SAN FRANCISCO – Patients with sepsis had significantly higher rates of persistent lymphopenia, 28-day mortality, and 1-year mortality if they were hypothermic, compared with normothermic patients in a small retrospective study.
In the study, 32 of 58 septic patients who were hypothermic within 24 hours of their blood cultures developed persistent lymphopenia (55%), compared with 43% of 183 normothermic patients and 48% of 204 febrile patients.
Dr. Anne Drewry reported that hypothermia was associated with a nearly tripled risk for persistent lymphopenia (odds ratio, 2.7) compared with normothermic patients in a multivariate logistic regression analysis to account for confounding variables. The likelihood of persistent lymphopenia in febrile patients was not significantly different from that of normothermic patients.
The significantly higher risk of persistent lymphopenia in patients with hypothermia compared with normothermia was accompanied by significantly higher risk for some secondary adverse outcomes in the observational cohort study, she reported at the Critical Care Congress, sponsored by the Society for Critical Care Medicine.
Thirty-nine hypothermic patients developed septic shock (67%), compared with 55% of normothermic patients and 47% of febrile patients.
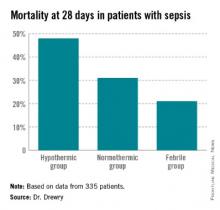
Mortality rates at 28 days were 48% in the hypothermic group (28 patients), 31% in the normothermic group, and 21% in the febrile group (which was significantly lower compared with the normothermic patients). At 1 year, 35 hypothermic patients had died (60%) compared with 45% of normothermic patients and 39% of febrile patients, she said.
"Hypothermic patients may be candidates for early treatment with agents that reverse sepsis-induced lymphopenia in future clinical trials," said Dr. Drewry of Washington University, St. Louis.
She and her associates studied data on 455 patients hospitalized between January 2010 and July 2012 and diagnosed with sepsis, and whose blood cultures were positive for bacterial or fungal organisms within 5 days of admission. They considered patients to be hypothermic if their most extreme temperature values within the first 24 hours of blood cultures were less than 36° C and to be febrile if the temperature values were 38.3° C or higher.
Data on 335 patients were analyzed for the primary outcome of persistent lymphopenia, not counting 110 patients who died or were discharged prior to day 4 after sepsis diagnosis or who had no blood counts drawn on day 4.
Mean APACHE II (Acute Physiology and Chronic Health Evaluation II) scores at baseline were 22 in the hypothermic group, significantly higher than the mean score of 16 in normothermic patients and 17 in febrile patients. Higher APACHE II scores were the only variable besides hypothermia to be significantly associated with increased risk of persistent lymphopenia; higher scores conferred a 7% increase in risk.
Hypothermic patients were significantly more likely to be infected with gram-negative organisms (50%) than were normothermic patients (36%) or febrile patients (34%).
The three groups did not differ significantly in rates of acute kidney injury, secondary infection, or need for mechanical ventilation, among secondary outcomes in a univariate analysis. Factors that were not significantly associated with persistent lymphopenia risk in the multivariable analysis included the presence of comorbidity and the type of organism (gram-positive, gram-negative, fungal, or polymicrobial).
Hypothermia occurs in 10%-25% of critically ill patients with sepsis, Dr. Drewry said. A prior study by other investigators suggested that severely septic patients with hypothermia are older, have more severe disease, and are at higher risk of death than normothermic or febrile patients (Crit. Care 2013;17:R271).
"Previous data from our group suggests that persistent lymphopenia predicts mortality and secondary infection in septic patients and may be a marker for sepsis-induced immunosuppression" even after accounting for possible confounders, Dr. Drewry said.
It’s unclear why some patients don’t mount a fever in response to infection and why these patients have worse outcomes, she added. "Our overarching hypothesis is that hypothermia in response to infection is a sign of an underlying predisposition to sepsis-induced immunosuppression."
The study excluded patients diagnosed with hematological or immunological disease and patients treated with chemotherapy or corticosteroids while hospitalized or within 6 months before admission.
Dr. Drewry reported having no financial disclosures.
sboschert@frontlinemedcom.com On Twitter @sherryboschert