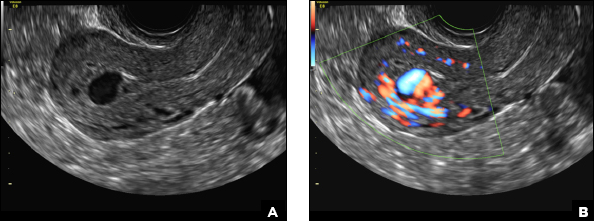
A) Retained products of conception (RPOC) INCORRECT
RPOC is a common complication arising from the presence of retained placental or fetal tissue after delivery, spontaneous, or elective abortion and is diagnosed by the presence of chorionic villi suggesting trophoblastic or placental tissue.1,2 Interpreting imaging findings is often a challenge secondary to the nonspecific findings of RPOC and often overlapping imaging features with blood products and enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). Management usually is based on clinical findings in collaboration with supportive imaging features. On ultrasound, RPOC is suspected when there is a thickened endometrial echo complex (>8 mm to 13 mm) and/or the presence of an endometrial mass. Additionally, increased vascularity on color Doppler significantly increases the likelihood of RPOC; the absence of vascularity can be seen with both blood products and avascular RPOC.1 Vascularity in RPOC can be differentiated from EMV by its extension into the endometrium.
Retained products of conception (RPOC) and hemorrhage. A) Color Doppler ultrasound of a postpartum uterus after spontaneous vaginal delivery (SVD) demonstrates a thickened endometrial echo complex with an endometrial mass and increased vascularity (long arrow) suspicious for RPOC. The patient was managed conservatively with biweekly ultrasound until the bleeding resolved at 4 weeks. B) Color Doppler ultrasound of a different patient’s postpartum uterus following SVD demonstrates an echogenic endometrial mass but without flow on color Doppler (short arrow), which may represent avascular RPOC or hemorrhage. The patient was later clinically diagnosed with RPOC. C) Color Doppler ultrasound of a third patient’s postpartum uterus. Status post-vaginal birth after cesarean with heavy bleeding showed an expanded endometrium filled with avascular echogenic mass (arrowhead), which may represent either avascular RPOC or hemorrhage. She was given a diagnosis of postpartum hemorrhage and treated with misoprostol.
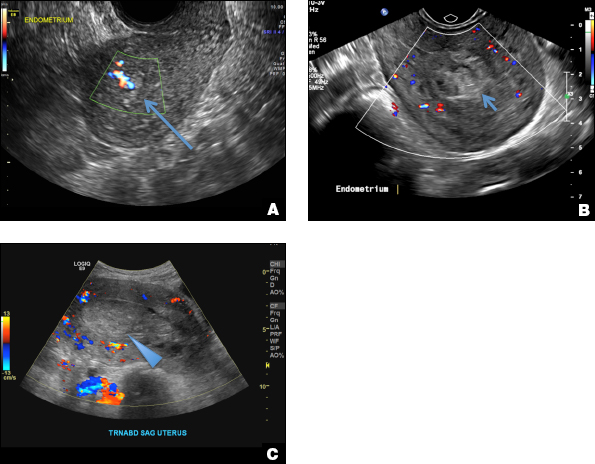
B) Complete hydatidiform mole INCORRECT
Complete hydatidiform mole (CHM) usually presents early in gestation with markedly elevated β-hCG. On ultrasound, it appears classically as an echogenic mass with innumerable small cystic spaces creating a “snowstorm or cluster of grape appearance” from hydropic chorionic villi along with larger irregular fluid collections and the absence of fetal parts.3 Ovarian hyperstimulation from elevated β-hCG can result in large bilateral ovarian cysts called theca lutein cysts.3
Complete hydatidiform mole. A) Transvaginal grayscale ultrasound of the uterus demonstrates an echogenic mass with innumerable small cystic spaces (long arrow) creating a “snowstorm or cluster of grape appearance.” B) Color Doppler ultrasound of the uterus demonstrates cystic spaces and larger irregular fluid collections (short arrows). No fetal parts are identified.
