Nevertheless, multiple gestation is sufficiently problematic that we recommend some strategies to reduce its incidence:
- Use low-dosage gonadotropin stimulation with careful monitoring, and limit the number of follicles that are roughly 15 mm or larger to two in patients 37 years of age or younger; three in patient 38 to 40 years old; and more in patients older than 40
- Develop specific cancellation criteria, which should be explained to and accepted by patients undergoing controlled ovarian stimulation. Gonadotropin-releasing hormone (GnRH) antagonists may be of benefit.1
- When clomiphene citrate stimulates the development of two or more mature follicles, outcomes do not differ from those obtained with controlled ovarian stimulation using gonadotropins and intrauterine insemination (IUI).2 Therefore, a reasonable strategy in many patients is to consider initiating treatment with clomiphene citrate and IUI and to proceed directly to in vitro fertilization (IVF) when treatment fails, thereby avoiding controlled ovarian stimulation altogether.3
- Pre-ovulatory ultrasonography-guided aspiration of excess follicles to reduce the risk of multiple gestation has potential benefit but needs further study.
Overall, regardless of the medication or regimen employed, it may not be possible to entirely eliminate the risk of multiple gestation associated with ovulation induction or controlled ovarian stimulation.
When to consider gestation reduction
High-order multifetal gestation reduction has been utilized as a strategy to reduce complications associated with ovulation induction and controlled ovarian stimulation, but use of this technology must be regarded as an adverse outcome of infertility treatment. Overall, data suggest that multifetal gestation reduction is associated with a reduced risk of prematurity, although its true benefit is difficult to elucidate due to potential bias in the interpretation of data. A small percentage of patients lose the entire pregnancy, and the procedure can present patients with a profound ethical dilemma and psychological trauma. Thorough counseling is imperative.
Despite feelings of loss and guilt that persist for a year or longer, most patients report that they would make the decision to undergo gestation reduction again if a similar situation arose in the future.4
The procedure should be performed only in a specialized center by an experienced practitioner.
When performing ovulation induction and controlled ovarian stimulation, use the lowest dose of drug necessary to obtain a single mature follicle in anovulatory women, two follicles in young ovulatory women, and three follicles in women 38 to 40 years old. Because of the high risk of multiple gestation associated with controlled ovarian stimulation followed by IUI, consider moving directly to IVF after use of clomiphene citrate and IUI.
Practice Committee of the Society for Assisted Reproductive Technology and Practice Committee of the American Society for Reproductive Medicine. Elective single-embryo transfer [published online ahead of print December 22, 2011]. Fertil Steril. doi:10.1016/j.fertnstert.2011.11.050.
As IVF implantation rates have improved, the practice of transferring multiple embryos has resulted in a much-increased pregnancy rate but also a high percentage of multiple gestations. Elective single embryo transfer (eSET) has been advocated as the only effective means to avoid multiple pregnancy in IVF cycles, but there is significant concern that it might ultimately reduce the pregnancy rate.
ASRM recently published a Practice Committee Opinion that offers guidance for patient selection and describes barriers to eSET. Patient selection is critical.
Utilization of eSET in the United States has increased over the past decade but still lags behind other countries. Use of double embryo transfer (DET) has increased, significantly reducing the likelihood of high-order multiple pregnancies associated with ART but producing no change in the twin pregnancy rate (FIGURE). Randomized, controlled trials and other studies have demonstrated that the cumulative pregnancy rate per retrieval is no different for eSET followed by frozen embryo transfer than it is for DET in properly selected patients.
Most transfers involve two embryos
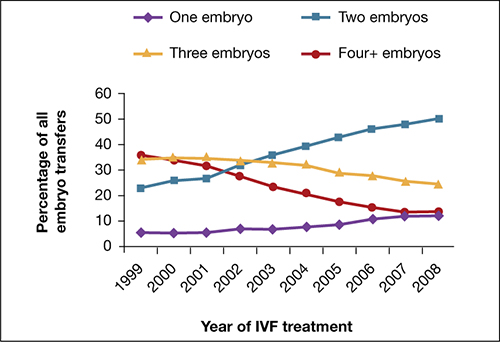
Percentage of transfer of one, two, three, or four or more embryos among all in vitro fertilization cycles performed in the United States, 1999–2008.
SOURCE: ASRM. Reproduced with permission.eSET is most appropriate for women who have a good prognosis:
- age younger than 35 years
- >1 top-quality embryo available for transfer
- first or second treatment cycle
- prior successful IVF
- recipients of embryos from donated eggs.
Women 35 to 40 years old can be considered for eSET if they have top-quality, blastocyst-stage embryos available for transfer.
Barriers to eSET include a lack of provider and patient education about it, financial considerations, embryo selection, and successful cryopreservation. When insurance coverage or refund guarantees are available, patient acceptance of eSET increases.



