As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
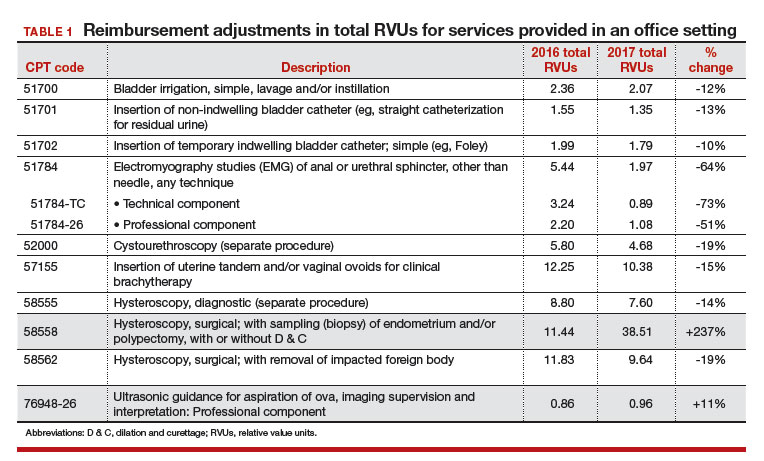
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
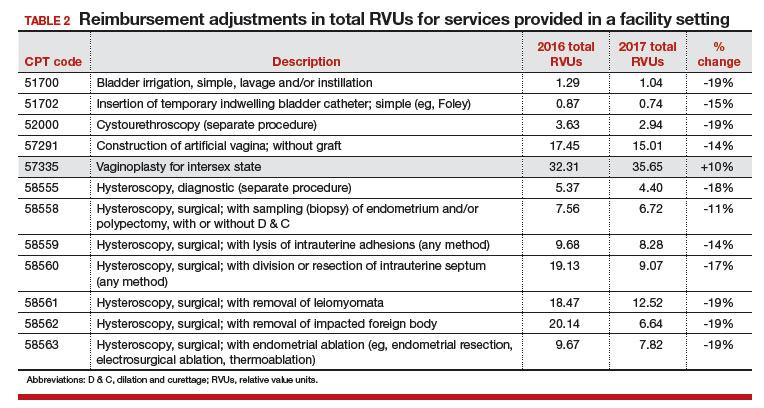
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.