TREATMENT Adding CBT
At an interdisciplinary session several weeks later that includes Ms. P and her parents, the treatment team discusses the revised diagnoses of ASD and MDD, a treatment recommendation for cognitive-behavioral therapy (CBT), and continued use of medication. At this session, Ms. P discloses that she has not been consistent with her medication regimen since her last appointment, which helps explain the increase in her PHQ-9 score from 2 to 14 and GAD-7 score from 10 to 15 as noted at this interdisciplinary session.
The authors’ observations
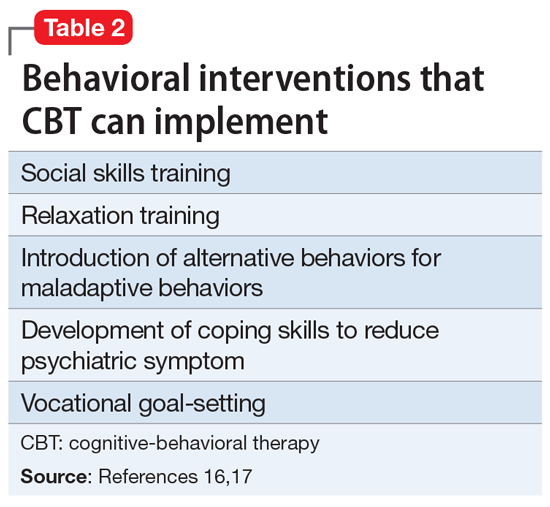
CBT can be helpful in improving medication adherence, developing coping skills, and modifying maladaptive behaviors.16,17Table 216,17 provides examples of behavioral interventions that CBT can implement. The evidence for the benefits of psychosocial interventions for adults with ASD is growing. A small systemic review of psychosocial interventions for adults with ASD found that social cognition training, social skills training, and applied behavior analysis had positive benefits.18
OUTCOME Improvement with psychotherapy
Ms. P and family agree with the team’s recommendations. The aims of Ms. P’s psychotherapy are to maintain medication compliance; implement behavioral modification, vocational rehabilitation, and community engagement; develop social skills; increase functional independence; and develop coping skills for depression and anxiety.
Once her medication is augmented with psychotherapy, Ms. P exhibits a steady decline in PHQ-9 and GAD-7 scores, consistent with an overall reduction of subjective anxiety and depression. In 5 months, her PHQ-9 score decreases from 14 to 2 and her GAD-7 score decreases from 15 to 3. Ms. P is treatment-compliant, more active around the home, and spends more time engaging with friends face-to-face. Overall, the psychotherapy interventions most helpful to her are the development of social skills and coping skills. She reports improved mood, energy levels, concentration, interests, and appetite. Suicidal ideation lessens, and she has not engaged in self-harm since beginning treatment. Worries, tension, and difficulty relaxing also have lessened, though restlessness persists. Excoriation has also decreased significantly, and Ms. P spends less time in the bathroom. Sheenrolls in college courses, plans to start a volleyball team, and is excited about the future.
Bottom Line
The prevalence of schizoid personality disorder (SPD) is low, and its symptoms overlap with those of autism spectrum disorder. Therefore, before diagnosing SPD in an adult patient, it is important to obtain a detailed developmental history and include an interdisciplinary team to assess for autism spectrum disorder.