Patients with fibromyalgia often resist being referred to a psychiatrist because they fear being told their pain and other somatic symptoms are “all in their heads.” Evidence is mounting that they may be literally correct—the symptoms of fibromyalgia appear to have a physiologic connection with the central nervous system. Abnormal CNS activity, including sleep patterns, response to stress, pain processing, and neurotransmitter levels, has been documented in patients with fibromyalgia.
As psychiatrists, we can reassure these patients—and their primary care physicians and rheumatologists—that we are in a position to help because we:
- have expertise in assessing mood and anxiety disorders and in managing antidepressants, the medication physicians most commonly prescribe for fibromyalgia;
- are skilled in the use of the anticonvulsant gabapentin, which is being used in fibromyalgia for its analgesic and sedative effects;
- can offer much-needed support through psychotherapy, as chronic pain and other fibromyalgia-related symptoms create great stress in these patients’ lives.
Antidepressants are showing promise as an effective treatment for pain, fatigue, and depression in patients with fibromyalgia in studies by our group and others. The following information can help you stay current with the newest understandings of this ailment.
Table 1
CRITERIA FOR DIAGNOSING FIBROMYALGIA
| 1. | History of widespread pain |
| Definition Pain in the right and left side of the body, pain above and below the waist, axial skeletal pain (cervical spine or anterior chest or thoracic spine or low back). In this definition, shoulder and buttock pain is considered as pain for each involved side. “Low back” pain is considered lower segment pain. | |
| 2. | Pain in 11 of 18 tender point sites on digital palpation |
| Definition Pain, on digital palpation, must be present in at least 11 of the following 18 tender points: | |
| Occiput Bilateral, at the suboccipital muscle insertion | |
| Low cervical Bilateral, at the anterior aspects of the intertransverse spaces at C5-C7 | |
| Trapezius Bilateral, at the midpoint of the upper border | |
| Supraspinatus Bilateral, at origins, above the scapula spine near the medial border | |
| Second rib Bilateral, at the second costochondral junctions, just lateral to the junctions on upper surfaces | |
| Lateral epicondyle Bilateral, 2 cm distal to the epicondyles | |
| Gluteal Bilateral, in upper outer quadrants of buttocks in anterior fold of muscle | |
| Greater trochanter Bilateral, posterior to the trochanteric prominence | |
| Knee Bilateral, at the medial fat pad proximal to the joint line | |
| Digital palpation should be performed with an approximate force of 4 kg. For a tender point to be considered “positive” the patient must state that the palpation was painful. “Tender” is not to be considered “painful” Source: American College of Rheumatology1 | |
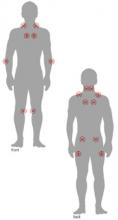
Figure 1 LOCATION OF FIBROMYALGIA TENDER POINTS
To palpate tender point sites, pressure is applied with the thumb pad perpendicularly to each site and the force increased by 1 kg per second until 4 kg of pressure is achieved. Whitening of the thumbnail bed usually occurs when applying the 4-kg force.
Mood disorders in fibromyalgia
A diagnosis of fibromyalgia requires the finding of widespread pain and tenderness at specific anatomic points (Table 1, Figure 1).1 Most patients also report fatigue, sleep disturbance, and morning stiffness (Box 1).2-5 American College of Rheumatology criteria do not require exclusionary tests such as radiographs and blood tests for the diagnosis.
Primary care physicians are increasingly making the diagnosis themselves and referring patients to rheumatologists only when conditions other than fibromyalgia are suspected. The differential diagnosis is broad, and other rheumatic and nonrheumatic disorders have similar symptoms, require different treatment, and affect fibromyalgia management (Table 2).6
Patients with fibromyalgia often report symptoms of major depressive disorder, such as depressed mood, anxiety, fatigue, and insomnia.7 Many psychological studies of such patients have documented increased rates of depressive symptoms.8 Depression and anxiety symptoms are common and frequently severe, even among individuals with fibromyalgia in the general population.9
Patients’ mood and anxiety disorders correlate highly with the number of medically unexplained symptoms and are associated with functional disability.10 The presence of psychological symptoms predicts persistent fibromyalgia symptoms,11 and psychological distress is strongly associated with symptom severity.12
Evidence for a CNS link
CNS mechanisms appear to contribute to the development of clinical findings in fibromyalgia.
Abnormal sleep A qualitative defect in sleep has been identified in patients with fibromyalgia.13 This sleep abnormality consists of inappropriate intrusion of alpha waves (normally seen during wakefulness or REM sleep) into deep sleep (usually characterized by delta waves).13 Some researchers believe alpha-delta sleep intrusion is associated with the chronic musculoskeletal pain and fatigue of fibromyalgia and, in turn, is mediated by an abnormality in central serotonergic neurotransmission.14 This sleep abnormality is not specific to fibromyalgia and can be found in other conditions, however.15 Debate continues regarding the role of sleep dysregulation in the pathophysiology of fibromyalgia.