The physician recognized this as a typical presentation of primary pulmonary tuberculosis (TB).
TB is a bacterial infection caused by M tuberculosis, an obligate intracellular pathogen that is aerobic, acid fast, and nonencapsulated. More than 8 million cases occur annually around the world, with nearly 2 million TB-related deaths. In 2010, the multiple-drug resistant TB rate in the United States was 1.2% (88 cases)—a rate that remains relatively stable. Based on the 2010 data, 60% of US cases of M tuberculosis occurred in foreign-born individuals.
Prophylactic treatment of those with latent TB (infection without active disease—diagnosed by tuberculin skin test conversion from negative to positive or by an interferon gamma release assay performed on blood) can reduce the risk of active TB by 90% or more.
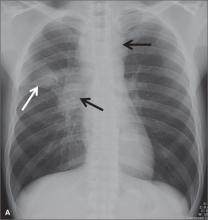
TB is transmitted by aerosolized respiratory droplet nuclei. TB usually localizes to the middle and upper lung zones accompanied by hilar and paratracheal lymphadenopathy (as the tubercle bacilli spread from lung to lymphatic vessels). Early nonspecific signs and symptoms include fever, night sweats, fatigue, anorexia, weight loss. On exam, crackles or rhonchi will be present. Later, patients develop a nonproductive cough (lasting 2-3 weeks) or a cough with purulent sputum. Patients with extensive disease may develop dyspnea or acute respiratory distress syndrome.
Initial treatment centers on administering the following 4 medications together for 2 months: isoniazid (INH), rifampin, pyrazinamide, and ethambutol. This is followed by a 4-month continuation phase with INH and rifampin.
In this case, the patient was admitted to a private room with negative pressure; the patient’s sputum was sent for acid-fast bacillus (AFB) stain and cultures. The results showed acid-fast bacilli consistent with Mycobacterium spp. While culture results were pending, the patient was started on the 4 anti-tuberculosis drug regimen. Fortunately, the sputum culture result showed pan susceptible Mycobacterium tuberculosis, and his treatment continued with directly observed therapy through the local city health department.
Figure courtesy of Carlos Santiago Restrepo, MD. Text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith, M. Tuberculosis. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:310-319.
To learn more about the Color Atlas of Family Medicine, see: http://www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking this link: http://usatinemedia.com/