Expert Commentary
Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean?
It is higher after elective primary cesarean.
Roselyn Jan W. Clemente-Fuentes, MD; Heather Pickett, DO; Misty Carney, MLIS; and Paul Crawford, MD
Roselyn Jan W. Clemente-Fuentes, MD, Heather Pickett, DO, and Paul Crawford, MD, are from the Nellis Family Medicine Residency Program Nellis Air Force Base, Nevada. Misty Carney, MLIS, is at the Stimson Library, Fort Sam Houston, Texas.
The authors report no financial relationships relevant to this article.

Evidence-based answer
Acetaminophen is safe for use in pregnancy but lacks evidence of efficacy (strength of recommendation [SOR]: C, usual practice).
Both physical therapy and water aerobics reduce sick days caused by low-back pain (strength of recommendation [SOR]: B, randomized controlled trial [RCT]). Acupuncture, including auricular acupuncture, also relieves low-back pain and improves function (SOR: B, 2 RCTs).
Osteopathic manipulative therapy (OMT) slightly improves disability (SOR: B, RCT).
Corticosteroid injection at the sacrospinous ligament insertion decreases pain (SOR: B, RCT).
Insufficient evidence of efficacy exists for support garments (SOR: B, systematic review).
No serious maternal or fetal adverse effects have been reported with any of these therapies.
Evidence Summary
Even though clinical research is lacking, acetaminophen is widely used to relieve low-back pain with no documented teratogenic effect (US Food and Drug Administration [FDA] category B). Nonsteroidal anti-inflammatory drugs are classified as FDA category D in the third trimester because of their documented association with oligohydramnios, premature closure of the ductus arteriosus, nephrotoxicity, and periventricular hemorrhage in the fetus.1 Opioids are category C and a poor choice to treat low-back pain in pregnancy.2
Physical therapy and water aerobics relieve pain, reduce sick days
A 2007 Cochrane review of interventions for treating back pain in pregnancy analyzed eight studies with a total of 1305 patients that examined the effects of adding physical therapy and acupuncture to usual care.3 In one RCT, 407 patients with and without pain received five 30-minute individualized physical therapy exercise sessions, two 45-minute group physical therapy classes, or standard care.3,4 Low-back pain decreased with group physical therapy (P <.05; number needed to treat [NNT] = 3.2) and individual therapy (NNT = 2.1). Patients who received individual therapy had a 12% decrease in sick days.
A prospective trial of 258 patients, half of whom did water aerobics and half physical therapy, showed comparable results for the two interventions (NNT = 11.4 for decreased sick days; odds ratio = 0.38, 95% confidence interval [CI], 0.16–0.88).3
Acupuncture reduces pain and analgesic use
A prospective, randomized open study cited in the 2007 Cochrane review divided 72 patients at 24 to 37 weeks’ gestational age into a group that received acupuncture plus standard care and a standard-care–only control group.3,5 Treatment sessions occurred one or two times per week until delivery or recovery. The acupuncture group reported decreased pain (60% vs 14% for controls; P <.01; NNT = 2.2) and improved function (43% vs 9% for controls; P <.001; NNT = 2.9). There was also a difference in analgesic use: 0% for the acupuncture group vs 14% for controls; P <.05; NNT = 7.1.
A 2009 RCT divided 159 patients at 25 to 38 weeks’ gestational age into three groups: auricular acupuncture at specific points for one week, sham auricular acupuncture at nonspecific points for one week, and controls. At the end of Week 1, 80% of the acupuncture group had a clinically significant reduction in pain compared with 56% in the sham acupuncture group and 36% in the control group (P = .001 acupuncture vs sham, NNT = 4.2; P <.0001 acupuncture vs controls, NNT = 2.3).6
Osteopathic manipulative therapy (OMT) decreases disability, but not pain
A 2010 RCT divided 144 third trimester patients into three groups that received usual obstetric care, sham ultrasound therapy plus usual obstetric care, or OMT.7 Pain remained similar among the three groups throughout the study. Using the 24-point Roland-Morris Disability Questionnaire, OMT decreased disability by 0.72 points (95% CI, 0.31–1.14; P <.001) compared with 0.35 points in the usual obstetric-care–only group (95% CI, −0.06 to 0.76; P = .09). Ultrasound had no effect.
Corticosteroid injection reduces pain in a small trial
A small RCT of injection with the corticosteroid triamcinolone at the sacrospinous ligament insertion in 36 women with low-back pain showed significant reduction in pain in 17 of 18 women in the triamcinolone group compared with 9 of 18 women in the control group (P <.01; NNT = 2).8
Evidence lacking on maternity support garments
A poor-quality systematic review of 10 studies (N = 1909) of maternity support garments found insufficient evidence because of the heterogeneity of the trials.9
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists suggests the following measures to prevent and treat low-back pain in pregnancy:10
• wear low-heeled (not flat) shoes with good arch support
• get help when lifting heavy objects
• place one foot on a stool or box when standing for long periods
• place a board between the mattress and box spring if the bed is too soft
• squat down, bend knees, and keep back straight when lifting
• sit in chairs with good back support or use a small pillow to provide support
• sleep on side with pillows between knees for support
• apply heat, cold, or massage to the painful area.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: obg@frontlinemedcom.comThis article was originally published in The Journal of Family Practice (J Fam Pract. 2013;62(5):260, 268).
It is higher after elective primary cesarean.
Planned home birth was associated with a significantly greater likelihood of a 5-minute Apgar score less than 4, compared with hospital birth (0....
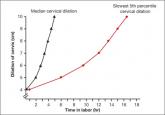
We are in a new era. Our patients, and their labors, have changed on a global scale. To optimally manage labor you need to use these new norms in...
