6. Avoid general anesthesia
Use neuraxial anesthesia for labor and delivery in eclampsia
Turner JA. Severe preeclampsia: anesthetic implications of the disease and its management. Am J Ther. 2009;16(4):284–248.
Huang CJ, Fan YC, Tsai PS. Differential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo Cesarean delivery: a population-based study. Br J Anaesth. 2010;105(6):818–826.
Epidural, spinal, or combined anesthesia is safe in the absence of coagulopathy or severe thrombocytopenia. General anesthesia increases the risk of aspiration, failed intubation due to pharyngolaryngeal edema, and stroke secondary to the increase in systemic and intracerebral pressures during intubation and extubation.
Eclampsia is not an indication for cesarean delivery
Repke JT, Sibai BM. Preeclampsia and eclampsia. OBG Manage. 2009;21(4):44–55.
Once the mother has been resuscitated and stabilized, the provider should choose a mode of delivery that is based on fetal condition, gestational age, presence or absence of labor, and the cervical Bishop score. Vaginal delivery can be achieved in most patients who have a gestational age of 34 weeks or greater.
8. Late presentation happens
Be aware that eclampsia can develop for the first time as long as 28 days postpartum
Sibai BM, Stella CL. Diagnosis and management of atypical preeclampsia-eclampsia. Am J Obstet Gynecol. 2009;200(5):481.e31–37.
Atypical eclampsia is any eclampsia that develops beyond 48 hours postpartum. A history of diagnosed predelivery preeclampsia is not necessary for development of late postpartum eclampsia. In general, more than 50% of patients who develop late postpartum eclampsia have no evidence of preeclampsia prior to delivery.
Be aware that the clinical and neuro-imaging features of eclampsia overlap with those of reversible cerebral vasoconstriction syndrome (angiopathy)
Fletcher JJ, Kramer AH, Bleck TP, Solenski NJ. Overlapping features of eclampsia and postpartum angiopathy. Neurocrit Care. 2009;11(2):199–209.
Women who have reversible cerebral vasoconstriction syndrome have clinical findings (acute onset of recurrent headaches, visual changes, seizures, and hypertension) and cerebral magnetic resonance imaging (MRI) findings (posterior reversible encephalopathy syndrome) that are similar to those of women who have late postpartum eclampsia (FIGURE). However, in women who have postpartum cerebral angiopathy, cerebral angiography will show the presence of bead-like vasoconstriction—which is usually absent in eclampsia.
Posterior reversible encephalopathy syndrome
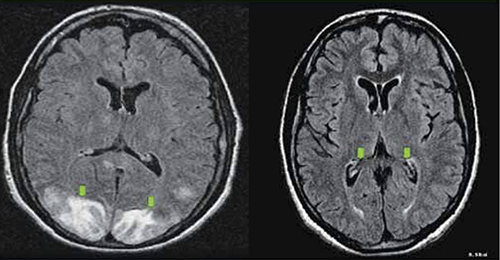
Green arrows point to vasogenic edema in the occipital lobes and, partially, the parietal lobes. The edema is gone on repeat magnetic resonance imaging (see Recommendation #9).
10. Act today, see a better outcome tomorrow
Avoid long-term maternal neurologic injury by managing eclampsia properly
Zeeman GG. Neurologic complications of preeclampsia. Semin Perinatol. 2009;33(3):166–172.
Residual neurologic damage is rare in the majority of women who have eclampsia. However, long-term cerebral white-matter injury (cytotoxic edema, infarction) on MRI imaging and impaired memory and cognitive function may develop in some women who have multiple seizures and who have inadequately controlled persistent severe hypertension.
We want to hear from you! Tell us what you think.


