Approaches to managing the OP position
First stage of labor
Identification of a cephalic-presenting fetus in the OP position in the first stage of labor might warrant increased attention to fetal position in the second stage of labor, but does not usually alter management of the first stage.
Second stage of labor
If an OP position is identified in the second stage of labor, many obstetricians will consider manual rotation of the fetal occiput to an anterior pelvic quadrant to facilitate labor progress. Because a fetus in the OP position may spontaneously rotate to the OA position at any point during the second stage, a judicious interval of waiting is reasonable before attempting a manual rotation in the second stage. For example, allowing the second stage to progress for 60 to 90 min in a nulliparous woman or 30 to 60 min in a multiparous woman will permit some fetuses to rotate to the OA position without intervention.
If the OP position persists beyond these time points, a manual rotation could be considered. There are no high-quality clinical trials to support this maneuver,12 but observational reports suggest that this low-risk maneuver may help reduce the rate of CD and anal sphincter trauma.13-15
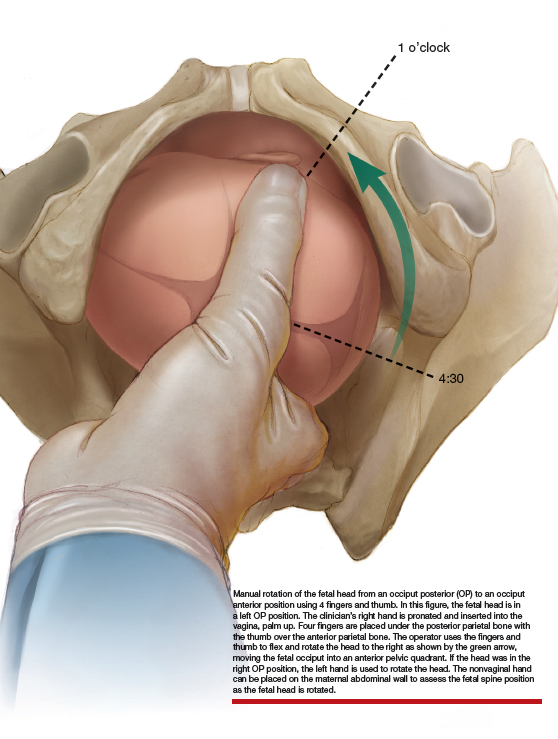
Manual rotation from OP to OA. Prior to performing the rotation, the maternal bladder should be emptied and an adequate anesthetic provided. One technique is to use the 4 fingers of the hand as a “spatula” to turn the head. If the fetus is in a left OP position, the operator’s right hand is pronated and inserted into the vagina, palm up. Four fingers are placed under the posterior parietal bone with the thumb over the anterior parietal bone (ILLUSTRATION).4 The operator uses the fingers and thumb to flex and rotate the head to the right, moving the fetal occiput into an anterior pelvic quadrant.4 If the head is in the right OP position, the left hand is used to rotate the head. The nonvaginal hand can be placed on the maternal abdominal wall to assess the fetal spine position as the fetal head is rotated. The fetal head may need to be held in the anterior pelvic quadrant during a few maternal pushes to prevent the head from rotating back into the OP position.
Approaching delivery late in the second stage
If the second stage has progressed for 3 or 4 hours, as in the case described above, and the fetus remains in the OP position, delivery may be indicated to avoid the maternal and fetal complications of an even more prolonged second stage. At some point in a prolonged second stage, expectant management carries more maternal and fetal risks than intervention.
Late in the second stage, options for delivery of the fetus in the OP include: CD, rotational forceps delivery, direct forceps delivery from the OP position, and vacuum delivery.
Cesarean delivery. CD of the fetus in the OP position may be indicated when the fetus is estimated to be macrosomic, the station is high (biparietal diameter palpable on abdominal examination), or when the parturient has an android pelvis (narrow fore-pelvis and anterior convergence of the pelvic bone structures in a wedge shape). During CD, if difficulty is encountered in delivering the fetal head, a hand from below, extension of the uterine incision, or reverse breech extraction may be necessary to complete the delivery. If the clinical situation is conducive to operative vaginal delivery, forceps or vacuum can be used.
Continue to: Rotational forceps delivery...