 hospitals have trauma centers and a third level I center (the University of South Alabama in neighboring Mobile) has joined the program. "There was also an increase in level II centers in the southern part of the state, which had previously been underserved," Dr. Zarzaur noted.
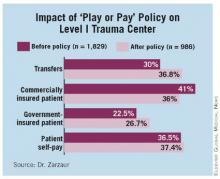
The study found a shift in the payer mix after the policy was put in place, despite similar patient demographics, injury severity, and mortality. Associated with this change in payer mix was an increase in transfers from referring facilities, Dr. Zarzaur said. Among residents of Mississippi, "there was a decrease in the number of commercially insured patients and an increase in government-insured as well as self-pay patients, but there was no similar change in the Tennessee cohort," he said.
Overall, commercially insured patients made up 41% of patients admitted from Mississippi before the policy, compared with 36% since. The ratio of reimbursements to charges declined under the policy to 0.22, compared with 0.26 previously, with a ratio of 1 indicating profit, Dr. Zarzaur said.
At Presley, reimbursements for all patients decreased slightly for the entire cohort, Dr. Zarzaur said. Although that was more pronounced for Mississippians, "play or pay" made up for it. "Funds received from the Trauma Care System Fund almost completely offset this unfavorable change in payer mix," Dr. Zarzaur said.
Discussion leader Dr. David B. Hoyt, professor emeritus of surgery at the University of California, Irvine, and executive director of the American College of Surgeons, applauded the concept. "Fundamentally, ‘play or pay’ is a social contract with citizens and patients of the most important type: It legislates our responsibility to a safety net and allows hospitals to participate either directly or through financial support," he said.
He also noted that California tried to employ a similar funding scheme but abandoned it. "There’s a lesson in this about the persistence and the timing of a policy development that has implications for the AAST and the ACS Committee on Trauma," he said. "This is probably one of best ideas that will come forth as we consider ideas for refinancing our health system."