Sequelae of major perineal laceration can be severe
Major perineal laceration occurs in approximately 2% to 20% of vaginal deliveries in the United States. The principal risk factors for third- and fourth-degree lacerations are nulliparity, midline episiotomy, and operative vaginal delivery, especially forceps extraction. Both types of laceration may lead to serious morbidity, such as prolonged pain, fecal incontinence, and perineal infection, including necrotizing fasciitis. These infections typically are polymicrobial, mixed aerobic–anaerobic. Moreover, fourth-degree lacerations may result in rectovaginal fistula if they are not repaired properly. This complication causes considerable debility and major social inconvenience for the patient.
Although the sample size was relatively small, this study clearly demonstrated that a single dose of extended-spectrum cephalosporin (cefotetan or cefoxitin) was highly effective in reducing the rate of perineal infection and perineal wound disruption. Whether a more limited-spectrum agent such as cefazolin would be as effective is not certain.
I strongly recommend routine antibiotic prophylaxis for any patient who sustains a third- or fourth-degree perineal laceration.
If the patient has a mild allergy to penicillin (morbilliform rash), I would administer cefotetan because it is less expensive than cefoxitin. If the patient has a severe reaction to penicillin (urticaria, anaphylaxis), I would administer both clindamycin and gentamicin in order to ensure adequate coverage of the multiple organisms likely to cause soft-tissue infection of the genital tract.
Clindamycin alone covers only aerobic gram-positive cocci and offers no protection against the coliform organisms that are so prevalent in perineal wound infection.8
Diarrhea linked to Clostridium difficile emerges as a potent threat to pregnant women
Rouphael NG, O’Donnell JA, Bhatnagar J, et al. Clostridium difficile-associated diarrhea: an emerging threat to pregnant women. Am J Obstet Gynecol. 2008;198:635.e1–635.e6 [Classification of evidence – Level III].
This report describes 10 cases of severe Clostridium difficile-associated diarrhea (CDAD) in pregnant women during 2005 and 2006. CDAD usually affects elderly debilitated patients in hospitals and nursing homes. This report is of great concern because the affected patients were otherwise healthy, young, pregnant women. The observations are even more alarming because the mortality rate in this small series was 30% for both mothers and babies.
Details of the series
The women developed signs of severe CDAD 3 to 60 days after receiving antibiotics; the median was 5 days. CDAD was considered severe if the patient required hospitalization, ICU admission, or colectomy, or if she died. These cases occurred in California, Georgia, Oklahoma, and Pennsylvania and were reported to the Centers for Disease Control and Prevention (CDC).
Six women became ill before delivery, and four developed symptoms postpartum. The most common manifestations of infection were diarrhea, abdominal pain and distention, and fever. The peripheral white blood cell count was in the range of 11–72 × 103/μL. In nine patients, the diagnosis was confirmed by a positive test for toxin A/B; seven of these patients also had visible pseudomembranes in the colon. One patient had a positive stool sample for C difficile ( FIGURE 2 ).
Six patients required admission to the ICU. Six developed toxic megacolon, and five required subtotal colectomy. Three had sepsis; three had acute renal failure; two had disseminated intravascular coagulation. Three patients died, and three had stillbirths. Two patients relapsed following treatment.
One patient had no treatment and died. The others received either metronidazole or vancomycin or a combination of the two. One of the patients who died received metronidazole, vancomycin, and cholestyramine.
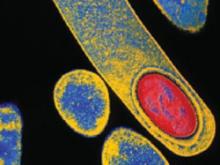
FIGURE 2 Clostridium difficile
C difficile is a spore-forming, gram-positive anaerobic bacillus that is a common cause of antibiotic-associated diarrhea.
An epidemic strain appears
The incidence of C difficile infection in acute care US hospitals has increased to 84 for every 100,000 patients in recent years, about three times the rate of 31 for every 100,000 that was reported in 1996, as the authors note. Many of the most severe cases of CDAD are caused by a new epidemic strain of bacteria, termed North American Pulsed Field type 1 (NAP1) and PCR ribotype 027.
This new strain is characterized by three key virulence factors:
- increased production of toxins A and B
- resistance to fluoroquinolones
- production of binary toxin.
Toxins A and B bind to the surface of intestinal epithelial cells, stimulate tissue injury and inflammation, and, ultimately, lead to cell death. Binary toxin appears to act synergistically with toxins A and B to cause severe colitis.9
Metronidazole is no longer the treatment of choice for severe CDAD
Before 2000, treatment of CDAD with vancomycin or metronidazole was 97% to 98% effective.9 In recent years, however, a failure rate as high as 26% has been reported among patients who are treated with metronidazole.10 One prospective, randomized clinical trial demonstrated that, in patients who had severe CDAD, vancomycin, 125 mg four times daily, was superior to metronidazole, 250 mg four times daily (97% success rate vs 76%; p=.02).11 The efficacy of the two drugs was comparable in treating milder cases of CDAD (98% for vancomycin, 90% for metronidazole; p=.36).