- Comprehensive surgical staging is an integral part of treatment of early-stage endometrial cancer.
- Standard surgical staging includes exploratory laparotomy, complete inspection of the abdomen and pelvis, biopsies of suspicious areas, total abdominal hysterectomy, bilateral salpingo-oophorectomy, and lymph-node sampling.
- The extent of lymph-node sampling, the appropriate adjuvant therapy, and the use of laparoscopy are the major areas of controversy in the management of early-stage endometrial cancer.
- Concerns that hormone replacement therapy may increase the likelihood of endometrial cancer recurrence have not yet been adequately explored by randomized trials.
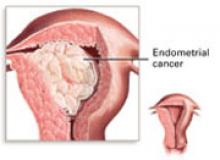
Approximately 39,300 new cases of endometrial cancer were diagnosed in 2002, and the disease is the sixth most common cause of cancer deaths in women. While the mortality rate has declined by more than half since 1940, the disease still caused an estimated 6,600 deaths in 2002. The lifetime risk of being diagnosed with endometrial cancer is approximately 2.7%, and the median age at diagnosis is 65 years. Almost three quarters of cases are diagnosed before the disease has spread outside the uterus. The overall 5-year survival rate for all stages of endometrial cancer is 86%, with disease confined to the uterus having a 97% 5-year survival rate.1
Preoperative intracavitary radiation treatment of endometrial cancer has fallen out of favor since it was found to lead to a loss of important diagnostic and prognostic information (including depth of myometrial invasion), possible overtreatment of early lesions, and a delay of definitive surgical therapy in situations of possible lymph-node metastases.2 Currently, comprehensive surgical staging is an integral part of the treatment of early-stage endometrial cancer.
Surgical staging
Prior to 1988, endometrial cancer was staged according to a universal clinical staging system, which has since proved to be frequently inaccurate (TABLE 1). The staging system changed to comprehensive surgical staging after several studies showed that information obtained intraoperatively is an important indicator of prognosis and survival (TABLE 2).3-5 These factors include depth of myometrial invasion, tumor grade, cervical involvement, peritoneal cytology, adnexal metastases, vascular space invasion, and lymph-node status.
The standard surgical staging procedure involves an exploratory laparotomy, complete inspection of the abdomen and pelvis, biopsies of any suspicious areas on the peritoneal or intestinal surfaces, abdominal and pelvic washings, total abdominal hysterectomy, bilateral salpingo-oophorectomy, and selected pelvic and para-aortic lymph-node sampling. Omental sampling generally should be performed in patients with serous or clear-cell histology. In these high-risk histologic subtypes, complete surgical staging should be performed even for patients with superficial or no myometrial invasion, as the risk of lymph node metastases is 30% to 50%.6
TABLE 1
Corpus cancer clinical staging, International Federation of Gynecology and Obstetrics (FIGO), 1971
| STAGE | CHARACTERISTICS |
|---|---|
| I | Carcinoma is confined to the corpus |
| IA | Length of the uterine cavity is 8 cm or less |
| IB | Length of the uterine cavity is more than 8 cm |
| Histologic subtypes of adenocarcinoma: | |
| G1 | Highly differentiated adenomatous carcinoma |
| G2 | Differentiated adenomatous carcinoma with partly solid areas |
| G3 | Predominantly solid or entirely undifferentiated carcinoma |
| II | Carcinoma involves the corpus and cervix |
| III | Carcinoma extends outside the uterus but not outside the true pelvis |
| IV | Carcinoma extends outside the true pelvis or involves the bladder or rectum |
TABLE 2
Corpus cancer surgical staging, International Federation of Gynecology and Obstetrics (FIGO), 1988
| STAGE | CHARACTERISTICS |
| IA, G123 | Tumor limited to the endometrium |
| IB, G123 | Invasion to less than half the myometrium |
| IC, G123 | Invasion to more than half the myometrium |
| IIA, G123 | Endocervical glandular involvement only |
| IIB, G123 | Cervical stromal invasion |
| IIIA, G123 | Tumor invades serosa or adnexae or positive peritoneal cytology |
| IIIB, G123 | Vaginal metastases |
| IIIC, G123 | Metastases to pelvic or para-aortic lymph nodes |
| IVA, G123 | Tumor invades bladder and/or bowel mucosa |
| IVB | Distant metastases including intra-abdominal and/or inguinal lymph node |
| Histopathology: degree of differentiation* | |
| G1 | 5% or less of a nonsquamous or nonmorular solid growth pattern |
| G2 | 6% to 50% of a nonsquamous or nonmorular solid growth pattern |
| G3 | More than 50% of a nonsquamous or nonmorular solid growth pattern |
| * Cases should be grouped by the degree of differentiation of the adenocarcinoma. | |
| Notes on pathologic grading: | |
| Notable nuclear atypia inappropriate for the architectural grade raises a grade 1 or grade 2 tumor by 1 grade. | |
| In serous adenocarcinomas, clear-cell adenocarcinomas, and squamous-cell carcinomas, nuclear grading takes precedence. | |
| Adenocarcinomas with squamous differentiation are graded according to the nuclear grade of the glandular component. | |
| Rules related to staging: | |
| Because corpus cancer is now surgically staged, procedures previously used for determination of stages are no longer applicable, such as the finding of fractional dilatation and curettage to differentiate between Stages I and II. | |
| There may be a small number of patients with corpus cancer who will be treated primarily with radiation therapy. If that is the case, the clinical staging adopted by FIGO in 1971 would still apply, but designation of that staging system would be noted. | |
| Ideally, width of the myometrium should be measured, along with the width of tumor invasion. | |