Our process for office-based uterine aspiration
We follow the step-by-step process outlined below for performing office-based uterine aspiration. Clinicians should review their clinic’s protocols prior to implementing such a plan.
Review the patient history and pregnancy dating. Patients with serious medical conditions, such as history of postabortion hemorrhage or a bleeding disorder, may not be appropriate candidates for an office-based procedure. We perform bedside ultrasonography to confirm pregnancy dating and diagnosis of pregnancy failure.
Review consent for the procedure and sedation. Risks of office-based uterine aspiration are the same as those for D&C: bleeding, uterine perforation, and failure to fully evacuate the uterus. Benefits include rapid, safe evacuation of the pregnancy. Alternative treatments include expectant or medical management.
For pain management, we start by discussing expectations with the patient. Providing general anesthesia in the outpatient setting is not safe; many women are satisfied, however, with local anesthesia with or without sedation.
Local anesthesia may be given using a paracervical block with 2 mL of 1% lidocaine at the tenaculum site followed by 18 mL divided between the 4 and 8 o’clock positions. In our practice, we are trained providers of conscious sedation, so additionally we offer IV fentanyl 100 μg and IV midazolam 2 mg given prior to the procedure.
Provide antibiotic prophylaxis. The American College of Obstetricians and Gynecologists and the Society for Family Planning recommend doxycycline 200 mg orally as a preoperative prophylaxis for office-based uterine aspiration.14,15 Metronidazole is an acceptable alternative for patients who have medication allergies.
Prepare the surgical field. To complete this procedure, you will need the following equipment:
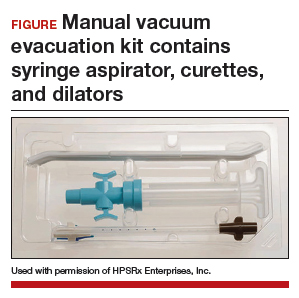
- one MVA kit that includes an aspirator, curettes, and dilators (FIGURE)
- 20 mL 1% lidocaine, divided into two 10-mL syringes with a 22-gauge 3.5-inch spinal needle
- speculum
- cervical antiseptic prep
- single-tooth tenaculum
- ring forceps.
Perform the MVA procedure. A full description of how to perform the MVA procedure using the Ipas MVA Plus Aspirator device is available online at http://provideaccess.org/wp-content/uploads/2012/09/4Performing-MVA-Us ing-the-Ipas-MVA-Plus.pdf.
A good option for many women
A D&C in the OR remains an appropriate option for patients who are clinically unstable due to heavy vaginal bleeding. With highly sensitive home urine pregnancy tests, pregnancies often are diagnosed before clinically apparent miscarriage. In fact, many such patients are diagnosed with pregnancy failure in the office, as was our patient in the case scenario. For such women, office-based management of early pregnancy failure is preferred because it is safe, cost-effective, and patient centered.
The “Break This Practice Habit” series is spearheaded by Dr. Lauren Demosthenes, who makes overarching high value cost decisions in her role as Medical Director of High Value Care and Innovation, Department of ObGyn at Greenville Health System in Greenville, South Carolina. Watch for quarterly case presentations of low value, low evidence practices that should be questioned in current day, followed by reasons why that practice should be abandoned. If you would like to contribute to this series, please submit your query to Dr. Demosthenes at ldemosthenes@mdedge.com.