Clinical Review

2014 Update on abnormal uterine bleeding
Randomized data shed light on AUB associated with fibroids, adenomyosis, and the use of progestins
Amy Garcia, MD, is Director, Center for Women’s Surgery and Garcia Institute for Hysteroscopic Training, Albuquerque, and Clinical Assistant Professor, Department of Obstetrics and Gynecology, University of New Mexico School of Medicine, Albuquerque. Dr. Garcia serves on the OBG Management Board of Editors.
Dr. Garcia reports that she receives grant or research support from Hologic, Inc. She is a consultant to Bayer, Boston Scientific, Channel Medsystems, Ethicon, Hologic, IOGYN, Karl Storz Endoscopy, Minerva Surgical, and Smith & Nephew. She is a speaker for Ethicon.

The reported prevalence of CSD has varied in the literature and appears to depend on the modality of diagnosis and the population studied. For instance, van der Voet and colleagues reported that in random populations of women who had undergone cesarean delivery, the defect was evident in 24% to 69% of women evaluated with transvaginal noncontrast ultrasound; the defect was evident in 56% to 78% of women evaluated with transvaginal contrast sonography. 8
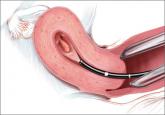
The scar defect also has been identified with magnetic resonance imaging (MRI) and found to be equal in sensitivity to TVUS. 9,10 When identified hysteroscopically, a definitive out-pouching is visualized in the lower uterine segment, where the defect has been termed an “isthmocele.” 6 Hysteroscopically, the defect also is visualized commonly within the cervical canal, indicating that cesarean incisions often are made through cervical tissue at the time of delivery ( FIGURE 3 , VIDEO 1, VIDEO 2 [see below]). Not all women with CSD report bleeding abnormalities, but it appears that the deeper and wider the defect, the more likely a woman is to present with postmenstrual AUB. 7 According to the International Federation of Gynecology and Obstetrics (FIGO) Classification of AUB, CSD-associated postmenstrual bleeding falls into the “iatrogenic” category in the PALM-COIEN pneumonic. 11
Related article: Dr. Garcia discusses the FIGO classification and the PALM-COEIN pneumonic in Update: Minimally invasive gynecology (April 2013)
![]()
![]()
A pair of studies shed light on CSD
Two recent European publications by van der Voet and colleagues addressed CSD and its association with AUB. These studies refer to CSD as the “niche” within the cesarean scar, but for the purpose of this article, I will use the term CSD. The first is a prospective cohort study, in which the authors addressed the definition, diagnosis, and prevalence of a defect within the cesarean scar and reported the incidence of associated AUB. 7 The second publication is a systematic review which includes a critical investigation of minimally invasive therapy for CSD-related AUB. 8 Both publications provide current clinical insight into the evaluation and management of AUB associated with CSD.
Related articles:
• Update on abnormal uterine bleeding Malcolm G. Munro, MD (March 2014)
• Update on Technology Barbara S. Levy, MD (September 2013)
• STOP performing dilation and curettage for the evaluation of abnormal uterine bleeding Amy Garcia, MD (Stop/Start, June 2013)
THE NICHE IN THE SCAR
van der Voet LF, Bij de Vaate AM, Veersema S, Brolmann HAM, Huirne JAF. Long-term complications of caesarean section. The niche in the scar: A prospective cohort study on niche prevalence and its relation to abnormal uterine bleeding. BJOG. 2014;121(2):236–244.
Most studies reporting the prevalence of cesarean delivery–associated postmenstrual bleeding are based on populations of women who were symptomatic with AUB, thus infusing a potential referral bias into these prevalence estimates. In contrast, this study by van der Voet and colleagues utilizes a prospective cohort design, making it the only study to date to enroll a random cohort of patients immediately after having undergone cesarean delivery.

Randomized data shed light on AUB associated with fibroids, adenomyosis, and the use of progestins

How to assess technology and apply new findings to patient care
Understanding of abnormal uterine bleeding has been hampered by inconsistent use of terminology and a lack of classification of its causes, but...
