Mothers did not transmit hepatitis B virus to their offspring when their viral load was less than 5 x 107 IU/mL, even when the mothers tested positive for e antigen, researchers reported online May 26 in Annals of Internal Medicine.
"Prenatal treatments, such as oral antiviral agents, are unlikely to be of additional benefit in this population and may cause harm, even if used only for short periods, by inducing viral resistance or post-treatment hepatitis flares," said Ai Kubo, Ph.D., of the Kaiser Permanente division of research in Oakland, Calif., and her associates.
Vertical transmission occurred in 3.61 of every 100 live births to mothers whose viral loads exceeded the 5 x 107 IU/mL cutoff, the researchers reported (95% confidence interval, 0.75-10.56). "Future studies to evaluate the effectiveness of additional prophylaxis measures, such as late-pregnancy antiviral treatment, are warranted among these high-risk women," they said.
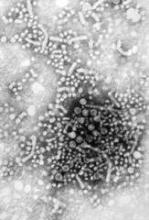
The observational study included 4,446 infants born to 3,253 hepatitis B virus (HBV)-positive mothers between 1997 and 2010. The mothers were members of the Kaiser Permanente Northern California integrated health services delivery organization, which has a centralized program of prenatal screening and neonatal immunoprophylaxis for HBV. The investigators searched electronic health data records to identify women who tested positive for HBV surface antigen and were due to deliver within 4 months, then tracked their infants to verify that they received HBV immunoglobulin and HBV vaccine (Ann. Int. Med. 2014 May 27 [doi: 10.7326/M13-2529]).
An estimated 0.75 infants were infected with HBV per 100 live births, the researchers reported (Poisson 95% confidence interval, 0.48-1.10). Infants born to e antigen–positive mothers had an infection rate of 3.37 per 100 live births (95% CI, 2.08-5.14), compared with 0.04 (95% CI, 0.001-0.24) for mothers who tested negative for e antigen. The lowest viral level associated with transmission was 6.32 x 107 IU/mL, the investigators said.
The centralized program expanded over time, so by 2010 most mothers who tested positive for HBV surface antigen underwent prenatal testing for e antigen status and HBV viral load, the researchers also reported. In addition, almost all offspring of infected mothers received HBV immunoglobulin, a complete series of HBV vaccine within recommended time frames, and follow-up testing for HBV immune response and infection.
"Our results suggest that an organized program with high rates of prenatal screening, detection, and immunoprophylaxis can effectively prevent vertical transmission of hepatitis B," said Dr. Kubo and her associates. But they cautioned that "a centralized approach may be difficult to implement in many prenatal settings."
Kaiser Permanente Community Benefit and the National Institutes of Health funded the study. Dr. Kubo reported no conflicts of interest.