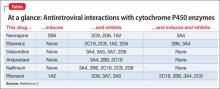
Patients with HIV often receive antiretroviral therapy, which includes non-nucleoside reverse transcriptase inhibitors and protease inhibitors. Opiate, amphetamine, cocaine, and Cannabis abuse are common among this population.1 Many of these substances and antiretroviral medications undergo hepatic metabolism by cytochrome P450 (CYP) isoenzymes, which could lead to adverse events (Table2).
MDMA
The synthetic derivative of the amphetamine 3,4-methylenedioxymethamphetamine (MDMA [“Ecstasy” or “Molly”]) is metabolized by CYP2D6; thus, coadministration of MDMA with ritonavir can result in MDMA toxicity. This can induce a dangerous, potentially fatal serotonin syndrome characterized by tachycardia, arrhythmia, hyperthermia, seizures, myocardial infarction, rhabdomyolysis, renal or liver failure, and death.3
Opiates
Opiates are metabolized by CYP2D6 and, sometimes by CYP3A4. Metabolism of opiates, such as oxycodone, is decreased when these drugs are coadministered with a CYP2D6 inhibitor—potentially leading to toxicity.
Analgesic effect may be augmented when a CYP2D6 inhibitor is started, and decreased when the agent is stopped. Inducers of CYP2D6 or CYP3A4 can lead to decreased analgesia and oxycodone withdrawal.
Efavirenz can cause methadone withdrawal. Methadone inhibition of CYP2D6 and CYP3A4 can increase the serum level of antiretroviral medications, with adverse effects and resulting poor compliance.4
Cannabis
Tetrahydrocannabinol is metabolized by CYP3A4 and CYP2D6. Cannabis and CYP3A4 inhibitor co-utilization can cause toxicity, evidenced by paranoia, hallucinations, delusions, depersonalization, tachycardia, and orthostatic hypotension. Co-exposure of antiretroviral agents in occasional Cannabis users yields only a small change metabolically; however, nonadherence has been reported more frequently in heavy users.5
Education can help
The variability of CYP genotypes makes it important to understand drug metabolism as an aid to improving outcomes among patients with HIV who abuse drugs. Because of the risk for adverse effects, discuss the dangers of substance abuse with patients for whom antiretroviral therapy has been prescribed.
Clinical education should improve compliance and prognosis in patients with HIV. Advise drug users about pharmaceutical effects and risks of co-utilization. This might help some patients limit the use of illicit substances—and will help physicians manage pharmacotherapy with greater safety.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.