News
The new year brings refinements to CPT and Medicare codes
New codes, deleted codes, and clarification of just who is a qualified health-care provider are some of the changes that occurred on January 1,...
Melanie Witt, RN, CPC, COBGC, MA, is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
Ms. Witt reports no financial relationships relevant to this article.

Here you’ll find new codes for noninvasive prenatal testing and your peer-to-peer consultation time, as well as information on which ObGyn services are likely to be hardest hit by decreased RVUs in 2014
WATCH for Melanie Witt’s update on ICD-10 conversion ahead of its official release date later this year.
The code set of the 2014 Current Procedural Terminology (CPT), which took effect on January 1, includes several changes that affect all women’s health-care providers, including:
a clarification of who should bill discharge-day management
the addition of interprofessional telephone and Internet consultations
new codes for image-guided fluid drainage
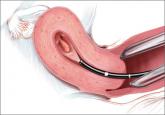
new codes for fibroid embolization and laparoscopic ablation of fibroids.
There are also some new laboratory codes: one that captures the work of the noninvasive prenatal DNA test Harmony, and one to test for Trichomonas vaginalis. Finally, the code for anogenital examinations was revised to reflect current practice.
Medicare also has made some changes you should note, related to the levonorgestrel-releasing intrauterine system Skyla and billing for “incident to” services, and the type of provider who can order a fecal occult blood test. In addition, Medicare changes to some of the practice expense relative value units (RVUs) and geographic payment adjustor values will have an impact on some frequently used ObGyn services.
The changes to the CPT code set took effect January 1. Because of Health Insurance Portability and Accountability Act (HIPAA) requirements, insurers were required to accept new codes on that date.
CPT CODE CHANGES
Discharge-day management coding clarified
Codes 99238 and 99239 should be reported by the admitting provider for all services rendered on the date of discharge as long as the admission and discharge were not on the same date of service. Concurrent hospital services performed by the nonadmitting clinician on the date of discharge should be billed instead as a subsequent inpatient hospital encounter (codes 99231–99233).
Interprofessional phone and Web consultations now reimbursed
Most clinicians at one time or another end up giving advice to another health-care provider about the care of a patient he or she never sees and, up until 2014, there was no way to ask for reimbursement for this additional work. Starting on January 1, however, there were four new codes to allow a consultant clinician to report this work. These services, of a consulting physician who has specific specialty expertise, typically will be provided in complex or urgent situations where a timely face-to-face service with the patient may not be feasible.
The new codes are billed based on total documented cumulative time spent (to account for more than one telephone/Internet contact to complete the consultation request). The codes are for interprofessional telephone/Internet assessment and management service provided by a consultative physician including a verbal and written report to the patient’s treating/requesting physician or other qualified health-care professional, with varying time intervals for medical consultative discussion and review:
99446 5–10 minutes
99447 11–20 minutes
99448 21–30 minutes
99449 31 minutes or more
Like all new codes, these have some very specific requirements:
The billing physician cannot have had a face-to-face encounter with the patient within the past 14 days. If the consultation leads to scheduling a face-to-face appointment or surgery within 14 days, these codes cannot be reported.
If the consultation is to accept transfer of care or arrange for an immediate face-to-face encounter with the consulting physician, these codes should not be billed.
The documentation must include a review of all pertinent medical records, studies, medications, etc., that may be required to render an opinion on how to proceed with care of the patient, and reviewing of any data is not reported separately.
The patient either can be new to the consultant or can be established (with a new or an exacerbated problem).
The majority of the service (more than 50%) must be devoted to the medical consultative verbal/Internet real-time discussion, and not be reported more than once within a 7-day interval.
The request for advice by the qualified health-care professional must be documented in the patient’s medical record, including the reason for the request.
There must be a verbal opinion report and written report from the consultant to the treating physician.
The treating physician who asks for the telephone/Internet advice can report a prolonged services, non–face-to-face code if the time exceeds the typical time of a problem E/M service by 30 minutes to get credit for the discussion with the consultant.
CASE
As an example, Dr. Moody, Mary’s primary care physician, has ordered a computed tomography scan for her due to reports of sharp epigastric pain. A large mass in the area of the right ovary is detected. Dr. Moody phones Dr. Gerard, the patient’s ObGyn of record, for an opinion about additional testing for this mass. Mary was last seen by Dr. Gerard at her well-woman visit 8 months ago; there were no complaints reported or problems detected.
New codes, deleted codes, and clarification of just who is a qualified health-care provider are some of the changes that occurred on January 1,...

With robotic assistance, a surgeon can reduce blood loss, shorten hospitalization, and ease laparoscopic suturing and knot-tying—but myomectomy is...