Providing patients and their families with information and education about their psychiatric illness is a central tenet of mental health care. Discussions about diagnostic impressions, treatment options, and the risks and benefits of interventions are customary. Additionally, patients and families often receive written material or referral to other information sources, including self-help books and a growing number of online resources. Although patient education remains a useful and expected element of good care, there is evidence that, alone, it is insufficient to change health behaviors.1
A growing body of literature and clinical experience suggests that self-management strategies complement patient education and improve treatment outcomes for patients with chronic illnesses, including psychiatric conditions.2,3 The Cochrane Collaboration describes patient education as “teaching or training of patients concerning their own health needs,” and self-management as “the individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a long-term disorder.”4
In this article, we review:
• characteristics of long-term care models
• literature supporting the benefits of self-management programs
• clinical initiatives illustrating important elements of self-management support
• opportunities and challenges faced by clinicians, patients, families, clinics, and healthcare systems implementing self-management programs.
Principles of self-management
Chronic care models must account for conditions in which the clinical course can be variable, that are not amenable to a cure, and that demand long-term treatment. Optimal health outcomes rely on patients accurately monitoring, reporting, and responding to their symptoms, while engaging in critical health-related behaviors. In addition, clinicians must teach, partner with, and motivate patients to engage in crucial disease-management activities. Although typically not considered in this light, we believe most psychiatric disorders are best approached through a long-term care model, and benefit from self-management principles.
Basics of self-management include:
• patients must formulate goals and learn skills relevant to their disease
• problems are patient-selected and targeted with individualized, flexible treatment plans.
Corbin and Strauss believe effective “self-managers” achieve competency in three areas:
• role management, which entails healthy adjustments to changes in role
responsibilities, expectations, and self-identity
• emotional management, which often is particularly challenging in psychiatric conditions because of the emotional disruption inherent in living with a psychiatric illness.6
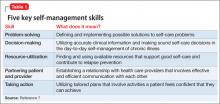
Proficiency in these three “self-manager” domains is enhanced by mastering five key self-management skills outlined in Table 1.7
Successful intervention programs vary widely with regard to individual vs group formats, communication interface, and involved health professionals. However, evidence indicates that problem solving, decision making, and action planning are key components.7 Successful planning includes:
• detailed descriptions of what, how, when, and where the activity will be accomplished
• assessment of patient confidence and adjustment of plans if confidence is limited
• continuous monitoring and self-tailoring of plans through collaborative discussions with providers, fostering a spirit of partnership and ownership.
Table 2 illustrates elements of successful action plans in our Action Planning Worksheet. Adapted from the work of Scharzer,8 Prochaska,9 and Clark,10 we developed this self-management tool for individual and group treatment settings. It serves as a vehicle for collaborative patient-provider discussion and planning. The nuts-and-bolts nature of the discussions inevitably leads to learning new, important, and often unexpected information about our patients’ daily lives and the challenges they face as they share their dominant priorities, fears, and insecurities.
Patients provide consistently positive feedback about action planning, and clinicians often find that the process reveals fruitful areas for further psychotherapeutic intervention. Examples include identifying a range of negative automatic thoughts or catastrophic thinking impeding initiation of important activation, and exposure activities for depressed or anxious patients.