Low malignant potential tumors of the ovary – otherwise known as borderline tumors – include ovarian tumors with atypical cellularity, which lack stromal invasion that differentiates them from low grade and high grade invasive carcinomas. They can coexist with extraovarian disease, however, in the setting of borderline tumors these foci are referred to as “implants” rather than metastases. As discussed below, these implants can exhibit the presence of invasion or not.
Classification
The two most common histologic categories of borderline tumors are serous and mucinous cell types. Rarer histologic types such as endometrioid, clear cell, and Brenner also exist. However, these are so infrequent that they will not be covered in this discussion as there are very limited data to make generalizations about these histologies.
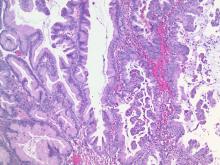
Serous borderline tumors contain cellularity similar to that of fallopian tubal epithelium. Approximately 25% of all serous ovarian tumors exhibit borderline features. Compared with mucinous tumors, they are more commonly bilateral and smaller in size (mean size of 12 cm) at the time of diagnosis and they are more likely to be associated with extraovarian implants (typically peritoneal). In fact, up to 25% of serous borderline tumors have concomitant extraovarian implants. Cancer antigen (CA) 125 is commonly a tumor marker for these tumors (elevated in 45% of early stage disease and 80% of advanced stage disease).1
Incidence
The incidence of borderline ovarian tumors is 2.5 per 100,000 woman years in the United States. About 70% are diagnosed at stage I.3 They arise in a younger population compared with invasive ovarian carcinomas. Risk factors for development of borderline tumors are similar to those of invasive ovarian carcinomas (such as nulliparity) but there may be a stronger association between the development of borderline ovarian tumors and infertility, as well as prior use of infertility treatment.4
Diagnosis
The diagnosis of borderline tumors of the ovaries occurs almost exclusively at the time of surgical pathology (either frozen section or definitive pathology).
Preoperative assessments with imaging and tumor markers – usually CA 125 and carcinoembryonic antigen (CEA) – are nonspecific for this tumor type. Preoperative imaging will typically reveal complex ovarian cysts with papillations and vascularity. However, in the case of mucinous borderline tumors, unilocular cysts are common.1 The presence of ascites and peritoneal implants can be observed on preoperative imaging of serous borderline tumors with extraovarian disease. However, it is not possible for this imaging to accurately differentiate borderline tumors with implants from low grade and high grade carcinomas with metastases.
Surgical management
Borderline tumors are commonly diagnosed in women of reproductive age and decisions need to be made regarding fertility sparing surgery, ovarian sparing surgery, and whether staging is performed. The recommended surgery for women who have completed child bearing is complete hysterectomy with bilateral salpingo-oophorectomy. However, cystectomy or unilateral salpingo-oophorectomy can be considered for women who desire fertility preservation. Conservative fertility preserving surgery is associated with an increased risk of recurrence, but with no negative impact on survival.1
Staging – with at least omentectomy and comprehensive evaluation of the peritoneal cavity, with or without peritoneal biopsies – can be considered, though staging is not associated with improved survival. Lymphadenectomy is also not associated with improved oncologic outcomes and routine lymphadenectomy is not recommended for borderline tumors.1 However, about a quarter of patients with gross evidence of extraovarian disease have implants within lymph nodes. Bulky lymph nodes should be removed, particularly in this group of patients.
Complete removal of extraovarian implants is the surgical intervention that is most important for survival and recurrence.1 This requires that surgeons thoroughly evaluate the peritoneal cavity and retroperitoneum, and possess the capability to completely resect all sites of disease.
Historically appendectomy was part of surgical staging of mucinous borderline tumors in order to identify a primary appendiceal lesion, but only 1% of patients with a grossly normal appearing appendix have significant pathology identified. This is no longer recommended.2
Treatment
The primary treatment for borderline tumors of the ovary is surgery. A minimally invasive approach is appropriate when feasible, though it may be associated with an increased risk of cyst rupture, particularly if cystectomy is attempted. Outcomes are best when extraovarian implants are completely resected. Adjuvant chemotherapy is not associated with improved survival and is not routinely recommended, though the guidelines from the National Comprehensive Cancer Network include this as an option for patients with advanced stage disease that is either completely or incompletely resected.5
Prognosis
In general, prognosis is excellent for borderline tumors with 5- and 10-year survival of 99% and 97%, 98% and 90%, and 96% and 88% for stages I, II and III tumors, respectively.1 However, several pathologic, molecular, and anatomic features are important in predicting who is at highest risk for recurrence.
Serous borderline tumors with invasive implants (as opposed to desmoplastic implants) and incompletely resected extraovarian implants are associated with increased recurrence and poor prognosis.Micropapillary features and stromal invasion are histologic features that have historically been associated with worse prognosis, but it is unclear if these are independent risk factors, or instead associated with invasive implants. For mucinous borderline tumors, intraepithelial carcinoma has been inconclusively associated with poor prognosis.1,6
Surveillance
Recurrences do occur in patients with a history of borderline tumors of the ovary, however these typically occur late. For this reason, surveillance is important and should continue for many years after diagnosis. Most recurrences are within the peritoneal cavity and are treated with surgical excision and patients should be counseled regarding symptoms of recurrence that include gastrointestinal symptoms, bloating, and pain.
In accordance with guidelines from the Society of Gynecologic Oncology, surveillance examinations can take place annually as there is no evidence that more frequent evaluations improve outcomes. These visits should include physical examinations (with pelvic examinations), symptom assessment, and, if elevated preoperatively, assessment of relevant tumor markers (typically CA 125 and/or CEA).7 Surveillance should continue for at least 10 years postoperatively.
Routine imaging is not recommended for all patients in surveillance. However, for patients who have had fertility-sparing surgery, imaging with pelvic ultrasound is recommended, particularly for women with a history of cystectomy or serous borderline tumor (who are at increased risk for bilateral tumors).
Women who have had fertility-sparing surgery should be considered for complete oophorectomy and hysterectomy after they have completed childbearing, as incomplete surgeries are associated with an increased risk for recurrence.7 Prognosis is most closely associated with the presence of invasive implants and residual disease following surgery. Surgeons who manage these tumors can safely consider fertility-sparing procedures but should be equipped to completely resect all gross disease.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She reported having no relevant financial disclosures.
References
1. Lancet Oncol. 2012 Mar;13(3):e103-15.
2. Arch Gynecol Obstet. 2016 Nov;294(6):1283-9.
3. Cancer. 2002 Dec 1;95(11):2380-9.
4. Am J Epidemiol. 2002 Feb 1;155(3):217-24.
5. J Natl Compr Canc Netw. 2016 Sep;14(9):1134-63.