Contraceptive mandate triggers a firestorm
On February 10, 2012, under pressure from religious groups, the Obama Administration offered a religious exemption to the contraception mandate for certain employers and group health plans. Under this “accommodation,” certain religious employers are exempt from the requirement to cover contraceptive services in their group health plans. An employer qualifies for this exemption if it:
- has the inculcation of religious values as one of its purposes
- primarily employs individuals who share its religious tenets
- primarily serves individuals who share its religious tenets, and
- qualifies for nonprofit status under
Internal Revenue Service (IRS) rules. At the same time that the Obama Administration wanted to accommodate employers’ religious beliefs, it also wanted to ensure that every woman would have access to free preventive care, including contraceptive services, regardless of where she works. And so while the Administration requires insurers to offer group health plan coverage without contraceptive coverage to religious-affiliated organizations, it also requires insurers to provide contraceptive coverage directly to individuals covered under the organization’s group health plan with no cost sharing.
This contraceptive mandate—even with the accommodation—has set off a firestorm on Capitol Hill that will eventually be settled in the courts.
Medicaid expansion falls short of original goal
In National Federation of Independent Business v. Sebelius, the plaintiffs asked the Supreme Court to rule on the federal government’s authority to require states to expand their Medicaid programs. Medicaid costs are typically shared by the federal and state governments. Under the ACA, state Medicaid programs were required to cover nearly all individuals who have incomes below 133% of the federal poverty level—$30,656 for a family of four in 2012—paid entirely by the federal government from 2014 through 2016. After that, the federal share gradually declines to, and then stays at, 90%. States that did not expand their Medicaid programs risked losing all federal Medicaid funding.
The Court ruled that the federal government can expand Medicaid but can’t penalize states that don’t accept the expansion mandate—effectively turning the mandate into a state option. States will receive the additional federal funds if they expand coverage, but states that don’t expand will not be penalized by losing existing federal funds for other parts of the program.
Since the ruling, a number of governors have announced that they will not expand their Medicaid programs, including governors of Florida and Louisiana. Those two states alone are home to 20% of all individuals intended to be covered under the Medicaid expansion.
This part of the ACA is particularly important to women because it strikes, for the first time, the requirement that a low-income woman must be pregnant to receive Medicaid coverage.
The figure below shows the dramatic potential improvement in coverage for women if all states fully implement the Medicaid expansion. Time, court decisions, elections, and state budget fights will determine how much of this change is realized for women’s health.
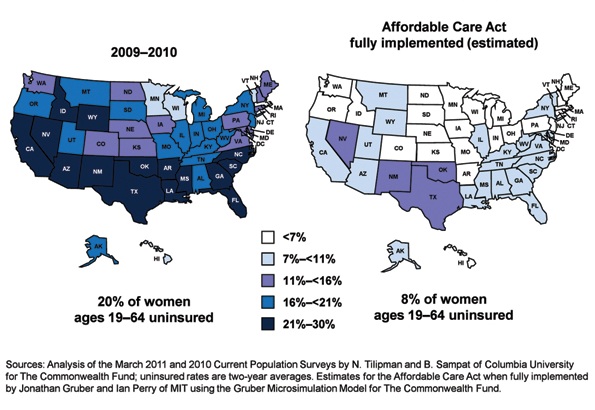
Percentage of insured women will increase under ACA
Percentage of women aged 19 to 64 years who were uninsured in 2009–2012 and under the Affordable Care Act when fully implemented.
SOURCE: Commonwealth Fund. Analysis of the March 2011 and 2010 Current Population Surveys by N. Tilipman and B. Sampat of Columbia University.
Women gain direct access to ObGyns
The ACA guarantees women in all states and all plans direct access to their ObGyns. Before the ACA, women in nine states lacked this guarantee, and women in 16 other states had only limited direct access. Now, a woman can go directly to her ObGyn without having to get a referral from her primary care physician or insurer.
Direct access is especially important because the ACA establishes new delivery systems, such as medical homes and accountable care organizations, designed to capture patients to maximize savings. An ObGyn does not have to be the patient’s primary care provider, and the patient’s access to her ObGyn cannot be limited to a certain number of visits or types of services.
ACA encourages states to cover family-planning services
Under the ACA, states have an easier time covering family-planning services, up to the same eligibility levels as pregnant women. Family planning is still an optional service that a state can choose to extend to women who have incomes above the Medicaid income eligibility level but, before the ACA was enacted, states had to apply to HHS for permission to waive the federal rules, often a very cumbersome process.
Prior to the ACA, 27 states had family planning waivers to provide services to nonpregnant women who had incomes above the Medicaid eligibility level—most at or near 200% of poverty. Now, states can provide family planning services to this population without federal approval.