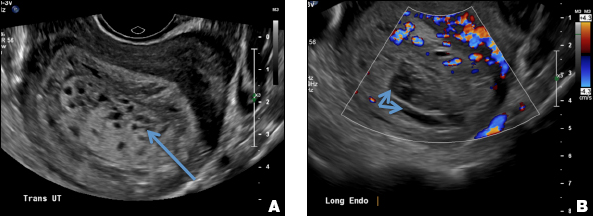
C) Enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). CORRECT
EMV is an extremely rare cause of postpregnancy hemorrhage most often seen secondary to iatrogenic causes but can also be congenital or acquired from excessive hormone stimulation.2 On ultrasound, EMV appears as a hypoechoic vascular lesion or serpiginous network of vessels located in the myometrium with increased velocity and low resistance waveform on spectral Doppler.4 Subinvolution of placental site implantation where there is failure of the vessels to involute can sometimes be indistinguishable from acquired EMV and occasionally difficult to differentiate from RPOC.1 In stable patients with equivocal ultrasound findings, magnetic resonance imaging (MRI) with its superior contrast resolution can help delineate the endometrium from myometrium and clearly identify EMV as serpiginous signal voids in the myometrium with avid enhancement following contrast.5 Computed tomography (CT) angiogram is also of value in both the diagnosis and pretreatment planning of EMV prior to transcatheter uterine artery embolization.
Enhanced myometrial vascularity (EMV) also known as arteriovenous malformation (AVM). A & B) Transvaginal ultrasounds of a uterus with Doppler demonstrate a serpiginous tangle of vessels located in the myometrium (long arrows) with increased velocity and low-resistance waveform on spectral Doppler. C) Transvaginal ultrasound of the uterus with Doppler in a different patient demonstrates a markedly vascular mass centered in the myometrium (short arrow) with low-resistance waveform. D) Axial arterial phase CT angiogram a few weeks later demonstrates multiple enhancing vessels in the uterus (arrowhead) arising from the uterine artery compatible with EMV.
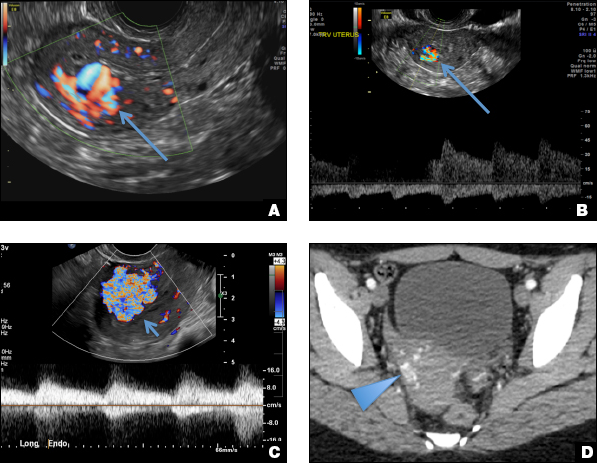
D) Endometritis INCORRECT
Endometritis is a common cause of fever and sepsis in the postpartum state, but it can also occur after procedures such as uterine fibroid embolization (UFE). On ultrasound, the endometrium usually is distended with avascular echogenic fluid. The presence of shadowing gas in the appropriate clinical setting is concerning for endometritis. CT scan can confirm the presence of gas and evaluate for septic thrombophlebitis, an uncommon, life-threatening complication of endometritis.
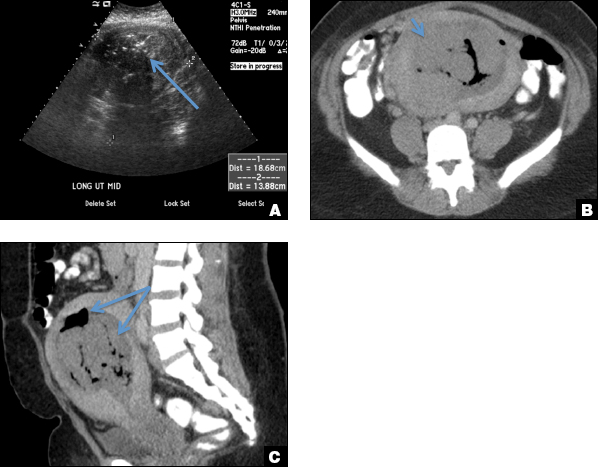
Endometritis. A) Transabdominal ultrasound of the uterus in a patient with fever and sepsis following UFE demonstrates echogenic fluid distending the endometrium with shadowing gas (long arrow). B & C) Axial and sagittal contrast-enhanced CT scans demonstrate an expanded endometrium filled with hyperdense material (short arrow) and large foci of gas (long arrows) consistent with endometritis.