Is histologic analysis of a polyp sufficient risk assessment?
Rahimi S, Marani C, Renzi C, Natale ME, Giovannini P, Zeloni R. Endometrial polyps and the risk of atypical hyperplasia on biopsies of unremarkable endometrium: a study on 694 patients with benign endometrial polyps. Int J Gynecol Pathol. 2009;28(6):522–528.
This study involved 694 consecutive patients who had benign endometrial polyps. Investigators sought to clarify the relationship between polyps and the underlying endometrium—specifically, to determine whether a polyp is a “circumscribed pathology of the endometrium or a polypoid expression of endometrial hyperplasia.” In describing the rationale for the study, the authors observe that the association between polyps and premalignant and malignant changes remains unclear.
Participants underwent hysteroscopy for removal of the polyps, at which time two biopsies of “unremarkable” endometrium, far from the base of the polyp, were also obtained.
Overall, endometrial hyperplasia without atypia was identified on hysteroscopically unremarkable endometrium in 18% of women, and atypia was identified in 7.3%. Among postmenopausal women, hyperplasia without atypia was identified in 21.6% of cases, atypia in 12%, and adenocarcinoma in 1.2%.
Multivariable analysis revealed that postmenopausal women who had polyps heavier than 1 g were 3.6 times more likely to have atypia (95% CI, 1.3–10.3). Among premenopausal women, the likelihood of atypia increased when the polyp weighed more than 0.4 g (odds ratio [OR], 3.5; 95% CI, 1.1–10.9) or the patient was older than 40 years (OR, 3.82; 95% CI, 1.1–13.2).
Endometrial lesions are not always evident at the time of hysteroscopy. Therefore, when evaluating an endometrial lesion such as a polyp, combine hysteroscopy with histopathologic assessment of the background endometrium (by means of a pipelle or curette), especially in women who have high-risk characteristics such as menopausal status or large polyps.
They’re accessible in the OBG Management Video Library at obgmanagement.com

VIDEO 1: Saline-infusion sonographic imaging of a polyp

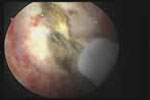
VIDEO 2: Hysteroscopic imaging of a polyp in a menopausal patient. A flexible 3-mm scope is used to assess an asymptomatic menopausal woman in whom an enlarged endometrial stripe was identified during earlier imaging.

VIDEO 3: Hysteroscopic imaging of a polyp and associated hyperplasia. A flexible 3-mm scope is used to evaluate a menopausal women who has uterine bleeding, revealing a 2-cm polyp.

VIDEO 4: Office polypectomy. An 8-mm, apparently benign polyp is removed from a premenopausal woman using continuous-flow operative hysteroscopy in an office setting.
VIDEO 5: Removal of a large polyp. A large (2 cm x 2.5 cm) polyp is removed in pieces, with the polyp partially attached to the endometrial wall, from a premenopausal woman who has abnormal bleeding.
More: Watch Dr. Brent Seibel perform OR-based hysteroscopic polypectomy


