NEW ORLEANS – The National Cancer Institute is woefully underfunding gynecologic cancer research, compared with several other cancer types, when the money the institute is spending annually is factored by the incidence and lethal impact of each cancer using U.S. data from 2007 to 2014.
That period featured “systematic and pervasive underfunding of gynecologic cancers in relation to other cancer sites,” Ryan J. Spencer, MD, said at the annual meeting of the Society of Gynecologic Oncology. The trends over the period he studied worsened with time and pose the risk that progress in gynecologic cancers – uterine, cervical, and ovarian – will “lag behind” other cancers’ progress in prevention, treatment, and improved survival, said Dr. Spencer, a gynecologic oncologist at the University of Wisconsin–Madison.
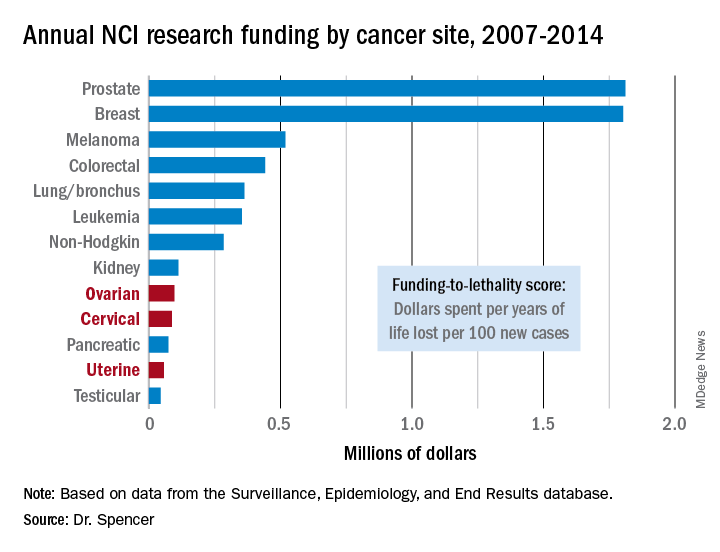
To quantify the funding challenges that these three gynecologic cancers have experienced, Dr. Spencer and his associates first calculated a lethality factor for them and 10 other cancer types based on 2014 incidence and mortality data from the Surveillance, Epidemiology, and End Results database maintained by the National Cancer Institute. For example, ovarian cancer had a mortality-to-incidence ratio of 0.636. They then multiplied this by the average person-years of life lost from death attributable to ovarian cancer, 17.5 years, which calculated to about 11 years of life lost for each new case, or 1,100 years of life lost for every 100 new cases of ovarian cancer. Finally, they used this calculated value for each cancer type to divide the amount of money spent by the NCI each year during 2007-2014 to fund research into each of the 13 cancer types to derive an amount spent per year of life lost per 100 new cases, a statistic Dr. Spencer called the funding-to-lethality score.In 2014, the NCI alloted about $92 million for research funding for ovarian cancer, which resulted in a funding-to-lethality score of about $83,000 per year of life lost per 100 new cases. When averaged for the entire 2007-2014 period, the funding-to-lethality score for ovarian cancer was $97,000 per year of life lost per 100 new cases, $87,000 for cervical cancer, and $57,000 for uterine cancer. These levels ranked these cancers as numbers 9, 10, and 12, respectively, in the standings for NCI research dollars spent relative to lethality. In contrast, prostate and breast cancer stood at the top of the list, with funding-to-lethality scores of $1.8 million each, followed by melanoma with a funding-to-lethality score of $519,000 per year of life lost for every 100 new cases. The lowest-funded cancer, in thirteenth place, was testicular, with $44,000 per year of life lost per 100 new cases.Additional time trend analyses showed that the annual funding-to-lethality score for each of the three gynecologic cancers declined during the period studied.
“We must do everything we can to reverse these trends,” Dr. Spencer concluded.
SOURCE: Spencer R et al. SGO 2018, Abstract 3.