HT: Minimizing the risks of stroke, deep vein thrombosis, pulmonary embolism, and breast cancer
Results of multiple studies have shown that certain HT regimens increase the risk of stroke, deep vein thrombosis, pulmonary embolism, and breast cancer. Is it possible to prescribe HT in a way that reduces these risks?
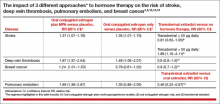
Results of observational studies indicate that, compared with oral estrogen therapy, transdermal HT is associated with a lower risk of stroke, deep vein thrombosis, pulmonary embolism, and breast cancer (TABLE).9−15
Reducing the risk of stroke caused by HT is an important goal. In a study of 15,710 women who had stroke and 59,958 control women aged 50 to 79 years, transdermal estradiol at a dose of 50 µg or less daily was not associated with an increased risk of stroke, compared with HT nonuse (rate ratio, 0.81; 95% CI, 0.62−1.05).9 Compared with HT nonuse, the use of oral estrogen (rate ratio, 1.28; 95% CI, 1.15−1.42) or transdermal estradiol 50 µg or greater daily (rate ratio, 1.89; 95% CI, 1.15−3.11) was associated with an increased risk of stroke.9
Reducing the risks of deep venous thromboembolism (VTE) and pulmonary embolism caused by HT is an important goal. In a meta-analysis of the risk of VTE with HT, compared with nonusers, oral estrogen therapy was associated with a significantly increased risk of VTE (odds ratio [OR], 2.5; 95% CI, 1.9−3.4). Compared with nonuse, transdermal estrogen therapy was not associated with an increased risk of VTE (OR, 1.2; 95% CI, 0.9−1.7).11 In a study comparing oral versus transdermal estradiol, transdermal estradiol was associated with a reduced risk of pulmonary embolism (0.46 [95% CI, 0.22−0.97]).13
Reducing the risk of breast cancer caused by HT is an important goal. Results of one study showed that the combination of oral estrogen plus synthetic progestin was associated with an increased risk of breast cancer, compared with nonuse (RR, 1.5; 95% CI, 1.1−1.9). By contrast, the combination of transdermal estradiol plus micronized progesterone was not associated with an increased risk of breast cancer, compared with nonuse (RR, 0.9; 95% CI, 0.7−1.2).15
Tell us! Send your Letter to the Editor!
The bottom line
In recently menopausal women with moderate to severe hot flashes, HT improves quality of life and appears to decrease mortality. However, HT with oral estrogen plus synthetic progestin is associated with an increased risk of stroke, deep vein thrombosis, pulmonary embolism, and breast cancer. Compared with oral estrogen, transdermal estradiol treatment is associated with a lower risk of stroke, deep vein thrombosis, and pulmonary embolism. Compared with oral estrogen plus a synthetic progestin, transdermal estradiol plus micronized progesterone is associated with a lower risk of breast cancer. The benefits of HT are likely maximized by initiating therapy in the perimenopause transition or early in the postmenopause, and the risks are minimized by using transdermal estradiol.16−18
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.