Polyps may also affect fertility
Rackow and coworkers demonstrated that endometrial polyps affect uterine receptivity on the molecular level, suggesting a relationship between endometrial polyps and infertility. And after a systematic review of endometrial polyps in women who had subfertility, Afifi and colleagues concluded that polypectomy can improve fertility, especially when assisted reproductive technologies are planned.
Myomas, polyps also contribute to bleeding abnormalities
Submucosal myomas have been associated with bleeding abnormalities, such as heavy menstrual bleeding and menopausal bleeding. Although the precise mechanism is unknown by which these bleeding abnormalities arise in the presence of submucosal fibroids, abnormalities within the endometrium or myometrium may play a role at the genetic and molecular level.7,8 There is clear evidence supporting hysteroscopic removal of submucosal fibroids to improve bleeding abnormalities.9,10
Hysteroscopic removal of eSge type 0 and type i submucosal myomas improves the pregnancy rate for patients who have otherwise unexplained primary infertility. Removal of endometrial polyps is also recommended to improve fertility.
Besides improving fertility, hysteroscopic removal of submucosal myomas and endometrial polyps improves menorrhagia and irregular and abnormal uterine bleeding.
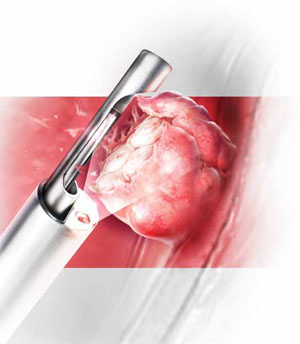
Hysteroscopic morcellators offer advantages over traditional resectoscopy, making hysteroscopic myomectomy of Type 0 and Type I myomas safer and more feasible for gynecologic surgeons. They allow resection using saline, operate without electrical energy, and utilize vacuum suction to remove tissue fragments from the uterine cavity.
Hysteroscopic morcellators ease the task of myomectomy
Hysteroscopic removal of submucosal myomas and polyps is an effective treatment for women who experience bleeding abnormalities or infertility, but the potential for complications deters many gynecologists from performing resectoscopic myomectomy.
Use of a monopolar loop electrode (VIDEO 1) requires an electrolyte-free distention medium, such as 1.5% glycine or 3% sorbitol, and intravasation of these fluids must be limited to minimize the risk of complications such as hyponatremia, cardiovascular compromise, cerebral edema, and, even, death.12 Although the use of normal saline with bipolar resectoscopic instrumentation (VIDEO 2) and automated fluid-management systems reduces the risk of fluid overload, it does not eliminate it entirely, and fluid balance must be carefully scrutinized.13
Intrauterine electrosurgery can burn pelvic organs if an activated electrode perforates the uterine wall and makes contact with bowel or other organs. Burns to the cervix, vagina, and vulva have also been reported when monopolar resectoscopic insulation fails or monopolar electrical current is inadvertently diverted.12
In addition, unless one uses tissue-vaporizing electrodes (VIDEO 3) or is equipped
with newer instrumentation that allows tissue to be removed through the operative sheath of the resectoscope, the myoma must be extracted in pieces, often with repeated removal and reinsertion of the resectoscope and grasping instruments, increasing the risk of cervical injury or uterine perforation with each placement.
Another variable that deters hysteroscopic myomectomy is the lack of training at the residency level. The typical ObGyn resident graduating between 2002 and 2007 had performed a median of only 40 to 51 operative hysteroscopic procedures by the time of graduation.14 This statistic suggests that few residency programs provide adequate training for more demanding hysteroscopic surgeries.
Mechanical morcellators facilitate tissue removal
Hysteroscopic morcellators offer advantages over traditional resectoscopy, making hysteroscopic myomectomy of Type 0 and Type I myomas safer and more feasible for gynecologic surgeons. These morcellators allow resection of a myoma using saline, minimizing the hazards of fluid overload. Because they are mechanical devices that do not require electrical energy, the potential for thermal injury is eliminated.
Mechanical morcellators utilize vacuum suction to remove tissue fragments from the uterine cavity, maintaining a tissue-free operative environment and eliminating the need for repeated manual removal. This feature also reduces the risks of perforation, creation of a false passageway, and gas embolus that have been linked to instrument reinsertion and manual removal of tissue fragments.12
Furthermore, mechanical morcellators are easy to use, reducing operative time and fluid deficit.
Removing Type II myomas with a hysteroscopic morcellator may pose a challenge, however, because of significant myometrial penetration. In addition, bleeding is more likely during removal of a Type II myoma than during removal of other types of tumors, necessitating the use of electric current to address it appropriately. Surgeons who are experienced using the morcellator can overcome these challenges by avoiding the myometrial interface and allowing uterine expulsive contractions to push the myoma into the cavity, making it unnecessary to penetrate the myometrium with the instrument. Thorough preoperative evaluation of Type II myomas is recommended, keeping in mind that removal may be safer and more effective using electrosurgical loop resection.



