BED may be difficult to detect because patients may feel ashamed or guilty and are often hesitant to disclose and discuss their symptoms. Furthermore, they are frequently frustrated by the subjective loss of control over their behaviors. Patients with BED often present to medical facilities seeking weight loss solutions rather than to psychiatric clinics.
Screening for eating disorders
Several screening instruments have been developed to help clinicians identify patients who may need further evaluation for possible diagnosis of an eating disorder, including anorexia nervosa, bulimia nervosa, and BED.2 The SCOFF questionnaire is composed of 5 brief clinician-administered questions to screen for eating disorders.2 The 7-item Binge Eating Disorder Screener (BED-7) is a screening instrument specific for BED that examines a patient’s eating patterns and behaviors during the past 3 months.3
In general, suspect BED in patients who have significant weight dissatisfaction, fluctuation in weight, and depressive symptoms. The DSM-5 criteria for binge eating disorder are shown in Table 14.
BED and comorbid psychiatric disorders
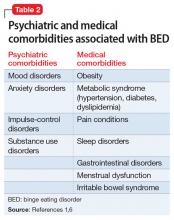
Patients with BED are more likely than the general population to have comorbid psychiatric disorders, including mood and anxiety disorders, attention-deficit/hyperactivity disorder, posttraumatic stress disorder, and substance use disorders. Swanson et al5 found that 83.5% of adolescents who met criteria for BED also met criteria for at least 1 other psychiatric disorder, and 37% endorsed >3 concurrent psychiatric conditions. Once BED is confirmed, it is important to screen for other psychiatric and medical comorbidities that are often present in individuals with BED (Table 21,6).
The rates of diagnosis and treatment of BED remain low. This is likely due to patient factors such as shame and fear of stigma and clinician factors such as lack of awareness, ineffective communication, hesitation to discuss the sensitive topic, or insufficient knowledge about treatment options once BED is diagnosed.
Continue to: TREATMENT Combination therapy